Glibenclamide and Metformin Hydrochloride Sustained Release Tablets Daonil M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Metformin Plus Saxagliptin for Type 2 Diabetes
Treatment evaluation Metformin plus saxagliptin for type 2 diabetes André J. Scheen Division of Diabetes, Nutrition and Metabolic Disorders and Division of Clinical Pharmacology, Department of Medicine, CHU Sart Tilman, University of Liège, Liège, Belgium Running title : Saxagliptin plus metformin Word count : Abstract : 148 Main text : 2404 Tables : 4 Figures : 0 Address for correspondence : Pr André J. SCHEEN Department of Medicine CHU Sart Tilman (B35) B-4000 LIEGE 1 BELGIUM Phone : 32-4-3667238 FAX : 32-4-3667068 Page 1 Email : andre.scheen @ chu.ulg.ac.be SUMMARY Metformin is considered as the first-line drug therapy for the management of type 2 diabetes. Dipeptidyl peptidase-4 (DPP-4) inhibitors, by promoting insulin secretion and reducing glucagon secretion in a glucose-dependent manner, offer new opportunities for oral therapy after failure of metformin. Saxagliptin, a DPP-4 inhibitor, and metformin may be administered together, separately or in fixed-dose combination (FDC), either as saxagliptin added to metformin or as initial combination in drug-naive patients. Both compounds exert complementary pharmacodynamic actions leading to better improvement in blood glucose control (fasting plasma glucose, postprandial glucose, HbA1c) than either compound separately. Adding saxagliptin to metformin monthotherapy results in a consistent, sustained and safe reduction in HbA1c levels. Tolerance is excellent without hypoglycemia or weight gain. The combination saxaglitpin plus metformin may be used as first-line or second-line therapy in the management of type 2 diabetes, especially as a valuable alternative to the classical metformin-sulfonylurea combination. Key-words : DPP-4 inhibitor – Fixed-dose combination - Metformin – Saxagliptin - Type 2 diabetes mellitus Page 2 1. -

CD26/DPP-4: Type 2 Diabetes Drug Target with Potential Influence On
cancers Review CD26/DPP-4: Type 2 Diabetes Drug Target with Potential Influence on Cancer Biology Emi Kawakita 1 , Daisuke Koya 2,3 and Keizo Kanasaki 1,3,* 1 Internal Medicine 1, Shimane University Faculty of Medicine, 89-1 Enya-cho, Izumo 693-8501, Japan; [email protected] 2 Department of Diabetology & Endocrinology, Kanazawa Medical University, Uchinada 920-0293, Japan; [email protected] 3 Division of Anticipatory Molecular Food Science and Technology, Medical Research Institute, Kanazawa Medical University, Uchinada 920-0293, Japan * Correspondence: [email protected]; Tel.: +81-853-20-2183 Simple Summary: Dipeptidyl peptidase (DPP)-4 inhibitor is widely used for type 2 diabetes. Al- though DPP-4/CD26 has been recognized as both a suppressor and inducer in tumor biology due to its various functions, how DPP-4 inhibitor affects cancer progression in diabetic patients is still unknown. The aim of this review is to summarize one unfavorable aspect of DPP-4 inhibitor in cancer-bearing diabetic patients. Abstract: DPP-4/CD26, a membrane-bound glycoprotein, is ubiquitously expressed and has diverse biological functions. Because of its enzymatic action, such as the degradation of incretin hormones, DPP-4/CD26 is recognized as the significant therapeutic target for type 2 diabetes (T2DM); DPP- 4 inhibitors have been used as an anti-diabetic agent for a decade. The safety profile of DPP-4 inhibitors for a cardiovascular event in T2DM patients has been widely analyzed; however, a clear association between DPP-4 inhibitors and tumor biology is not yet established. Previous preclinical Citation: Kawakita, E.; Koya, D.; Kanasaki, K. -
Treatment Patterns, Persistence and Adherence Rates in Patients with Type 2 Diabetes Mellitus in Japan: a Claims- Based Cohort Study
Open access Research BMJ Open: first published as 10.1136/bmjopen-2018-025806 on 1 March 2019. Downloaded from Treatment patterns, persistence and adherence rates in patients with type 2 diabetes mellitus in Japan: a claims- based cohort study Rimei Nishimura,1 Haruka Kato,2 Koichi Kisanuki,2 Akinori Oh,2 Shinzo Hiroi,2 Yoshie Onishi,3 Florent Guelfucci,4 Yukio Shimasaki2 To cite: Nishimura R, Kato H, ABSTRACT Strengths and limitations of this study Kisanuki K, et al. Treatment Objective To determine real-world trends in antidiabetic patterns, persistence and drug use, and persistence and adherence, in Japanese ► This retrospective evaluation of administrative adherence rates in patients patients with type 2 diabetes mellitus (T2DM). with type 2 diabetes mellitus claims data (2011–2015) using the Japan Medical Design Retrospective evaluation of administrative claims in Japan: a claims-based Data Center (JMDC) and Medical Data Vision (MDV) data (2011–2015) using the Japan Medical Data Center cohort study. BMJ Open databases was conducted to determine real-world (JMDC) and Medical Data Vision (MDV) databases. 2019;9:e025806. doi:10.1136/ trends in antidiabetic drug use, and persistence and Setting Analysis of two administrative claims databases bmjopen-2018-025806 adherence, in Japanese patients with type 2 dia- for Japanese patients with T2DM. betes mellitus (T2DM); 40 908 and 90 421 patients ► Prepublication history and Participants Adults (aged ≥18 years) with an International additional material for this were included from the JMDC and MDV databases, Classification of Diseases, 10th Revision code of T2DM and paper are available online. To respectively. at least one antidiabetic drug prescription. -

Komboglyze, INN-Saxagliptin, Metformin
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT Komboglyze 2.5 mg/850 mg film-coated tablets Komboglyze 2.5 mg/1,000 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Komboglyze 2.5 mg/850 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 850 mg of metformin hydrochloride. Komboglyze 2.5 mg/1,000 mg film-coated tablets Each tablet contains 2.5 mg of saxagliptin (as hydrochloride) and 1,000 mg of metformin hydrochloride. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). Komboglyze 2.5 mg/850 mg film-coated tablets Light brown to brown, biconvex, round, film-coated tablets, with “2.5/850” printed on one side and “4246” printed on the other side, in blue ink. Komboglyze 2.5 mg/1,000 mg film-coated tablets Pale yellow to light yellow, biconvex, oval shaped, film-coated tablets, with “2.5/1000” printed on one side and “4247” printed on the other side, in blue ink. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Komboglyze is indicated in adults with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: in patients inadequately controlled on their maximally tolerated dose of metformin alone in combination with other medicinal products for the treatment of diabetes, including insulin, in patients inadequately controlled with metformin and these medicinal products (see sections 4.4, 4.5 and 5.1 for available data on different combinations) in patients already being treated with the combination of saxagliptin and metformin as separate tablets. -

Effect of Oral Hypoglycaemic Agents on Glucose Tolerance in Pancreatic Diabetes
Gut: first published as 10.1136/gut.13.4.285 on 1 April 1972. Downloaded from Gut, 1972, 13, 285-288 Effect of oral hypoglycaemic agents on glucose tolerance in pancreatic diabetes B. I. JOFFE, W. P. U. JACKSON, S. BANK, AND A. I. VINIK From the Department of Medicine, Witwatersrand University Medical School, Johannesburg, the Gastro- intestinal and Endocrine Research Units of Cape Town University Medical School, and the Chemical Pathology Department of Natal University, South Africa SUMMARY The short-term therapeutic effect of oral hypoglycaemic agents has been assessed in 12 patients with symptomatic diabetes secondary to chronic pancreatitis (pancreatic diabetes). In six patients who had moderate to severe carbohydrate intolerance, associated with severe insulino- paenia during arginine infusion, the potent sulphonylurea chlorpropamide produced no change in the fasting blood glucose level after two weeks of treatment. This contrasted with the significant reduction produced in a matched group of maturity-onset primary diabetics. The six patients with milder diabetes, and a greater (although still subnormal) insulin secretory capacity, showed an improvement in oral glucose tolerance during the first hour following glucose administration while on chlorpropamide. When the biguanide phenformin was substituted for chlorpropamide in five of these patients, a statistically insignificant improvement in glucose tolerance was observed during treatment. Applications of these findings to the practical management of pancreatic diabetes are briefly http://gut.bmj.com/ considered. Chronic pancreatitis is frequently complicated by and two women, ranging from 30 to 67 years of age. diabetes (pancreatic diabetes). Recent studies The diagnosis of pancreatitis was confirmed on the utilizing immunoassay procedures (Joffe, Bank, basis of a gross abnormality in at least two aspects of Jackson, Keller, O'Reilly, and Vinik, 1968; Anderson the pancreatic function test, namely, a low volume of on September 24, 2021 by guest. -

AVANDIA (Rosiglitazone Maleate Tablets), for Oral Use Ischemic Cardiovascular (CV) Events Relative to Placebo, Not Confirmed in Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------- WARNINGS AND PRECAUTIONS ----------------------- These highlights do not include all the information needed to use • Fluid retention, which may exacerbate or lead to heart failure, may occur. AVANDIA safely and effectively. See full prescribing information for Combination use with insulin and use in congestive heart failure NYHA AVANDIA. Class I and II may increase risk of other cardiovascular effects. (5.1) • Meta-analysis of 52 mostly short-term trials suggested a potential risk of AVANDIA (rosiglitazone maleate tablets), for oral use ischemic cardiovascular (CV) events relative to placebo, not confirmed in Initial U.S. Approval: 1999 a long-term CV outcome trial versus metformin or sulfonylurea. (5.2) • Dose-related edema (5.3) and weight gain (5.4) may occur. WARNING: CONGESTIVE HEART FAILURE • Measure liver enzymes prior to initiation and periodically thereafter. Do See full prescribing information for complete boxed warning. not initiate therapy in patients with increased baseline liver enzyme levels ● Thiazolidinediones, including rosiglitazone, cause or exacerbate (ALT >2.5X upper limit of normal). Discontinue therapy if ALT levels congestive heart failure in some patients (5.1). After initiation of remain >3X the upper limit of normal or if jaundice is observed. (5.5) AVANDIA, and after dose increases, observe patients carefully for signs • Macular edema has been reported. (5.6) and symptoms of heart failure (including excessive, rapid weight gain; • Increased incidence of bone fracture was observed in long-term trials. dyspnea; and/or edema). If these signs and symptoms develop, the heart (5.7) failure should be managed according to current standards of care. -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal. -

MRI Evidence That Glibenclamide Reduces Acute Lesion Expansion in a Rat Model of Spinal Cord Injury
Spinal Cord (2013) 51, 823–827 OPEN & 2013 International Spinal Cord Society All rights reserved 1362-4393/13 www.nature.com/sc ORIGINAL ARTICLE MRI evidence that glibenclamide reduces acute lesion expansion in a rat model of spinal cord injury JM Simard1,2,3, PG Popovich4, O Tsymbalyuk1, J Caridi1, RP Gullapalli5, MJ Kilbourne6 and V Gerzanich1 Study design: Experimental, controlled, animal study. Objectives: To use non-invasive magnetic resonance imaging (MRI) to corroborate invasive studies showing progressive expansion of a hemorrhagic lesion during the early hours after spinal cord trauma and to assess the effect of glibenclamide, which blocks Sur1-Trpm4 channels implicated in post-traumatic capillary fragmentation, on lesion expansion. Setting: Baltimore. Methods: Adult female Long–Evans rats underwent unilateral impact trauma to the spinal cord at C7, which produced ipsilateral but not contralateral primary hemorrhage. In series 1 (six control rats and six administered glibenclamide), hemorrhagic lesion expansion was characterized using MRI at 1 and 24 h after trauma. In series 2, hemorrhagic lesion size was characterized on coronal tissue sections at 15 min (eight rats) and at 24 h after trauma (eight control rats and eight administered glibenclamide). Results: MRI (T2 hypodensity) showed that lesions expanded 2.3±0.33-fold (Po0.001) during the first 24 h in control rats, but only 1.2±0.07-fold (P40.05) in glibenclamide-treated rats. Measuring the areas of hemorrhagic contusion on tissue sections at the epicenter showed that lesions expanded 2.2±0.12-fold (Po0.001) during the first 24 h in control rats, but only 1.1±0.05-fold (P40.05) in glibenclamide-treated rats. -
Taking Metformin for Gestational Diabetes This Information Sheet Will Help You Understand More About Taking Metformin for Gestational Diabetes
Taking metformin for gestational diabetes This information sheet will help you understand more about taking metformin for gestational diabetes. This information sheet is not a substitute for talking with your midwife, doctor, nurse or pharmacist. Gestational diabetes Risks for your baby: Gestational diabetes means you have too much • may grow larger than normal (this increases the glucose (a type of sugar) in your blood when you risk of injury during birth) are pregnant. Insulin controls the amount of • born too early (premature) glucose in your blood. Sometimes you don’t make • low blood glucose after birth enough insulin or it doesn’t work as well when you are pregnant. • may need treatment in hospital • jaundice (yellow skin) that needs treatment Gestational diabetes is common. Up to eight pregnant women in every 100 get gestational • breathing problems. diabetes. Taking metformin helps reduce these risks. It can be hard to tell if you have gestational You can see how many women and babies are diabetes. Some women find that they: affected and how treatment helps in the picture • lack energy on the next page. • feel thirsty a lot • go to the toilet a lot Metformin is safe to take for • get lots of infections. gestational diabetes Metformin has been tested in clinical studies and Some women have no symptoms. This is why all is safe to take for gestational diabetes. pregnant women are tested for diabetes so they Metformin helps keep both your weight gain and can get treatment. blood pressure down. Metformin The main side effect is stomach upsets such as Metformin is a medicine that has been used feeling sick and diarrhoea. -
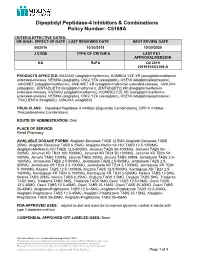
Dipeptidyl Peptidase-4 Inhibitors and Combinations
Dipeptidyl Peptidase-4 Inhibitors & Combinations Policy Number: C5169A CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE 06/2016 10/30/2019 10/30/2020 J CODE TYPE OF CRITERIA LAST P&T APPROVAL/VERSION NA RxPA Q4 2019 20191030C5169-A PRODUCTS AFFECTED: KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone), JANUMET (sitagliptin/metformin), JANUMET XR (sitagliptin/metformin extended-release), JANUVIA (sitagliptin), JENTADUETO (linagliptin/metformin), JENTADUETO XR (linagliptin/metformin extended-release), KAZANO (alogliptin/metformin), KOMBIGLYZE XR (saxagliptin/metformin extended-release), NESINA (alogliptin), ONGLYZA (saxagliptin), OSENI (alogliptin/pioglitazone) TRADJENTA (linagliptin), JANUVIA (sitagliptin) DRUG CLASS: Dipeptidyl Peptidase-4 Inhibitor-(Biguanide Combinations), DPP-4 Inhibitor- Thiazolidinedione Combinations ROUTE OF ADMINISTRATION: Oral PLACE OF SERVICE: Retail Pharmacy AVAILABLE DOSAGE FORMS: Alogliptin Benzoate TABS 12.5MG,Alogliptin Benzoate TABS 25MG, Alogliptin Benzoate TABS 6.25MG, Alogliptin-Metformin HCl TABS 12.5-1000MG Alogliptin-Metformin HCl TABS 12.5-500MG, Janumet TABS 50-1000MG, Janumet TABS 50- 500MG, Janumet XR TB24 100-1000MG, Janumet XR TB24 50-1000MG, Janumet XR TB24 50- 500MG, Januvia TABS 100MG, Januvia TABS 25MG, Januvia TABS 50MG, Jentadueto TABS 2.5- 1000MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5-500MG, Jentadueto TABS 2.5- 850MG, Jentadueto -

Polyhexamethylene Biguanide Hydrochloride) As Used in Cosmetics
Safety Assessment of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride) as Used in Cosmetics Status: Tentative Report for Public Comment Release Date: September 26, 2017 Panel Date: December 4-5, 2017 All interested persons are provided 60 days from the above date to comment on this safety assessment and to identify additional published data that should be included or provide unpublished data which can be made public and included. Information may be submitted without identifying the source or the trade name of the cosmetic product containing the ingredient. All unpublished data submitted to CIR will be discussed in open meetings, will be available at the CIR office for review by any interested party and may be cited in a peer-reviewed scientific journal. Please submit data, comments, or requests to the CIR Executive Director, Dr. Bart Heldreth. The 2017 Cosmetic Ingredient Review Expert Panel members are: Chair, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D.; Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Executive Director is Bart Heldreth, Ph.D. This report was prepared by Wilbur Johnson, Jr., M.S., Senior Scientific Analyst and Ivan Boyer, Ph.D., former Senior Toxicologist. © Cosmetic Ingredient Review 1620 L STREET, NW, SUITE 1200 ◊ WASHINGTON, DC 20036-4702 ◊ PH 202.331.0651 ◊ FAX 202.331.0088 ◊ [email protected] ABSTRACT: The Cosmetic Ingredient Review (CIR) Expert Panel (Panel) reviewed the safety of Polyaminopropyl Biguanide (polyhexamethylene biguanide hydrochloride), which functions as a preservative in cosmetic products. -

A Review on Evolution in Triglyceride Determination
Available online at www.derpharmachemica.com ISSN 0975-413X Der Pharma Chemica, 2018, 10(5): 84-88 CODEN (USA): PCHHAX (http://www.derpharmachemica.com/archive.html) Sodium-glucose co-transporter 2 (SGLT2) Inhibitors: New Target for Type 2 Diabetes Mellitus (T2DM) Review Swapna Vadlamani* Asst. proffesor, NIPER, Hyderabad, Andhra Pradesh, India ABSTRACT Introduction: Knocking out type2 diabetes by new insulin independent renal glucose transporters as targets, reducing the side effects related to high rise in glucose levels is a more efficient way to manage diabetes. Sodium-glucose co-transporter 2 (SGLT2) inhibitors block reabsorption of glucose back into the blood and stimulate secretion in urine in a way controlling blood glucose levels. Areas discussed: We emphasize in this review an overview of type 2 diabetes. New insulin independent targets, SGLT family inhibitors and their mechanism of action are briefly discussed. Molecular modeling studies carried out for new analogues of SGLT2 were indicated and also about current marketed SGLT drugs their safety issues are briefly outlined. Conclusion: SGLT2 inhibitors are very promising drugs for near future, where insulin sensitization is a problem. A combination of drugs related to insulin dependent pathway and also independent pathway like SGLT2/SGLT1 drugs will be more effective in glycemic control with lesser side effects. Keywords: Type II Diabetes, SGLT2 inhibitors INTRODUCTION Present scenario of food habits and absolutely very less physical activity is becoming the major cause for obesity finally leading to diabetes. Diabetes is said to be a rich man disease and mostly occurs at the later age of 40, but now one in every 5 persons at early age diagnosed turned to be diabetic mainly because of lifestyle changes.