Small Bowel Bleeding and Capsule Endoscopy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Provocative Testing and Localization in Video Capsule Endoscopy
1 2 The Role of Provocative 3 4 Testing and Localization of 5 6 the Video Capsule Endoscope in 7 the Management of Small 8 9 Intestinal Bleeding Q4 10 11 a, b 12 Daniel L. Raines, MD *, Douglas G. Adler, MD Q5 Q6 Q7 13 Q1 Q2 14 15 KEYWORDS 16 Small intestinal bleeding Provocative angiography Provocative endoscopy 17 Video capsule endoscopy Device-assisted enteroscopy 18 19 20 KEY POINTS 21 Cases of small intestinal bleeding (SIB) are commonly encountered in clinical practice 22 despite advancements in medical technology that allow consistent visualization of the 23 entire gastrointestinal tract. 24 The use of antithrombotic agents to provoke bleeding has been found to be revealing in 25 cases of SIB when used in combination with angiography as well as endoscopy. 26 The performance of endoscopic procedures, including video capsule endoscopy (VCE) 27 and device-assisted enteroscopy (DAE) on active antiplatelet and/or anticoagulant ther- 28 apy is considered low risk and may improve diagnostic yield. 29 The use of VCE for gastrointestinal bleeding in the inpatient setting has been found to 30 improve diagnostic yield and decrease hospital stay. 31 Because DAE is required for therapeutic intervention in patients with small bowel 32 bleeding, access to this technology is essential for effective management in many cases. 33 34 35 Video content accompanies this article at http://www.giendo.theclinics.com/. 36 37 Q8 38 OBSCURE GASTROINTESTINAL BLEEDING Definitions 39 40 Small intestinal bleeding (SIB) has been described as bleeding that is undefined in 41 cause despite evaluation by standard upper endoscopy, colonoscopy, and small Q9 42 bowel follow-through (SBFT). -

081999 Disseminated Intravascular Coagulation
The New England Journal of Medicine Current Concepts Systemic activation+ of coagulation DISSEMINATED INTRAVASCULAR COAGULATION Intravascular+ Depletion of platelets+ deposition of fibrin and coagulation factors MARCEL LEVI, M.D., AND HUGO TEN CATE, M.D. Thrombosis of small+ Bleeding and midsize vessels+ ISSEMINATED intravascular coagulation is and organ failure characterized by the widespread activation Dof coagulation, which results in the intravas- Figure 1. The Mechanism of Disseminated Intravascular Coag- cular formation of fibrin and ultimately thrombotic ulation. occlusion of small and midsize vessels.1-3 Intravascu- Systemic activation of coagulation leads to widespread intra- lar coagulation can also compromise the blood sup- vascular deposition of fibrin and depletion of platelets and co- agulation factors. As a result, thrombosis of small and midsize ply to organs and, in conjunction with hemodynam- vessels may occur, contributing to organ failure, and there may ic and metabolic derangements, may contribute to be severe bleeding. the failure of multiple organs. At the same time, the use and subsequent depletion of platelets and coag- ulation proteins resulting from the ongoing coagu- lation may induce severe bleeding (Fig. 1). Bleeding may be the presenting symptom in a patient with disseminated intravascular coagulation, a factor that can complicate decisions about treatment. TABLE 1. COMMON CLINICAL CONDITIONS ASSOCIATED WITH DISSEMINATED ASSOCIATED CLINICAL CONDITIONS INTRAVASCULAR COAGULATION. AND INCIDENCE Sepsis Infectious Disease Trauma Serious tissue injury Disseminated intravascular coagulation is an ac- Head injury Fat embolism quired disorder that occurs in a wide variety of clin- Cancer ical conditions, the most important of which are listed Myeloproliferative diseases in Table 1. -

What Everyone Should Know to Stop Bleeding After an Injury
What Everyone Should Know to Stop Bleeding After an Injury THE HARTFORD CONSENSUS The Joint Committee to Increase Survival from Active Shooter and Intentional Mass Casualty Events was convened by the American College of Surgeons in response to the growing number and severity of these events. The committee met in Hartford Connecticut and has produced a number of documents with rec- ommendations. The documents represent the consensus opinion of a multi-dis- ciplinary committee involving medical groups, the military, the National Security Council, Homeland Security, the FBI, law enforcement, fire rescue, and EMS. These recommendations have become known as the Hartford Consensus. The overarching principle of the Hartford Consensus is that no one should die from uncontrolled bleeding. The Hartford Consensus recommends that all citizens learn to stop bleeding. Further information about the Hartford Consensus and bleeding control can be found on the website: Bleedingcontrol.org 2 SAVE A LIFE: What Everyone Should Know to Stop Bleeding After an Injury Authors: Peter T. Pons, MD, FACEP Lenworth Jacobs, MD, MPH, FACS Acknowledgements: The authors acknowledge the contributions of Michael Cohen and James “Brooks” Hart, CMI to the design of this manual. Some images adapted from Adam Wehrle, EMT-P and NAEMT. © 2017 American College of Surgeons CONTENTS SECTION 1 3 ■ Introduction ■ Primary Principles of Trauma Care Response ■ The ABCs of Bleeding SECTION 2 5 ■ Ensure Your Own Safety SECTION 3 6 ■ A – Alert – call 9-1-1 SECTION 4 7 ■ B – Bleeding – find the bleeding injury SECTION 5 9 ■ C – Compress – apply pressure to stop the bleeding by: ■ Covering the wound with a clean cloth and applying pressure by pushing directly on it with both hands, OR ■Using a tourniquet, OR ■ Packing (stuff) the wound with gauze or a clean cloth and then applying pressure with both hands SECTION 6 13 ■ Summary 2 SECTION 1: INTRODUCTION Welcome to the Stop the Bleed: Bleeding Control for the Injured information booklet. -

ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding
nature publishing group PRACTICE GUIDELINES 1265 CME ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding L a u r e n B . G e r s o n , M D , M S c , F A C G1 , J e ff L. Fidler , MD 2 , D a v i d R . C a v e , M D , P h D , F A C G 3 a n d J o n a t h a n A . L e i g h t o n , M D , F A C G 4 Bleeding from the small intestine remains a relatively uncommon event, accounting for ~5–10% of all patients presenting with gastrointestinal (GI) bleeding. Given advances in small bowel imaging with video capsule endoscopy (VCE), deep enteroscopy, and radiographic imaging, the cause of bleeding in the small bowel can now be identifi ed in most patients. The term small bowel bleeding is therefore proposed as a replacement for the previous classifi cation of obscure GI bleeding (OGIB). We recommend that the term OGIB should be reserved for patients in whom a source of bleeding cannot be identifi ed anywhere in the GI tract. A source of small bowel bleeding should be considered in patients with GI bleeding after performance of a normal upper and lower endoscopic examination. Second-look examinations using upper endoscopy, push enteroscopy, and/or colonoscopy can be performed if indicated before small bowel evaluation. VCE should be considered a fi rst-line procedure for small bowel investigation. Any method of deep enteroscopy can be used when endoscopic evaluation and therapy are required. -

Obscure Gastrointestinal Bleeding in Cirrhosis: Work-Up and Management
Current Hepatology Reports (2019) 18:81–86 https://doi.org/10.1007/s11901-019-00452-6 MANAGEMENT OF CIRRHOTIC PATIENT (A CARDENAS AND P TANDON, SECTION EDITORS) Obscure Gastrointestinal Bleeding in Cirrhosis: Work-up and Management Sergio Zepeda-Gómez1 & Brendan Halloran1 Published online: 12 February 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review Obscure gastrointestinal bleeding (OGIB) in patients with cirrhosis can be a diagnostic and therapeutic challenge. Recent advances in the approach and management of this group of patients can help to identify the source of bleeding. While the work-up of patients with cirrhosis and OGIB is the same as with patients without cirrhosis, clinicians must be aware that there are conditions exclusive for patients with portal hypertension that can potentially cause OGIB. Recent Findings New endoscopic and imaging techniques are capable to identify sources of OGIB. Balloon-assisted enteroscopy (BAE) allows direct examination of the small-bowel mucosa and deliver specific endoscopic therapy. Conditions such as ectopic varices and portal hypertensive enteropathy are better characterized with the improvement in visualization by these techniques. New algorithms in the approach and management of these patients have been proposed. Summary There are new strategies for the approach and management of patients with cirrhosis and OGIB due to new develop- ments in endoscopic techniques for direct visualization of the small bowel along with the capability of endoscopic treatment for different types of lesions. Patients with cirrhosis may present with OGIB secondary to conditions associated with portal hypertension. Keywords Obscure gastrointestinal bleeding . Cirrhosis . Portal hypertension . -
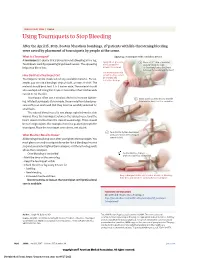
Using Tourniquets to Stop Bleeding
JAMA PATIENT PAGE | Trauma Using Tourniquets to Stop Bleeding After the April 15, 2013, Boston Marathon bombings, 27 patients with life-threatening bleeding were saved by placement of tourniquets by people at the scene. What Is a Tourniquet? Applying a tourniquet with a windlass device A tourniquet is a device that is placed around a bleeding arm or leg. Apply direct pressure 1 Place a 2-3” strip of material Tourniquets work by squeezing large blood vessels. The squeezing to the wound for about 2” from the edge helps stop blood loss. at least 15 minutes. of the wound over a long bone between the wound and the heart. Use a tourniquet only How Do I Put a Tourniquet On? when bleeding cannot be stopped and Tourniquets can be made out of any available material. For ex- is life threatening. ample, you can use a bandage, strip of cloth, or even a t-shirt. The material should be at least 2 to 3 inches wide. The material should also overlap itself. Using thin straps or material less than 2 inches wide can rip or cut the skin. Tourniquets often use a windlass device to increase tighten- 2 Insert a stick or other strong, straight ing. Inflated tourniquets (for example, those made from blood pres- item into the knot to act as a windlass. sure cuffs) can work well. But they must be carefully watched for small leaks. The injured blood vessel is not always right below the skin wound. Place the tourniquet between the injured vessel and the heart, about 2 inches from the closest wound edge. -

ER Guide to Bleeding Disorders
Bleeding disorders ER guide to bleeding disorders 1 Table of contents 4 General Guidelines 4–5 national Hemophilia Foundation guidelines 5–10 Treatment options 10 HemopHilia a Name:__________________________________________________________________________________________________ 10–11 national Hemophilia Foundation guidelines Address:________________________________________________________________________________________________ 12 dosage chart Phone:__________________________________________________________________________________________________ 14–15 Treatment products 16 HemopHilia B In case of emergency, contact: ______________________________________________________________________________ 16 national Hemophilia Foundation guidelines Relation to patient:________________________________________________________________________________________ 17 dosage chart 18 Treatment products 19 HemopHilia a or B with inHiBiTors Diagnosis: Hemophilia A: Mild Moderate Severe 20 national Hemophilia Foundation guidelines Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 21 Treatment products Hemophilia B: Mild Moderate Severe 22–23 Von willeBrand disease Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 23–24 national Hemophilia Foundation guidelines von Willebrand disease: Type 1 Type 2 Type 3 Platelet type 25 Treatment products 27 Bibliography Preferred product:_________________________________________________________________________________________ Dose for life-threatening -

Efficacy of Colonoscopy, Colon Capsule and Fecal Immunological Test For
Efficacy of colonoscopy, colon capsule and fecal immunological test for colorectal cancer screening, in first degree relatives of patients with colorectal neoplasia: a prospective randomized study - FAMCAP Study Version n°6 - Date: 2017-07-11 Sponsor: Hospices Civils de Lyon BP 2251 3 quai des Célestins 69229 LYON Cedex 02 - France Coordinator: Pr Jean-Christophe SAURIN Hepatogastroenterology - Pav. L Edouard Herriot Hospital - Hospices Civils de Lyon 5 Place d’Arsonval 69437 LYON Cedex 3 - FRANCE Phone: +33 (0)4 72 11 75 72; Fax: +33 (0)4 72 11 01 47 E-mail: [email protected] Methodologist: Pr Anne-Marie SCHOTT Pôle IMER - Hospices Civils de Lyon 162 avenue Lacassagne 69424 LYON Cedex 3 - FRANCE E-mail: [email protected] Sponsor code: 69HCL16_0091 ID-RCB number: 2016-A01097-44 Clinicaltrials.gov registration number: NCT02738359 Date of Ethics Committee (CPP Sud-Est III) approval: 2016-10-18 Abstract: Fecal immunological test (FIT) is the reference screening method in average risk patient. FIT is proposed every 2 years to all asymptomatic subjects with average risk aged from 50 to 74 years in France. Optical colonoscopy (OC) is the gold standard examination for patients at increased risk of colorectal cancer, like those with a first degree relative with colorectal cancer (relative risk between 2 and 4 times that of the general population). Colonoscopy should be performed in this high risk group before 50 years or 5 to 10 years before the earliest case of colorectal cancer. Optical colonoscopy has important limitations: complications (perforation, bleeding), need to use general anesthesia (in France 95% of colonoscopy are performed under general anesthesia), and low acceptability for screening even in high risk persons (40% in the best cases). -
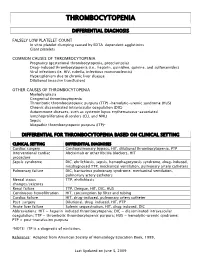
Thrombocytopenia.Pdf
THROMBOCYTOPENIA DIFFERENTIAL DIAGNOSIS FALSELY LOW PLATELET COUNT In vitro platelet clumping caused by EDTA-dependent agglutinins Giant platelets COMMON CAUSES OF THROMBOCYTOPENIA Pregnancy (gestational thrombocytopenia, preeclampsia) Drug-induced thrombocytopenia (i.e., heparin, quinidine, quinine, and sulfonamides) Viral infections (ie. HIV, rubella, infectious mononucleosis) Hypersplenism due to chronic liver disease Dilutional (massive transfusion) OTHER CAUSES OF THROMBOCYTOPENIA Myelodysplasia Congenital thrombocytopenia Thrombotic thrombocytopenic purpura (TTP) -hemolytic-uremic syndrome (HUS) Chronic disseminated intravascular coagulation (DIC) Autoimmune diseases, such as systemic lupus erythematosus-associated lymphoproliferative disorders (CLL and NHL) Sepsis Idiopathic thrombocytopenic purpura (ITP)* DIFFERENTIAL FOR THROMBOCYTOPENIA BASED ON CLINICAL SETTING CLINICAL SETTING DIFFERENTIAL DIAGNOSES Cardiac surgery Cardiopulmonary bypass, HIT, dilutional thrombocytopenia, PTP Interventional cardiac Abciximab or other IIb/IIIa blockers, HIT procedure Sepsis syndrome DIC, ehrlichiosis, sepsis, hemophagocytosis syndrome, drug-induced, misdiagnosed TTP, mechanical ventilation, pulmonary artery catheters Pulmonary failure DIC, hantavirus pulmonary syndrome, mechanical ventilation, pulmonary artery catheters Mental status TTP, ehrlichiosis changes/seizures Renal failure TTP, Dengue, HIT, DIC, HUS Continuous hemofiltration HIT, consumption by filter and tubing Cardiac failure HIT, drug-induced, pulmonary artery catheter Post-surgery -

Capsule Endoscopy
UnitedHealthcare® Medicare Advantage Policy Guideline Capsule Endoscopy Guideline Number: MPG036.06 Approval Date: March 10, 2021 Terms and Conditions Table of Contents Page Related Medicare Advantage Policy Guideline Policy Summary ............................................................................. 1 • Category III CPT Codes Applicable Codes .......................................................................... 3 References ..................................................................................... 9 Related Medicare Advantage Coverage Summary Guideline History/Revision Information ..................................... 10 • Gastroesophageal and Gastrointestinal (GI) Services Purpose ........................................................................................ 12 and Procedures Terms and Conditions ................................................................. 13 Policy Summary See Purpose Overview Wireless capsule endoscopy (WCE) requires that the patient ingest a small capsule containing a disposable light source, miniature color video camera, battery, antenna and a data transmitter. The self-contained capsule is made of specially sealed biocompatible material that is resistant to the digestive fluids throughout the gastrointestinal (GI) tract. Following ingestion of the capsule, natural contraction and relaxation of the GI tract propels the capsule forward. The camera contained in the capsule records images as it travels through the digestive system. During the entire procedure, the patient wears -

Clinical Impact of Small Bowel Capsule Endoscopy in Obscure Gastrointestinal Bleeding
medicina Article Clinical Impact of Small Bowel Capsule Endoscopy in Obscure Gastrointestinal Bleeding Ana-Maria Singeap 1,2 , Camelia Cojocariu 1,2,*, Irina Girleanu 1,2, Laura Huiban 1,2, Catalin Sfarti 1,2, Tudor Cuciureanu 1,2, Stefan Chiriac 1,2 , Carol Stanciu 2 and Anca Trifan 1,2 1 Department of Gastroenterology, Faculty of Medicine, “Grigore T. Popa” University of Medicine and Pharmacy, 700115 Iasi, Romania; [email protected] (A.-M.S.); [email protected] (I.G.); [email protected] (L.H.); [email protected] (C.S.); [email protected] (T.C.); [email protected] (S.C.); [email protected] (A.T.) 2 Institute of Gastroenterology and Hepatology, “St. Spiridon” Emergency Hospital, 700111 Iasi, Romania; [email protected] * Correspondence: [email protected]; Tel.: +40-752223968 Received: 31 August 2020; Accepted: 16 October 2020; Published: 19 October 2020 Abstract: Background and objectives: The most frequent indications for small bowel capsule endoscopy (SBCE) are obscure gastrointestinal bleeding (OGIB) and iron deficiency anemia (IDA). The aim of this study was to evaluate the diagnostic yield (DY) of SBCE in overt and occult OGIB, as well as its impact on the clinical outcome. Materials and Methods: This study retrospectively included all cases of OGIB investigated by SBCE in a tertiary care referral center, between 1st January 2016 and 31st December 2018. OGIB was defined by overt or occult gastrointestinal bleeding, with negative upper and lower endoscopy. Occult gastrointestinal bleeding was either proved by a fecal test or presumptively incriminated as a cause for IDA. DY was defined as the detection rate for what were thought to be clinically significant findings. -

Capsule Endoscopy
CLINICAL MEDICAL POLICY Policy Name: Capsule Endoscopy Policy Number: MP-038-MD-PA Responsible Department(s): Medical Management Provider Notice Date: 02/17/2020 Issue Date: 02/17/2020 Effective Date: 03/16/2020 Annual Approval Date: 12/2020 Revision Date: 12/18/2019 Products: Gateway Health℠ Medicaid Application: All participating hospitals and providers Page Number(s): 1 of 12 DISCLAIMER Gateway Health℠ (Gateway) medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions. POLICY STATEMENT Gateway Health℠ provides coverage under the medical-surgical benefits of the Company’s Medicaid products for medically necessary capsule endoscopy procedures. This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records. (Current applicable Pennsylvania HealthChoices Agreement Section V. Program Requirements, B. Prior Authorization of Services, 1. General Prior Authorization Requirements.) Policy No. MP-038-MD-PA Page 1 of 12 DEFINITIONS Prior Authorization Review Panel (PARP) – A panel of representatives from within the Pennsylvania Department of Human Services who have been assigned organizational responsibility for the review, approval and denial of all PH-MCO Prior Authorization policies and procedures. Gastric Emptying Scintigraphy – A diagnostic test where the individual ingests a radionuclide-labeled standard meal, and then images are taken at 0, 1, 2, and 4 hours postprandial in order to measure how much of the meal has passed beyond the stomach.