A Functional Candidate Screen for Coeliac Disease Genes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid
Comprehensive Summaries of Uppsala Dissertations from the Faculty of Pharmacy 231 _____________________________ _____________________________ Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21 BY JOHAN BYLUND ACTA UNIVERSITATIS UPSALIENSIS UPPSALA 2000 Dissertation for the Degree of Doctor of Philosophy (Faculty of Pharmacy) in Pharmaceutical Pharmacology presented at Uppsala University in 2000 ABSTRACT Bylund, J. 2000. Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid: Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21. Acta Universitatis Upsaliensis. Comprehensive Summaries of Uppsala Dissertations from Faculty of Pharmacy 231 50 pp. Uppsala. ISBN 91-554-4784-8. Cytochrome P450 (P450 or CYP) is an enzyme system involved in the oxygenation of a wide range of endogenous compounds as well as foreign chemicals and drugs. This thesis describes investigations of P450-catalyzed oxygenation of prostaglandins, linoleic and arachidonic acids. The formation of bisallylic hydroxy metabolites of linoleic and arachidonic acids was studied with human recombinant P450s and with human liver microsomes. Several P450 enzymes catalyzed the formation of bisallylic hydroxy metabolites. Inhibition studies and stereochemical analysis of metabolites suggest that the enzyme CYP1A2 may contribute to the biosynthesis of bisallylic hydroxy fatty acid metabolites in adult human liver microsomes. 19R-Hydroxy-PGE and 20-hydroxy-PGE are major components of human and ovine semen, respectively. They are formed in the seminal vesicles, but the mechanism of their biosynthesis is unknown. Reverse transcription-polymerase chain reaction using degenerate primers for mammalian CYP4 family genes, revealed expression of two novel P450 genes in human and ovine seminal vesicles. -

Synonymous Single Nucleotide Polymorphisms in Human Cytochrome
DMD Fast Forward. Published on February 9, 2009 as doi:10.1124/dmd.108.026047 DMD #26047 TITLE PAGE: A BIOINFORMATICS APPROACH FOR THE PHENOTYPE PREDICTION OF NON- SYNONYMOUS SINGLE NUCLEOTIDE POLYMORPHISMS IN HUMAN CYTOCHROME P450S LIN-LIN WANG, YONG LI, SHU-FENG ZHOU Department of Nutrition and Food Hygiene, School of Public Health, Peking University, Beijing 100191, P. R. China (LL Wang & Y Li) Discipline of Chinese Medicine, School of Health Sciences, RMIT University, Bundoora, Victoria 3083, Australia (LL Wang & SF Zhou). 1 Copyright 2009 by the American Society for Pharmacology and Experimental Therapeutics. DMD #26047 RUNNING TITLE PAGE: a) Running title: Prediction of phenotype of human CYPs. b) Author for correspondence: A/Prof. Shu-Feng Zhou, MD, PhD Discipline of Chinese Medicine, School of Health Sciences, RMIT University, WHO Collaborating Center for Traditional Medicine, Bundoora, Victoria 3083, Australia. Tel: + 61 3 9925 7794; fax: +61 3 9925 7178. Email: [email protected] c) Number of text pages: 21 Number of tables: 10 Number of figures: 2 Number of references: 40 Number of words in Abstract: 249 Number of words in Introduction: 749 Number of words in Discussion: 1459 d) Non-standard abbreviations: CYP, cytochrome P450; nsSNP, non-synonymous single nucleotide polymorphism. 2 DMD #26047 ABSTRACT Non-synonymous single nucleotide polymorphisms (nsSNPs) in coding regions that can lead to amino acid changes may cause alteration of protein function and account for susceptivity to disease. Identification of deleterious nsSNPs from tolerant nsSNPs is important for characterizing the genetic basis of human disease, assessing individual susceptibility to disease, understanding the pathogenesis of disease, identifying molecular targets for drug treatment and conducting individualized pharmacotherapy. -

4-6 Weeks Old Female C57BL/6 Mice Obtained from Jackson Labs Were Used for Cell Isolation
Methods Mice: 4-6 weeks old female C57BL/6 mice obtained from Jackson labs were used for cell isolation. Female Foxp3-IRES-GFP reporter mice (1), backcrossed to B6/C57 background for 10 generations, were used for the isolation of naïve CD4 and naïve CD8 cells for the RNAseq experiments. The mice were housed in pathogen-free animal facility in the La Jolla Institute for Allergy and Immunology and were used according to protocols approved by the Institutional Animal Care and use Committee. Preparation of cells: Subsets of thymocytes were isolated by cell sorting as previously described (2), after cell surface staining using CD4 (GK1.5), CD8 (53-6.7), CD3ε (145- 2C11), CD24 (M1/69) (all from Biolegend). DP cells: CD4+CD8 int/hi; CD4 SP cells: CD4CD3 hi, CD24 int/lo; CD8 SP cells: CD8 int/hi CD4 CD3 hi, CD24 int/lo (Fig S2). Peripheral subsets were isolated after pooling spleen and lymph nodes. T cells were enriched by negative isolation using Dynabeads (Dynabeads untouched mouse T cells, 11413D, Invitrogen). After surface staining for CD4 (GK1.5), CD8 (53-6.7), CD62L (MEL-14), CD25 (PC61) and CD44 (IM7), naïve CD4+CD62L hiCD25-CD44lo and naïve CD8+CD62L hiCD25-CD44lo were obtained by sorting (BD FACS Aria). Additionally, for the RNAseq experiments, CD4 and CD8 naïve cells were isolated by sorting T cells from the Foxp3- IRES-GFP mice: CD4+CD62LhiCD25–CD44lo GFP(FOXP3)– and CD8+CD62LhiCD25– CD44lo GFP(FOXP3)– (antibodies were from Biolegend). In some cases, naïve CD4 cells were cultured in vitro under Th1 or Th2 polarizing conditions (3, 4). -
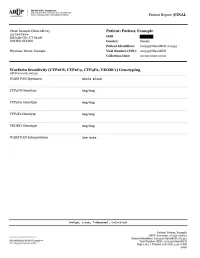
Warfarin Sensitivity (CYP2C8, CYP2C9
Patient Report |FINAL Section 79-1 of New York State Civil Rights Law requires informed consent be obtained from patients (or their legal guardians) prior to pursuing genetic testing. These forms must be kept on file by the ordering physician. Consent forms for genetic testing are available at www.aruplab.com. Incidental findings are not reported unless clinically significant but are available upon request. A Neg result indicates that no variants were detected. All variant alleles are defined based on consensus nomenclature and suggest reduced function of the associated protein(s). CYP2C8 and CYP2C9 are associated with inactivation of warfarin through metabolism. Variant alleles suggest reduced rates of warfarin metabolism, a prolonged time required to achieve steady-state concentrations, and a reduced dose requirement. CYP4F2 is associated with vitamin K recycling. Variant alleles suggest an increased dose requirement. VKORC1 is the therapeutic target for warfarin. Variant alleles suggest increased warfarin sensitivity and a reduced dose requirement. Dosing calculators such as that available through www.WarfarinDosing.org are available to predict loading and therapeutic/maintenance doses. This result has been reviewed and approved by , Ph.D. BACKGROUND INFORMATION: Warfarin Sensitivity (CYP2C8, CYP2C9 , CYP4F2, VKORC1) Genotyping CHARACTERISTICS: Warfarin sensitivity can lead to a life-threatening overdose event such as excessive bleeding. Genetic variation is recognized to explain a large proportion of variability in warfarin dose requirements. This test may predict individual warfarin sensitivity and non-standard dose requirements. The cytochrome P450 (CYP) isozymes 2C8 and 2C9 are involved in the metabolism of many drugs. Variants in the genes that code for CYP2C8 and CYP2C9 may influence pharmacokinetics of substrates such as warfarin, and may predict or explain non-standard dose requirements, therapeutic failure or adverse reactions. -

Supplementary Tables, Figures and Other Documents
Clinical Relevance of a 16-Gene Pharmacogenetic Panel Test for Medication Management in a Cohort of 135 Patients David Niedrig1,2, Ali Rahmany1,3, Kai Heib4, Karl-Dietrich Hatz4, Katja Ludin5, Andrea M. Burden3, Markus Béchir6, Andreas Serra7, Stefan Russmann1,3,7,* 1 drugsafety.ch; Zurich, Switzerland 2 Hospital Pharmacy, Clinic Hirslanden Zurich; Zurich Switzerland 3 Swiss Federal Institute of Technology Zurich (ETHZ); Zurich, Switzerland 4 INTLAB AG; Uetikon am See, Switzerland 5 Labor Risch, Molecular Genetics; Berne, Switzerland 6 Center for Internal Medicine, Clinic Hirslanden Aarau; Aarau, Switzerland 7 Institute of Internal Medicine and Nephrology, Clinic Hirslanden Zurich; Zurich, Switzerland * Correspondence: [email protected]; Tel.: +41 (0)44 221 1003 Supplementary Tables, Figures and Other Documents Figure S1: Example of credit-card sized pharmacogenomic profile issued to patients 1 Table S2: SNPs analyzed by the 16-gene panel test Gene Allele rs number ABCB1 Haplotypes 1236-2677- rs1045642 ABCB1 3435 rs1128503 ABCB1 rs2032582 COMT Haplotypes 6269-4633- rs4633 COMT 4818-4680 rs4680 COMT rs4818 COMT rs6269 CYP1A2 *1C rs2069514 CYP1A2 *1F rs762551 CYP1A2 *1K rs12720461 CYP1A2 *7 rs56107638 CYP1A2 *11 rs72547513 CYP2B6 *6 rs3745274 CYP2B6 *18 rs28399499 CYP2C19 *2 rs4244285 CYP2C19 *3 rs4986893 CYP2C19 *4 rs28399504 CYP2C19 *5 rs56337013 CYP2C19 *6 rs72552267 CYP2C19 *7 rs72558186 CYP2C19 *8 rs41291556 CYP2C19 *17 rs12248560 CYP2C9 *2 rs1799853 CYP2C9 *3 rs1057910 CYP2C9 *4 rs56165452 CYP2C9 *5 rs28371686 CYP2C9 *6 rs9332131 CYP2C9 -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -
Molecular Effects of Fermentation in the Gut and Its Relevance for Metabolism and Satiety
Molecular effects of fermentation in the gut and its relevance for metabolism and satiety Daniëlle Haenen Thesis committee Promotor Prof. Dr Michael R. Müller Professor of Nutrition, Metabolism and Genomics Wageningen University Co-promotors Dr Guido J.E.J. Hooiveld Assistant professor, Division of Human Nutrition Wageningen University Prof. Dr Bas Kemp Professor of Adaptation Physiology Wageningen University Other members Prof. Dr Renger F. Witkamp, Wageningen University Prof. Dr Wouter H. Hendriks, Wageningen University Prof. Dr Michiel Kleerebezem, Wageningen University Prof. Dr Albert K. Groen, University of Groningen This research was conducted under the auspices of the Graduate School VLAG (Advanced studies in Food Technology, Agrobiotechnology, Nutrition and Health Sciences). Molecular effects of fermentation in the gut and its relevance for metabolism and satiety Daniëlle Haenen Thesis submitted in fulfilment of the requirements for the degree of doctor at Wageningen University by the authority of the Rector Magnificus Prof. Dr M.J. Kropff, in the presence of the Thesis Committee appointed by the Academic Board to be defended in public on Wednesday 18 September 2013 at 1.30 p.m. in the Aula. Daniëlle Haenen Molecular effects of fermentation in the gut and its relevance for metabolism and satiety 210 pages PhD thesis, Wageningen University, Wageningen, NL (2013) With references, with summary in Dutch ISBN 978-94-6173-667-3 Abstract Dietary fibres, the edible parts of plants that are resistant to digestion and absorption in the human small intestine, were shown to be important in the prevention of obesity and the metabolic syndrome. This association can partially be attributed to a fibre-induced increase in satiety. -

Clinical Implications of 20-Hydroxyeicosatetraenoic Acid in the Kidney, Liver, Lung and Brain
1 Review 2 Clinical Implications of 20-Hydroxyeicosatetraenoic 3 Acid in the Kidney, Liver, Lung and Brain: An 4 Emerging Therapeutic Target 5 Osama H. Elshenawy 1, Sherif M. Shoieb 1, Anwar Mohamed 1,2 and Ayman O.S. El-Kadi 1,* 6 1 Faculty of Pharmacy and Pharmaceutical Sciences, University of Alberta, Edmonton T6G 2E1, AB, Canada; 7 [email protected] (O.H.E.); [email protected] (S.M.S.); [email protected] (A.M.) 8 2 Department of Basic Medical Sciences, College of Medicine, Mohammed Bin Rashid University of 9 Medicine and Health Sciences, Dubai, United Arab Emirates 10 * Correspondence: [email protected]; Tel.: 780-492-3071; Fax: 780-492-1217 11 Academic Editor: Kishor M. Wasan 12 Received: 12 January 2017; Accepted: 15 February 2017; Published: 20 February 2017 13 Abstract: Cytochrome P450-mediated metabolism of arachidonic acid (AA) is an important 14 pathway for the formation of eicosanoids. The ω-hydroxylation of AA generates significant levels 15 of 20-hydroxyeicosatetraenoic acid (20-HETE) in various tissues. In the current review, we discussed 16 the role of 20-HETE in the kidney, liver, lung, and brain during physiological and 17 pathophysiological states. Moreover, we discussed the role of 20-HETE in tumor formation, 18 metabolic syndrome and diabetes. In the kidney, 20-HETE is involved in modulation of 19 preglomerular vascular tone and tubular ion transport. Furthermore, 20-HETE is involved in renal 20 ischemia/reperfusion (I/R) injury and polycystic kidney diseases. The role of 20-HETE in the liver is 21 not clearly understood although it represents 50%–75% of liver CYP-dependent AA metabolism, 22 and it is associated with liver cirrhotic ascites. -

Identification of the Cytochrome P450 Enzymes Responsible for the X
FEBS Letters 580 (2006) 3794–3798 Identification of the cytochrome P450 enzymes responsible for the x-hydroxylation of phytanic acid J.C. Komen, R.J.A. Wanders* Departments of Clinical Chemistry and Pediatrics, Emma Children’s Hospital, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands Received 27 March 2006; revised 26 May 2006; accepted 30 May 2006 Available online 9 June 2006 Edited by Sandro Sonnino tanic acid occurs effectively by bacteria present in the rumen Abstract Patients suffering from Refsum disease have a defect in the a-oxidation pathway which results in the accumulation of of ruminants. phytanic acid in plasma and tissues. Our previous studies have Phytanic acid accumulates in patients with adult Refsum dis- shown that phytanic acid is also a substrate for the x-oxidation ease (ARD, MIM 266500) which is due to a defect in the a-oxi- pathway. With the use of specific inhibitors we now show that dation pathway caused by mutations in one of two genes members of the cytochrome P450 (CYP450) family 4 class are including the PAHX gene which codes for phytanoyl-CoA responsible for phytanic acid x-hydroxylation. Incubations with hydroxylase [2,3], and the PEX7 gene which codes for the microsomes containing human recombinant CYP450s (Super- PTS2 receptor [4]. The majority of ARD patients have muta- TM somes ) revealed that multiple CYP450 enzymes of the family tions in the PAHX gene. The increased levels of phytanic acid 4 class are able to x-hydroxylate phytanic acid with the follow- in plasma and tissues are thought to be the direct cause for the ing order of efficiency: CYP4F3A > CYP4F3B > CYP4F2 > pathology of the disease. -

Cytochrome P450 Expression and Activities in Human Tongue Cells and Their Modulation by Green Tea Extract
Cytochrome P450 expression and activities in human tongue cells and their modulation by green tea extract By: Shin-Pei Yang, and Gregory M. Raner Yang, S.-P. and Raner, G.M. Cytochrome P450 Expression, Induction and Activities in Human Tongue Cells and their Modulation by Green Tea Extract, Toxicol. Appl. Pharmacol. 202, 140-150 (2005). DOI: 10.1016/j.taap.2004.06.014 Made available courtesy of Elsevier: http://www.elsevier.com/wps/find/homepage.cws_home ***Reprinted with permission. No further reproduction is authorized without written permission from Elsevier. This version of the document is not the version of record. Figures and/or pictures may be missing from this format of the document.*** Abstract: The expression, inducibility, and activities of several cytochrome P450 (CYP) enzymes were investigated in a human tongue carcinoma cell model, CAL 27, and compared with the human liver model HepG2 cells. The modulation effects of green tea on various CYP isoforms in both cell lines were also examined. RT-PCR analysis of CAL 27 cells demonstrated constitutive expression of mRNA for CYPs 1A1, 1A2, 2C, 2E1, 2D6, and 4F3. The results were negative for CYP2A6, 2B6/7, 3A3/4, and 3A7. Both cell lines displayed identical expression and induction profiles for all of the isoforms examined in this study except 3A7 and 2B6/7, which were produced constitutively in HepG2 but not Cal-27 cells. CYP1A1 and 1A2 were both induced by treatment with β-napthoflavone as indicated by RT-PCR and Western blotting, while CYP2C mRNA was upregulated by all-trans retinoic acid and farnesol. -

Effect of Genetic Variability in the CYP4F2, CYP4F11 and CYP4F12 Genes on Liver Mrna Levels and Warfarin Response
Effect of genetic variability in the CYP4F2, CYP4F11 and CYP4F12 genes on liver mRNA levels and warfarin response J. Eunice Zhang1, Kathrin Klein2, Andrea L. Jorgensen3, Ben Francis3, Ana Alfirevic1, Stephane Bourgeois4, Panagiotis Deloukas4,5,6, Ulrich M. Zanger2 and Munir Pirmohamed1* 1Wolfson Centre for Personalized Medicine, Department of Molecular & Clinical Pharmacology, The University of Liverpool, UK 2Dr Margarete Fischer-Bosch Institute of Clinical Pharmacology, Stuttgart, and University of Tuebingen, Tuebingen, Germany. 3Department of Biostatistics, The University of Liverpool, UK 4William Harvey Research Institute, Barts and the London School of Medicine and Dentistry, Queen Mary University of London, UK 5Wellcome Trust Sanger Institute, Hinxton, Cambridge, UK. 6Princess Al-Jawhara Al-Brahim Centre of Excellence in Research of Hereditary Disorders, King Abdulaziz University, Jeddah, Saudi Arabia. Correspondence: Professor Sir Munir Pirmohamed Wolfson Centre for Personalised Medicine Department of Molecular & Clinical Pharmacology Block A: Waterhouse Buildings The University of Liverpool 1-5 Brownlow Street L69 3GL, UK [email protected] Running Title: Genotype-phenotype assessment of CYP4F12-CYP4F2-CYP4F11 region Keywords: warfarin, pharmacogenetics, mRNA expression, CYP4F2, CYP4F11, CYP4F12 1 Abstract Genetic polymorphisms in the gene encoding cytochrome P450 (CYP) 4F2, a vitamin K oxidase, affect stable warfarin dose requirements and time to therapeutic INR. CYP4F2 is part of the CYP4F gene cluster, which is highly polymorphic and exhibits a high degree of linkage disequilibrium, making it difficult to define causal variants. Our objective was to examine the effect of genetic variability in the CYP4F gene cluster on expression of the individual CYP4F genes and warfarin response. mRNA levels of the CYP4F gene cluster were quantified in human liver samples (n=149) obtained from a well characterized liver bank and fine mapping of the CYP4F gene cluster encompassing CYP4F2, CYP4F11 and CYP4F12 was performed. -

Expression of CYP2S1 in Human Hepatic Stellate Cells
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector FEBS Letters 581 (2007) 781–786 Expression of CYP2S1 in human hepatic stellate cells Carylyn J. Mareka, Steven J. Tuckera, Matthew Korutha, Karen Wallacea,b, Matthew C. Wrighta,b,* a School of Medical Sciences, Institute of Medical Science, University of Aberdeen, Aberdeen, UK b Liver Faculty Research Group, School of Clinical and Laboratory Sciences, University of Newcastle, Newcastle, UK Received 22 November 2006; revised 16 January 2007; accepted 23 January 2007 Available online 2 February 2007 Edited by Laszlo Nagy the expression and accumulation of scarring extracellular Abstract Activated stellate cells are myofibroblast-like cells associated with the generation of fibrotic scaring in chronically fibrotic matrix protein [2]. It is currently thought an inhibition damaged liver. Gene chip analysis was performed on cultured fi- of fibrosis in liver diseases may be an effective approach to brotic stellate cells. Of the 51 human CYP genes known, 13 treating patients for which the cause is refractive to current CYP and 5 CYP reduction-related genes were detected with 4 treatments (e.g. in approx. 30% of hepatitis C infected CYPs (CYP1A1, CYP2E1, CY2S1 and CYP4F3) consistently patients) [2,3]. At present, there is no approved treatment for present in stellate cells isolated from three individuals. Quantita- fibrosis. tive RT-PCR indicated that CYP2S1 was a major expressed Inadvertent toxicity of drugs is often associated with a ‘‘met- CYP mRNA transcript. The presence of a CYP2A-related pro- abolic activation’’ by CYPs [1].