Supplementary Tables, Figures and Other Documents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Report of the Advisory Group to Recommend Priorities for the IARC Monographs During 2020–2024
IARC Monographs on the Identification of Carcinogenic Hazards to Humans Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 CONTENTS Introduction ................................................................................................................................... 1 Acetaldehyde (CAS No. 75-07-0) ................................................................................................. 3 Acrolein (CAS No. 107-02-8) ....................................................................................................... 4 Acrylamide (CAS No. 79-06-1) .................................................................................................... 5 Acrylonitrile (CAS No. 107-13-1) ................................................................................................ 6 Aflatoxins (CAS No. 1402-68-2) .................................................................................................. 8 Air pollutants and underlying mechanisms for breast cancer ....................................................... 9 Airborne gram-negative bacterial endotoxins ............................................................................. 10 Alachlor (chloroacetanilide herbicide) (CAS No. 15972-60-8) .................................................. 10 Aluminium (CAS No. 7429-90-5) .............................................................................................. 11 -

Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid
Comprehensive Summaries of Uppsala Dissertations from the Faculty of Pharmacy 231 _____________________________ _____________________________ Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21 BY JOHAN BYLUND ACTA UNIVERSITATIS UPSALIENSIS UPPSALA 2000 Dissertation for the Degree of Doctor of Philosophy (Faculty of Pharmacy) in Pharmaceutical Pharmacology presented at Uppsala University in 2000 ABSTRACT Bylund, J. 2000. Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid: Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21. Acta Universitatis Upsaliensis. Comprehensive Summaries of Uppsala Dissertations from Faculty of Pharmacy 231 50 pp. Uppsala. ISBN 91-554-4784-8. Cytochrome P450 (P450 or CYP) is an enzyme system involved in the oxygenation of a wide range of endogenous compounds as well as foreign chemicals and drugs. This thesis describes investigations of P450-catalyzed oxygenation of prostaglandins, linoleic and arachidonic acids. The formation of bisallylic hydroxy metabolites of linoleic and arachidonic acids was studied with human recombinant P450s and with human liver microsomes. Several P450 enzymes catalyzed the formation of bisallylic hydroxy metabolites. Inhibition studies and stereochemical analysis of metabolites suggest that the enzyme CYP1A2 may contribute to the biosynthesis of bisallylic hydroxy fatty acid metabolites in adult human liver microsomes. 19R-Hydroxy-PGE and 20-hydroxy-PGE are major components of human and ovine semen, respectively. They are formed in the seminal vesicles, but the mechanism of their biosynthesis is unknown. Reverse transcription-polymerase chain reaction using degenerate primers for mammalian CYP4 family genes, revealed expression of two novel P450 genes in human and ovine seminal vesicles. -

Synonymous Single Nucleotide Polymorphisms in Human Cytochrome
DMD Fast Forward. Published on February 9, 2009 as doi:10.1124/dmd.108.026047 DMD #26047 TITLE PAGE: A BIOINFORMATICS APPROACH FOR THE PHENOTYPE PREDICTION OF NON- SYNONYMOUS SINGLE NUCLEOTIDE POLYMORPHISMS IN HUMAN CYTOCHROME P450S LIN-LIN WANG, YONG LI, SHU-FENG ZHOU Department of Nutrition and Food Hygiene, School of Public Health, Peking University, Beijing 100191, P. R. China (LL Wang & Y Li) Discipline of Chinese Medicine, School of Health Sciences, RMIT University, Bundoora, Victoria 3083, Australia (LL Wang & SF Zhou). 1 Copyright 2009 by the American Society for Pharmacology and Experimental Therapeutics. DMD #26047 RUNNING TITLE PAGE: a) Running title: Prediction of phenotype of human CYPs. b) Author for correspondence: A/Prof. Shu-Feng Zhou, MD, PhD Discipline of Chinese Medicine, School of Health Sciences, RMIT University, WHO Collaborating Center for Traditional Medicine, Bundoora, Victoria 3083, Australia. Tel: + 61 3 9925 7794; fax: +61 3 9925 7178. Email: [email protected] c) Number of text pages: 21 Number of tables: 10 Number of figures: 2 Number of references: 40 Number of words in Abstract: 249 Number of words in Introduction: 749 Number of words in Discussion: 1459 d) Non-standard abbreviations: CYP, cytochrome P450; nsSNP, non-synonymous single nucleotide polymorphism. 2 DMD #26047 ABSTRACT Non-synonymous single nucleotide polymorphisms (nsSNPs) in coding regions that can lead to amino acid changes may cause alteration of protein function and account for susceptivity to disease. Identification of deleterious nsSNPs from tolerant nsSNPs is important for characterizing the genetic basis of human disease, assessing individual susceptibility to disease, understanding the pathogenesis of disease, identifying molecular targets for drug treatment and conducting individualized pharmacotherapy. -

Phototoxicity of 7-Oxycoumarins with Keratinocytes in Culture T ⁎ Christophe Guillona, , Yi-Hua Janb, Diane E
Bioorganic Chemistry 89 (2019) 103014 Contents lists available at ScienceDirect Bioorganic Chemistry journal homepage: www.elsevier.com/locate/bioorg Phototoxicity of 7-oxycoumarins with keratinocytes in culture T ⁎ Christophe Guillona, , Yi-Hua Janb, Diane E. Heckc, Thomas M. Marianob, Robert D. Rappa, Michele Jettera, Keith Kardosa, Marilyn Whittemored, Eric Akyeaa, Ivan Jabine, Jeffrey D. Laskinb, Ned D. Heindela a Department of Chemistry, Lehigh University, Bethlehem, PA 18015, USA b Department of Environmental and Occupational Health, Rutgers University School of Public Health, Piscataway, NJ 08854, USA c Department of Environmental Science, New York Medical College, Valhalla, NY 10595, USA d Buckman Laboratories, 1256 N. McLean Blvd, Memphis, TN 38108, USA e Laboratoire de Chimie Organique, Université Libre de Bruxelles, B-1050 Brussels, Belgium ARTICLE INFO ABSTRACT Keywords: Seventy-one 7-oxycoumarins, 66 synthesized and 5 commercially sourced, were tested for their ability to inhibit 7-hydroxycoumarins growth in murine PAM212 keratinocytes. Forty-nine compounds from the library demonstrated light-induced 7-oxycoumarins lethality. None was toxic in the absence of UVA light. Structure-activity correlations indicate that the ability of Furocoumarins the compounds to inhibit cell growth was dependent not only on their physiochemical characteristics, but also Psoralens on their ability to absorb UVA light. Relative lipophilicity was an important factor as was electron density in the Methoxsalen pyrone ring. Coumarins with electron withdrawing moieties – cyano and fluoro at C – were considerably less 8-MOP 3 Phototoxicity active while those with bromines or iodine at that location displayed enhanced activity. Coumarins that were PAM212 keratinocytes found to inhibit keratinocyte growth were also tested for photo-induced DNA plasmid nicking. -
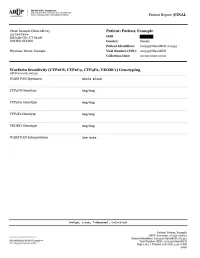
Warfarin Sensitivity (CYP2C8, CYP2C9
Patient Report |FINAL Section 79-1 of New York State Civil Rights Law requires informed consent be obtained from patients (or their legal guardians) prior to pursuing genetic testing. These forms must be kept on file by the ordering physician. Consent forms for genetic testing are available at www.aruplab.com. Incidental findings are not reported unless clinically significant but are available upon request. A Neg result indicates that no variants were detected. All variant alleles are defined based on consensus nomenclature and suggest reduced function of the associated protein(s). CYP2C8 and CYP2C9 are associated with inactivation of warfarin through metabolism. Variant alleles suggest reduced rates of warfarin metabolism, a prolonged time required to achieve steady-state concentrations, and a reduced dose requirement. CYP4F2 is associated with vitamin K recycling. Variant alleles suggest an increased dose requirement. VKORC1 is the therapeutic target for warfarin. Variant alleles suggest increased warfarin sensitivity and a reduced dose requirement. Dosing calculators such as that available through www.WarfarinDosing.org are available to predict loading and therapeutic/maintenance doses. This result has been reviewed and approved by , Ph.D. BACKGROUND INFORMATION: Warfarin Sensitivity (CYP2C8, CYP2C9 , CYP4F2, VKORC1) Genotyping CHARACTERISTICS: Warfarin sensitivity can lead to a life-threatening overdose event such as excessive bleeding. Genetic variation is recognized to explain a large proportion of variability in warfarin dose requirements. This test may predict individual warfarin sensitivity and non-standard dose requirements. The cytochrome P450 (CYP) isozymes 2C8 and 2C9 are involved in the metabolism of many drugs. Variants in the genes that code for CYP2C8 and CYP2C9 may influence pharmacokinetics of substrates such as warfarin, and may predict or explain non-standard dose requirements, therapeutic failure or adverse reactions. -

Pp375-430-Annex 1.Qxd
ANNEX 1 CHEMICAL AND PHYSICAL DATA ON COMPOUNDS USED IN COMBINED ESTROGEN–PROGESTOGEN CONTRACEPTIVES AND HORMONAL MENOPAUSAL THERAPY Annex 1 describes the chemical and physical data, technical products, trends in produc- tion by region and uses of estrogens and progestogens in combined estrogen–progestogen contraceptives and hormonal menopausal therapy. Estrogens and progestogens are listed separately in alphabetical order. Trade names for these compounds alone and in combination are given in Annexes 2–4. Sales are listed according to the regions designated by WHO. These are: Africa: Algeria, Angola, Benin, Botswana, Burkina Faso, Burundi, Cameroon, Cape Verde, Central African Republic, Chad, Comoros, Congo, Côte d'Ivoire, Democratic Republic of the Congo, Equatorial Guinea, Eritrea, Ethiopia, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Kenya, Lesotho, Liberia, Madagascar, Malawi, Mali, Mauritania, Mauritius, Mozambique, Namibia, Niger, Nigeria, Rwanda, Sao Tome and Principe, Senegal, Seychelles, Sierra Leone, South Africa, Swaziland, Togo, Uganda, United Republic of Tanzania, Zambia and Zimbabwe America (North): Canada, Central America (Antigua and Barbuda, Bahamas, Barbados, Belize, Costa Rica, Cuba, Dominica, El Salvador, Grenada, Guatemala, Haiti, Honduras, Jamaica, Mexico, Nicaragua, Panama, Puerto Rico, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and the Grenadines, Suriname, Trinidad and Tobago), United States of America America (South): Argentina, Bolivia, Brazil, Chile, Colombia, Dominican Republic, Ecuador, Guyana, Paraguay, -

Pharmacy and Poisons (Third and Fourth Schedule Amendment) Order 2017
Q UO N T FA R U T A F E BERMUDA PHARMACY AND POISONS (THIRD AND FOURTH SCHEDULE AMENDMENT) ORDER 2017 BR 111 / 2017 The Minister responsible for health, in exercise of the power conferred by section 48A(1) of the Pharmacy and Poisons Act 1979, makes the following Order: Citation 1 This Order may be cited as the Pharmacy and Poisons (Third and Fourth Schedule Amendment) Order 2017. Repeals and replaces the Third and Fourth Schedule of the Pharmacy and Poisons Act 1979 2 The Third and Fourth Schedules to the Pharmacy and Poisons Act 1979 are repealed and replaced with— “THIRD SCHEDULE (Sections 25(6); 27(1))) DRUGS OBTAINABLE ONLY ON PRESCRIPTION EXCEPT WHERE SPECIFIED IN THE FOURTH SCHEDULE (PART I AND PART II) Note: The following annotations used in this Schedule have the following meanings: md (maximum dose) i.e. the maximum quantity of the substance contained in the amount of a medicinal product which is recommended to be taken or administered at any one time. 1 PHARMACY AND POISONS (THIRD AND FOURTH SCHEDULE AMENDMENT) ORDER 2017 mdd (maximum daily dose) i.e. the maximum quantity of the substance that is contained in the amount of a medicinal product which is recommended to be taken or administered in any period of 24 hours. mg milligram ms (maximum strength) i.e. either or, if so specified, both of the following: (a) the maximum quantity of the substance by weight or volume that is contained in the dosage unit of a medicinal product; or (b) the maximum percentage of the substance contained in a medicinal product calculated in terms of w/w, w/v, v/w, or v/v, as appropriate. -

Enhancement of Hepatocarcinogenesis in Female Rats by Ethinyl Estradici and Mestranol but Not Estradici1
[CANCER RESEARCH 44, 3862-3869, September 1984] Enhancement of Hepatocarcinogenesis in Female Rats by Ethinyl Estradici and Mestranol but not Estradici1 James D. Yager,2 Harold A. Campbell, Daniel S. Longnecker, B. D. Roebuck, and Mary C. Benoit Departments ölAnatomy [J. D. Y.¡,Pathology [D. S. L], Pharmacology and Toxicology [B. D. R.¡,and Medicine [M. C. B.], Dartmouth Medical School, Hanover, New Hampshire 03756, and McArdle Laboratory tor Cancer Research, University of Wisconsin Medical School, Madison, Wisconsin 53706 [H. A. C.] ABSTRACT In experimental studies in animals, results have been obtained which suggest that synthetic estrogen treatment following car The effect of dietary exposure to synthetic estrogens on cinogen exposure (initiation) can enhance hepatic neoplasia. hepatocarcinogenesis was evaluated. Diethylnitrosamine-initi- Taper (32) was the first investigator to demonstrate that 2 ated and 0.85% NaCI solution-treated noninitiated female synthetic steroids used in oral contraceptive preparations in Sprague-Dawley rats were transferred to semisynthetic diets Europe, estradiol 17-phenylpropionate and estradiol benzoate, containing mestranol (0, 0.1, or 0.5 ppm), ethinyl estradiol (0.5 enhanced hepatocarcinogenesis in castrated female rats previ ppm), estradiol (0.6 ppm), or mestranol plus 0-methasone (0.5 ously initiated with A/-nitrosomorpholine In the United States, 2 and 0.2 ppm, respectively). 7-Glutamyl transferase (GGT>posi- synthetic estrogens, mestranol (170-ethinyl estradiol 3-methyl tive transections and hematoxylin and eosin-detectable nodules ether) and EE, are widely used in oral contraceptive preparations. and carcinomas were scored at 9 and 12 months. Quantitative We reported that, in intact, DEN-initiatedfemale Sprague-Dawley stereological calculations were performed to determine GGT rats, mestranol alone and together with norethynodrel enhanced lesion number and size. -

Clinical Implications of 20-Hydroxyeicosatetraenoic Acid in the Kidney, Liver, Lung and Brain
1 Review 2 Clinical Implications of 20-Hydroxyeicosatetraenoic 3 Acid in the Kidney, Liver, Lung and Brain: An 4 Emerging Therapeutic Target 5 Osama H. Elshenawy 1, Sherif M. Shoieb 1, Anwar Mohamed 1,2 and Ayman O.S. El-Kadi 1,* 6 1 Faculty of Pharmacy and Pharmaceutical Sciences, University of Alberta, Edmonton T6G 2E1, AB, Canada; 7 [email protected] (O.H.E.); [email protected] (S.M.S.); [email protected] (A.M.) 8 2 Department of Basic Medical Sciences, College of Medicine, Mohammed Bin Rashid University of 9 Medicine and Health Sciences, Dubai, United Arab Emirates 10 * Correspondence: [email protected]; Tel.: 780-492-3071; Fax: 780-492-1217 11 Academic Editor: Kishor M. Wasan 12 Received: 12 January 2017; Accepted: 15 February 2017; Published: 20 February 2017 13 Abstract: Cytochrome P450-mediated metabolism of arachidonic acid (AA) is an important 14 pathway for the formation of eicosanoids. The ω-hydroxylation of AA generates significant levels 15 of 20-hydroxyeicosatetraenoic acid (20-HETE) in various tissues. In the current review, we discussed 16 the role of 20-HETE in the kidney, liver, lung, and brain during physiological and 17 pathophysiological states. Moreover, we discussed the role of 20-HETE in tumor formation, 18 metabolic syndrome and diabetes. In the kidney, 20-HETE is involved in modulation of 19 preglomerular vascular tone and tubular ion transport. Furthermore, 20-HETE is involved in renal 20 ischemia/reperfusion (I/R) injury and polycystic kidney diseases. The role of 20-HETE in the liver is 21 not clearly understood although it represents 50%–75% of liver CYP-dependent AA metabolism, 22 and it is associated with liver cirrhotic ascites. -

Comparison of Two Diluents of 1% Methoxsalen in the Treatment of Vitiligo
Net Letter eye care/cosmetic products should also be tested. Though anterior chamber after instillation of 10% phenylephrine phenylephrine is widely used by ophthalmologists in India hydrochloride solution. Br J Ophthalmol 1974;55:554-9. in nonhypertensive adults as a mydriatic agent to obtain 2. Wigger-Alberti W, Elsner P, Wuthrich B. Allergic contact maximum pupillary dilatation prior to fundus examination dermatitis to phenylephrine. Allergy 1998;53:217-8. 3. Yamamoto A, Harada S, Nakada T, Iijima M. Contact and assessment of refractory errors, allergic contact dermatitis to phenylephrine hydrochloride eyedrops. Clin dermatitis has not been reported from this country so far. Exp Dermatol 2004:29;200-1. This may be partly due to a low index of suspicion or failure 4. Herbst RA, Uter W, Pirker C, Geier J, Frosch PJ. Allergic and to perform patch tests in patients with transient and self- non-allergic periorbital dermatitis: Patch test results of the healing periorbital dermatitis. Information Network of the Department of Dermatology during a 5-year period. Contact Dermatitis 2004;51:13-9. RREFERENCESEFERENCES 5. Borch JE, Elmquist JS, Bindslevjensen C, Anderson KE. Phenylephrine and acute periorbital dermatitis. Contact 1. Agarwall Jl, Beveridge B. Liberation of iris pigment in the Dermatitis 2005;53:298-9. CComparisonomparison ofof twotwo ddiluentsiluents ooff 11%% mmethoxsalenethoxsalen inin thethe ttreatmentreatment ooff vvitiligoitiligo KKiraniran VV.. GGodseodse Consultant Dermatologist, Shree Skin Center and Laboratory, Mumbai, India AAddressddress fforor ccorrespondence:orrespondence: Dr. Kiran Godse, Shree Skin Center and Laboratory, 21/22, L market, Sector 8, Nerul, Navi Mumbai - 400 706, India. E-mail: [email protected] Sir, less than 20% of the body surface area. -
Predicting Drug Interactions from Dissolution Studies
PREDICTING DRUG INTERACTIONS FROM DISSOLUTION STUDIES Imre Klebovich Semmelweis University Department of Pharmaceutics Disso India – Goa 2015 International Annual Symposium on Dissolution Science 31 st August– 1st September, 2015, Goa, India THE BASIC LOGIC OF NOVEL DRUG RESEARCH CONCEPT in-celebro in-silico in-vitro in-vivo MAIN TYPES OF DRUG INTERACTIONS - Drug - Food - Alcohol Pleasure-giving - Smoking materials - Caffeine Drug - Transporters Interactions - Pharmacogenomics - Psychoactive drugs - Antacid and inhibitor of gastric juice secretion DRUG-FOOD INTERACTION COMPARISON ON IN VITRO DISSOLUTION AND IN VIVO HUMAN ABSORPTION PARAMETERS ON FIVE DIFFERENT ORAL FLUMECINOL PREPARATIONS CHEMICAL STRUCTURE OF FLUMECINOL (ZIXORYNR) hepatic enzyme inducer (CYP-450 2B1) METHOD OF FORMULATION OF DIFFERENT ORAL FLUMECINOL PREPARATIONS Symbol Formulation Methodfortechnology adsorbate in hard absorption of flumecinol on O—O Adsorbate gelatine capsule the surface of silicium dioxide microcapsules in hard microencapsulation by Δ—Δ Microcapsules gelaine capsule coacervation technique ß-cyclodextrine inclusion complexation by x—x tablet inclusion complex ß-cyclodextrine micropellets in hard forming of micropellets by a □—□ Micropellets I. gelaine capsule I. centrifugal granulator micropellets in hard forming of micropellets by a ●—● Micropellets II. gelaine capsule II. centrifugal granulator MEAN CUMULATIVE PERCENT OF FLUMECINOL IN VITRO DISSOLVED AT PH 1.2 OF FIVE FORMULATIONS PHARMACOKINETIC CURVES OF FLUMECINOL IN HUMAN AFTER 100 MG SINGLE ORAL -

A Pharmaceutical Product for Hormone Replacement Therapy Comprising Tibolone Or a Derivative Thereof and Estradiol Or a Derivative Thereof
Europäisches Patentamt *EP001522306A1* (19) European Patent Office Office européen des brevets (11) EP 1 522 306 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.7: A61K 31/567, A61K 31/565, 13.04.2005 Bulletin 2005/15 A61P 15/12 (21) Application number: 03103726.0 (22) Date of filing: 08.10.2003 (84) Designated Contracting States: • Perez, Francisco AT BE BG CH CY CZ DE DK EE ES FI FR GB GR 08970 Sant Joan Despi (Barcelona) (ES) HU IE IT LI LU MC NL PT RO SE SI SK TR • Banado M., Carlos Designated Extension States: 28033 Madrid (ES) AL LT LV MK (74) Representative: Markvardsen, Peter et al (71) Applicant: Liconsa, Liberacion Controlada de Markvardsen Patents, Sustancias Activas, S.A. Patent Department, 08028 Barcelona (ES) P.O. Box 114, Favrholmvaenget 40 (72) Inventors: 3400 Hilleroed (DK) • Palacios, Santiago 28001 Madrid (ES) (54) A pharmaceutical product for hormone replacement therapy comprising tibolone or a derivative thereof and estradiol or a derivative thereof (57) A pharmaceutical product comprising an effec- arate or sequential use in a method for hormone re- tive amount of tibolone or derivative thereof, an effective placement therapy or prevention of hypoestrogenism amount of estradiol or derivative thereof and a pharma- associated clinical symptoms in a human person, in par- ceutically acceptable carrier, wherein the product is pro- ticular wherein the human is a postmenopausal woman. vided as a combined preparation for simultaneous, sep- EP 1 522 306 A1 Printed by Jouve, 75001 PARIS (FR) 1 EP 1 522 306 A1 2 Description [0008] The review article of Journal of Steroid Bio- chemistry and Molecular Biology (2001), 76(1-5), FIELD OF THE INVENTION: 231-238 provides a review of some of these compara- tive studies.