Effect of Genetic Variability in the CYP4F2, CYP4F11 and CYP4F12 Genes on Liver Mrna Levels and Warfarin Response
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid
Comprehensive Summaries of Uppsala Dissertations from the Faculty of Pharmacy 231 _____________________________ _____________________________ Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21 BY JOHAN BYLUND ACTA UNIVERSITATIS UPSALIENSIS UPPSALA 2000 Dissertation for the Degree of Doctor of Philosophy (Faculty of Pharmacy) in Pharmaceutical Pharmacology presented at Uppsala University in 2000 ABSTRACT Bylund, J. 2000. Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid: Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21. Acta Universitatis Upsaliensis. Comprehensive Summaries of Uppsala Dissertations from Faculty of Pharmacy 231 50 pp. Uppsala. ISBN 91-554-4784-8. Cytochrome P450 (P450 or CYP) is an enzyme system involved in the oxygenation of a wide range of endogenous compounds as well as foreign chemicals and drugs. This thesis describes investigations of P450-catalyzed oxygenation of prostaglandins, linoleic and arachidonic acids. The formation of bisallylic hydroxy metabolites of linoleic and arachidonic acids was studied with human recombinant P450s and with human liver microsomes. Several P450 enzymes catalyzed the formation of bisallylic hydroxy metabolites. Inhibition studies and stereochemical analysis of metabolites suggest that the enzyme CYP1A2 may contribute to the biosynthesis of bisallylic hydroxy fatty acid metabolites in adult human liver microsomes. 19R-Hydroxy-PGE and 20-hydroxy-PGE are major components of human and ovine semen, respectively. They are formed in the seminal vesicles, but the mechanism of their biosynthesis is unknown. Reverse transcription-polymerase chain reaction using degenerate primers for mammalian CYP4 family genes, revealed expression of two novel P450 genes in human and ovine seminal vesicles. -

Transcriptomic Characterization of Fibrolamellar Hepatocellular
Transcriptomic characterization of fibrolamellar PNAS PLUS hepatocellular carcinoma Elana P. Simona, Catherine A. Freijeb, Benjamin A. Farbera,c, Gadi Lalazara, David G. Darcya,c, Joshua N. Honeymana,c, Rachel Chiaroni-Clarkea, Brian D. Dilld, Henrik Molinad, Umesh K. Bhanote, Michael P. La Quagliac, Brad R. Rosenbergb,f, and Sanford M. Simona,1 aLaboratory of Cellular Biophysics, The Rockefeller University, New York, NY 10065; bPresidential Fellows Laboratory, The Rockefeller University, New York, NY 10065; cDivision of Pediatric Surgery, Department of Surgery, Memorial Sloan-Kettering Cancer Center, New York, NY 10065; dProteomics Resource Center, The Rockefeller University, New York, NY 10065; ePathology Core Facility, Memorial Sloan-Kettering Cancer Center, New York, NY 10065; and fJohn C. Whitehead Presidential Fellows Program, The Rockefeller University, New York, NY 10065 Edited by Susan S. Taylor, University of California, San Diego, La Jolla, CA, and approved September 22, 2015 (received for review December 29, 2014) Fibrolamellar hepatocellular carcinoma (FLHCC) tumors all carry a exon of DNAJB1 and all but the first exon of PRKACA. This deletion of ∼400 kb in chromosome 19, resulting in a fusion of the produced a chimeric RNA transcript and a translated chimeric genes for the heat shock protein, DNAJ (Hsp40) homolog, subfam- protein that retains the full catalytic activity of wild-type PKA. ily B, member 1, DNAJB1, and the catalytic subunit of protein ki- This chimeric protein was found in 15 of 15 FLHCC patients nase A, PRKACA. The resulting chimeric transcript produces a (21) in the absence of any other recurrent mutations in the DNA fusion protein that retains kinase activity. -

Synonymous Single Nucleotide Polymorphisms in Human Cytochrome
DMD Fast Forward. Published on February 9, 2009 as doi:10.1124/dmd.108.026047 DMD #26047 TITLE PAGE: A BIOINFORMATICS APPROACH FOR THE PHENOTYPE PREDICTION OF NON- SYNONYMOUS SINGLE NUCLEOTIDE POLYMORPHISMS IN HUMAN CYTOCHROME P450S LIN-LIN WANG, YONG LI, SHU-FENG ZHOU Department of Nutrition and Food Hygiene, School of Public Health, Peking University, Beijing 100191, P. R. China (LL Wang & Y Li) Discipline of Chinese Medicine, School of Health Sciences, RMIT University, Bundoora, Victoria 3083, Australia (LL Wang & SF Zhou). 1 Copyright 2009 by the American Society for Pharmacology and Experimental Therapeutics. DMD #26047 RUNNING TITLE PAGE: a) Running title: Prediction of phenotype of human CYPs. b) Author for correspondence: A/Prof. Shu-Feng Zhou, MD, PhD Discipline of Chinese Medicine, School of Health Sciences, RMIT University, WHO Collaborating Center for Traditional Medicine, Bundoora, Victoria 3083, Australia. Tel: + 61 3 9925 7794; fax: +61 3 9925 7178. Email: [email protected] c) Number of text pages: 21 Number of tables: 10 Number of figures: 2 Number of references: 40 Number of words in Abstract: 249 Number of words in Introduction: 749 Number of words in Discussion: 1459 d) Non-standard abbreviations: CYP, cytochrome P450; nsSNP, non-synonymous single nucleotide polymorphism. 2 DMD #26047 ABSTRACT Non-synonymous single nucleotide polymorphisms (nsSNPs) in coding regions that can lead to amino acid changes may cause alteration of protein function and account for susceptivity to disease. Identification of deleterious nsSNPs from tolerant nsSNPs is important for characterizing the genetic basis of human disease, assessing individual susceptibility to disease, understanding the pathogenesis of disease, identifying molecular targets for drug treatment and conducting individualized pharmacotherapy. -

Colorectal Cancer and Omega Hydroxylases
1 The differential expression of omega-3 and omega-6 fatty acid metabolising enzymes in colorectal cancer and its prognostic significance Abdo Alnabulsi1,2, Rebecca Swan1, Beatriz Cash2, Ayham Alnabulsi2, Graeme I Murray1 1Pathology, School of Medicine, Medical Sciences and Nutrition, University of Aberdeen, Aberdeen, AB25, 2ZD, UK. 2Vertebrate Antibodies, Zoology Building, Tillydrone Avenue, Aberdeen, AB24 2TZ, UK. Address correspondence to: Professor Graeme I Murray Email [email protected] Phone: +44(0)1224 553794 Fax: +44(0)1224 663002 Running title: omega hydroxylases and colorectal cancer 2 Abstract Background: Colorectal cancer is a common malignancy and one of the leading causes of cancer related deaths. The metabolism of omega fatty acids has been implicated in tumour growth and metastasis. Methods: This study has characterised the expression of omega fatty acid metabolising enzymes CYP4A11, CYP4F11, CYP4V2 and CYP4Z1 using monoclonal antibodies we have developed. Immunohistochemistry was performed on a tissue microarray containing 650 primary colorectal cancers, 285 lymph node metastasis and 50 normal colonic mucosa. Results: The differential expression of CYP4A11 and CYP4F11 showed a strong association with survival in both the whole patient cohort (HR=1.203, 95% CI=1.092-1.324, χ2=14.968, p=0.001) and in mismatch repair proficient tumours (HR=1.276, 95% CI=1.095-1.488, χ2=9.988, p=0.007). Multivariate analysis revealed that the differential expression of CYP4A11 and CYP4F11 was independently prognostic in both the whole patient cohort (p = 0.019) and in mismatch repair proficient tumours (p=0.046). Conclusions: A significant and independent association has been identified between overall survival and the differential expression of CYP4A11 and CYP4F11 in the whole patient cohort and in mismatch repair proficient tumours. -
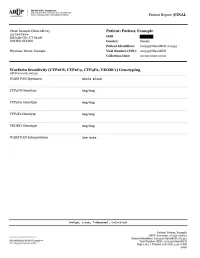
Warfarin Sensitivity (CYP2C8, CYP2C9
Patient Report |FINAL Section 79-1 of New York State Civil Rights Law requires informed consent be obtained from patients (or their legal guardians) prior to pursuing genetic testing. These forms must be kept on file by the ordering physician. Consent forms for genetic testing are available at www.aruplab.com. Incidental findings are not reported unless clinically significant but are available upon request. A Neg result indicates that no variants were detected. All variant alleles are defined based on consensus nomenclature and suggest reduced function of the associated protein(s). CYP2C8 and CYP2C9 are associated with inactivation of warfarin through metabolism. Variant alleles suggest reduced rates of warfarin metabolism, a prolonged time required to achieve steady-state concentrations, and a reduced dose requirement. CYP4F2 is associated with vitamin K recycling. Variant alleles suggest an increased dose requirement. VKORC1 is the therapeutic target for warfarin. Variant alleles suggest increased warfarin sensitivity and a reduced dose requirement. Dosing calculators such as that available through www.WarfarinDosing.org are available to predict loading and therapeutic/maintenance doses. This result has been reviewed and approved by , Ph.D. BACKGROUND INFORMATION: Warfarin Sensitivity (CYP2C8, CYP2C9 , CYP4F2, VKORC1) Genotyping CHARACTERISTICS: Warfarin sensitivity can lead to a life-threatening overdose event such as excessive bleeding. Genetic variation is recognized to explain a large proportion of variability in warfarin dose requirements. This test may predict individual warfarin sensitivity and non-standard dose requirements. The cytochrome P450 (CYP) isozymes 2C8 and 2C9 are involved in the metabolism of many drugs. Variants in the genes that code for CYP2C8 and CYP2C9 may influence pharmacokinetics of substrates such as warfarin, and may predict or explain non-standard dose requirements, therapeutic failure or adverse reactions. -

Comparative Proteomics Analysis of Human Liver Microsomes and S9
DMD Fast Forward. Published on November 7, 2019 as DOI: 10.1124/dmd.119.089235 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 89235 Comparative Proteomics Analysis of Human Liver Microsomes and S9 Fractions Xinwen Wang, Bing He, Jian Shi, Qian Li, and Hao-Jie Zhu Department of Clinical Pharmacy, University of Michigan, Ann Arbor, Michigan (X.W., B.H., J.S., H.-J.Z.); and School of Life Science and Technology, China Pharmaceutical University, Nanjing, Jiangsu, 210009 (Q.L.) Downloaded from dmd.aspetjournals.org at ASPET Journals on October 2, 2021 1 DMD Fast Forward. Published on November 7, 2019 as DOI: 10.1124/dmd.119.089235 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 89235 Running title: Comparative Proteomics of Human Liver Microsomes and S9 Corresponding author: Hao-Jie Zhu Ph.D. Department of Clinical Pharmacy University of Michigan College of Pharmacy 428 Church Street, Room 4565 Downloaded from Ann Arbor, MI 48109-1065 Tel: 734-763-8449, E-mail: [email protected] dmd.aspetjournals.org Number of words in Abstract: 250 at ASPET Journals on October 2, 2021 Number of words in Introduction: 776 Number of words in Discussion: 2304 2 DMD Fast Forward. Published on November 7, 2019 as DOI: 10.1124/dmd.119.089235 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 89235 Non-standard ABBreviations: DMEs, drug metabolism enzymes; HLM, human liver microsomes; HLS9, -

Supplementary Tables, Figures and Other Documents
Clinical Relevance of a 16-Gene Pharmacogenetic Panel Test for Medication Management in a Cohort of 135 Patients David Niedrig1,2, Ali Rahmany1,3, Kai Heib4, Karl-Dietrich Hatz4, Katja Ludin5, Andrea M. Burden3, Markus Béchir6, Andreas Serra7, Stefan Russmann1,3,7,* 1 drugsafety.ch; Zurich, Switzerland 2 Hospital Pharmacy, Clinic Hirslanden Zurich; Zurich Switzerland 3 Swiss Federal Institute of Technology Zurich (ETHZ); Zurich, Switzerland 4 INTLAB AG; Uetikon am See, Switzerland 5 Labor Risch, Molecular Genetics; Berne, Switzerland 6 Center for Internal Medicine, Clinic Hirslanden Aarau; Aarau, Switzerland 7 Institute of Internal Medicine and Nephrology, Clinic Hirslanden Zurich; Zurich, Switzerland * Correspondence: [email protected]; Tel.: +41 (0)44 221 1003 Supplementary Tables, Figures and Other Documents Figure S1: Example of credit-card sized pharmacogenomic profile issued to patients 1 Table S2: SNPs analyzed by the 16-gene panel test Gene Allele rs number ABCB1 Haplotypes 1236-2677- rs1045642 ABCB1 3435 rs1128503 ABCB1 rs2032582 COMT Haplotypes 6269-4633- rs4633 COMT 4818-4680 rs4680 COMT rs4818 COMT rs6269 CYP1A2 *1C rs2069514 CYP1A2 *1F rs762551 CYP1A2 *1K rs12720461 CYP1A2 *7 rs56107638 CYP1A2 *11 rs72547513 CYP2B6 *6 rs3745274 CYP2B6 *18 rs28399499 CYP2C19 *2 rs4244285 CYP2C19 *3 rs4986893 CYP2C19 *4 rs28399504 CYP2C19 *5 rs56337013 CYP2C19 *6 rs72552267 CYP2C19 *7 rs72558186 CYP2C19 *8 rs41291556 CYP2C19 *17 rs12248560 CYP2C9 *2 rs1799853 CYP2C9 *3 rs1057910 CYP2C9 *4 rs56165452 CYP2C9 *5 rs28371686 CYP2C9 *6 rs9332131 CYP2C9 -

Investigation of the Underlying Hub Genes and Molexular Pathogensis in Gastric Cancer by Integrated Bioinformatic Analyses
bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Investigation of the underlying hub genes and molexular pathogensis in gastric cancer by integrated bioinformatic analyses Basavaraj Vastrad1, Chanabasayya Vastrad*2 1. Department of Biochemistry, Basaveshwar College of Pharmacy, Gadag, Karnataka 582103, India. 2. Biostatistics and Bioinformatics, Chanabasava Nilaya, Bharthinagar, Dharwad 580001, Karanataka, India. * Chanabasayya Vastrad [email protected] Ph: +919480073398 Chanabasava Nilaya, Bharthinagar, Dharwad 580001 , Karanataka, India bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract The high mortality rate of gastric cancer (GC) is in part due to the absence of initial disclosure of its biomarkers. The recognition of important genes associated in GC is therefore recommended to advance clinical prognosis, diagnosis and and treatment outcomes. The current investigation used the microarray dataset GSE113255 RNA seq data from the Gene Expression Omnibus database to diagnose differentially expressed genes (DEGs). Pathway and gene ontology enrichment analyses were performed, and a proteinprotein interaction network, modules, target genes - miRNA regulatory network and target genes - TF regulatory network were constructed and analyzed. Finally, validation of hub genes was performed. The 1008 DEGs identified consisted of 505 up regulated genes and 503 down regulated genes. -

Clinical Implications of 20-Hydroxyeicosatetraenoic Acid in the Kidney, Liver, Lung and Brain
1 Review 2 Clinical Implications of 20-Hydroxyeicosatetraenoic 3 Acid in the Kidney, Liver, Lung and Brain: An 4 Emerging Therapeutic Target 5 Osama H. Elshenawy 1, Sherif M. Shoieb 1, Anwar Mohamed 1,2 and Ayman O.S. El-Kadi 1,* 6 1 Faculty of Pharmacy and Pharmaceutical Sciences, University of Alberta, Edmonton T6G 2E1, AB, Canada; 7 [email protected] (O.H.E.); [email protected] (S.M.S.); [email protected] (A.M.) 8 2 Department of Basic Medical Sciences, College of Medicine, Mohammed Bin Rashid University of 9 Medicine and Health Sciences, Dubai, United Arab Emirates 10 * Correspondence: [email protected]; Tel.: 780-492-3071; Fax: 780-492-1217 11 Academic Editor: Kishor M. Wasan 12 Received: 12 January 2017; Accepted: 15 February 2017; Published: 20 February 2017 13 Abstract: Cytochrome P450-mediated metabolism of arachidonic acid (AA) is an important 14 pathway for the formation of eicosanoids. The ω-hydroxylation of AA generates significant levels 15 of 20-hydroxyeicosatetraenoic acid (20-HETE) in various tissues. In the current review, we discussed 16 the role of 20-HETE in the kidney, liver, lung, and brain during physiological and 17 pathophysiological states. Moreover, we discussed the role of 20-HETE in tumor formation, 18 metabolic syndrome and diabetes. In the kidney, 20-HETE is involved in modulation of 19 preglomerular vascular tone and tubular ion transport. Furthermore, 20-HETE is involved in renal 20 ischemia/reperfusion (I/R) injury and polycystic kidney diseases. The role of 20-HETE in the liver is 21 not clearly understood although it represents 50%–75% of liver CYP-dependent AA metabolism, 22 and it is associated with liver cirrhotic ascites. -

Essential Role of the Cytochrome P450 CYP4F22 in the Production of Acylceramide, the Key Lipid for Skin Permeability Barrier Formation
Essential role of the cytochrome P450 CYP4F22 in the production of acylceramide, the key lipid for skin permeability barrier formation Yusuke Ohnoa, Shota Nakamichia, Aya Ohkunia, Nozomi Kamiyamaa, Ayano Naoeb, Hisashi Tsujimurab, Urara Yokoseb, Kazumitsu Sugiurac, Junko Ishikawab, Masashi Akiyamac, and Akio Kiharaa,1 aLaboratory of Biochemistry, Faculty of Pharmaceutical Sciences, Hokkaido University, Kita-ku, Sapporo 060-0812, Japan; bKao Corporation, Haga-gun, Tochigi 321-3497, Japan; and cDepartment of Dermatology, Nagoya University Graduate School of Medicine, Showa-ku, Nagoya 466-8550, Japan Edited by David W. Russell, University of Texas Southwestern Medical Center, Dallas, TX, and approved May 21, 2015 (received for review February 19, 2015) A skin permeability barrier is essential for terrestrial animals, and its lamellae and/or to stabilize the multiple lipid layers. Linoleic impairment causes several cutaneous disorders such as ichthyosis and acid is one of the essential FAs, and its deficiency causes ich- atopic dermatitis. Although acylceramide is an important lipid for the thyosis symptoms resulting from a failure to form normal acyl- skin permeability barrier, details of its production have yet to be de- ceramide (8). Ichthyosis is a cutaneous disorder accompanied termined, leaving the molecular mechanism of skin permeability bar- by dry, thickened, and scaly skin; it is caused by a barrier ab- rier formation unclear. Here we identified the cytochrome P450 gene normality. In patients who have atopic dermatitis, both total CYP4F22 (cytochrome P450, family 4, subfamily F, polypeptide 22) as ceramide levels and the chain length of ceramides are de- the long-sought fatty acid ω-hydroxylase gene required for acylcer- creased, and ceramide composition is altered also (9–11). -

Identification of the Cytochrome P450 Enzymes Responsible for the X
FEBS Letters 580 (2006) 3794–3798 Identification of the cytochrome P450 enzymes responsible for the x-hydroxylation of phytanic acid J.C. Komen, R.J.A. Wanders* Departments of Clinical Chemistry and Pediatrics, Emma Children’s Hospital, Academic Medical Center, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands Received 27 March 2006; revised 26 May 2006; accepted 30 May 2006 Available online 9 June 2006 Edited by Sandro Sonnino tanic acid occurs effectively by bacteria present in the rumen Abstract Patients suffering from Refsum disease have a defect in the a-oxidation pathway which results in the accumulation of of ruminants. phytanic acid in plasma and tissues. Our previous studies have Phytanic acid accumulates in patients with adult Refsum dis- shown that phytanic acid is also a substrate for the x-oxidation ease (ARD, MIM 266500) which is due to a defect in the a-oxi- pathway. With the use of specific inhibitors we now show that dation pathway caused by mutations in one of two genes members of the cytochrome P450 (CYP450) family 4 class are including the PAHX gene which codes for phytanoyl-CoA responsible for phytanic acid x-hydroxylation. Incubations with hydroxylase [2,3], and the PEX7 gene which codes for the microsomes containing human recombinant CYP450s (Super- PTS2 receptor [4]. The majority of ARD patients have muta- TM somes ) revealed that multiple CYP450 enzymes of the family tions in the PAHX gene. The increased levels of phytanic acid 4 class are able to x-hydroxylate phytanic acid with the follow- in plasma and tissues are thought to be the direct cause for the ing order of efficiency: CYP4F3A > CYP4F3B > CYP4F2 > pathology of the disease. -

Cytochrome P450 Expression and Activities in Human Tongue Cells and Their Modulation by Green Tea Extract
Cytochrome P450 expression and activities in human tongue cells and their modulation by green tea extract By: Shin-Pei Yang, and Gregory M. Raner Yang, S.-P. and Raner, G.M. Cytochrome P450 Expression, Induction and Activities in Human Tongue Cells and their Modulation by Green Tea Extract, Toxicol. Appl. Pharmacol. 202, 140-150 (2005). DOI: 10.1016/j.taap.2004.06.014 Made available courtesy of Elsevier: http://www.elsevier.com/wps/find/homepage.cws_home ***Reprinted with permission. No further reproduction is authorized without written permission from Elsevier. This version of the document is not the version of record. Figures and/or pictures may be missing from this format of the document.*** Abstract: The expression, inducibility, and activities of several cytochrome P450 (CYP) enzymes were investigated in a human tongue carcinoma cell model, CAL 27, and compared with the human liver model HepG2 cells. The modulation effects of green tea on various CYP isoforms in both cell lines were also examined. RT-PCR analysis of CAL 27 cells demonstrated constitutive expression of mRNA for CYPs 1A1, 1A2, 2C, 2E1, 2D6, and 4F3. The results were negative for CYP2A6, 2B6/7, 3A3/4, and 3A7. Both cell lines displayed identical expression and induction profiles for all of the isoforms examined in this study except 3A7 and 2B6/7, which were produced constitutively in HepG2 but not Cal-27 cells. CYP1A1 and 1A2 were both induced by treatment with β-napthoflavone as indicated by RT-PCR and Western blotting, while CYP2C mRNA was upregulated by all-trans retinoic acid and farnesol.