Henry Ford Health System Scholarly Commons
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Relics of the Bulgarian National Epic
PAISStt OF HILENDAR: FOUNDER OF THE NATIONAL IDEOLOGY In modern historiography the first centuries of the of the respectful image of Mediaeval Bulgaria. In Sremski Ottoman rule of Bulgarian lands are determined as Late Karlovci, one of the most active literary centres of the Middle Ages. The time from the beginning of the 18th time, Paissi read the book of Dubrovnik Abbot Mavro century to the 1877-1878 Russo-Turkish War is called Orbini "The Realm of the Slavs" in which he discovered Bulgarian National Revival. If the National Revival period considerable evidence about the Bulgarians' past. for Northern Bulgaria and the Sofia Region continued by In 1762 he completed "Slav-Bulgarian History, about 1878, for Eastern Rumelia it was by 1885 and for the People and the Kings, the Bulgarian Saints and All Macedonia and Adrianople Thrace by 1912-1913. Bulgarian Activities and Events". In 83 hand-written The National Revival in the Bulgarian lands witnessed pages the inspired Hilendar Monk interpreted using considerable economic progress. The Bulgarian were romantic and heightened tone the grandour of increasingly getting rid of their mediaeval restricted out- Mediaeval Bulgaria, the victory of the Bulgarian army look and helplessness and were gradually getting aware over Byzantium, the impressive bravery and manliness of as people, aspiring towards economic and cultural the Bulgarians, the historic mission of the Cyril and progress. Hilendar monk Paissii became a mouthpiece of Methodius brothers and other eloquent facts, worthy to these changes in the national self-awareness. He was be remembers and respected by the successors. Already the first to perceive the beginning of the new time and in the forward this noted Bulgarian appealed with gen- the need of formulating verbally the maturing historical uine sincerity towards his compatriots to love and keep prospects and tasks before the Bulgarian people. -

Abstracts from the 50Th European Society of Human Genetics Conference: Electronic Posters
European Journal of Human Genetics (2019) 26:820–1023 https://doi.org/10.1038/s41431-018-0248-6 ABSTRACT Abstracts from the 50th European Society of Human Genetics Conference: Electronic Posters Copenhagen, Denmark, May 27–30, 2017 Published online: 1 October 2018 © European Society of Human Genetics 2018 The ESHG 2017 marks the 50th Anniversary of the first ESHG Conference which took place in Copenhagen in 1967. Additional information about the event may be found on the conference website: https://2017.eshg.org/ Sponsorship: Publication of this supplement is sponsored by the European Society of Human Genetics. All authors were asked to address any potential bias in their abstract and to declare any competing financial interests. These disclosures are listed at the end of each abstract. Contributions of up to EUR 10 000 (ten thousand euros, or equivalent value in kind) per year per company are considered "modest". Contributions above EUR 10 000 per year are considered "significant". 1234567890();,: 1234567890();,: E-P01 Reproductive Genetics/Prenatal and fetal echocardiography. The molecular karyotyping Genetics revealed a gain in 8p11.22-p23.1 region with a size of 27.2 Mb containing 122 OMIM gene and a loss in 8p23.1- E-P01.02 p23.3 region with a size of 6.8 Mb containing 15 OMIM Prenatal diagnosis in a case of 8p inverted gene. The findings were correlated with 8p inverted dupli- duplication deletion syndrome cation deletion syndrome. Conclusion: Our study empha- sizes the importance of using additional molecular O¨. Kırbıyık, K. M. Erdog˘an, O¨.O¨zer Kaya, B. O¨zyılmaz, cytogenetic methods in clinical follow-up of complex Y. -
Annual Report 2003–2004
he Institute was founded in 1963 by Hellmut Becker, who was joined subsequently by Friedrich Edding (1964), Dietrich Goldschmidt (1964), and Saul B. Robinsohn (1964) as the first generation of scientific directors and senior fellows of the Max Planck Society. In the first decade of its existence, the development of educational research Research Report Research Report and educational policy was emphasized. 2003–2004 2003–2004 The appointment of a second generation of directors Research Report 2003-2004 (Wolfgang Edelstein, 1973, and Peter M. Roeder, he Max Planck Institute for Human Develop- 1973) added to this framework a commitment to ment, founded in 1963, is a multidisciplinary basic research in human development and research establishment dedicated to the study of educational processes. Primary emphases included human development and education. Its inquiries longitudinal research on child and adolescent are broadly defined, but concentrate on the development (Edelstein) and educational research on Center for Adaptive Behavior and Cognition evolu-tionary, social, historical, and institutional (Director: Gerd Gigerenzer) classroom processes and school organization contexts of human development, as well as (Roeder). examining it from life-span and life-course perspectives. The disciplines of education, Since the 1980s and with the appointment of a third Center for Educational Research (Director: Jürgen Baumert) psychology, and sociology reflect the current generation of senior fellows and scientific directors directors’ backgrounds, but the Institute’s (Paul B. Baltes, 1980; Karl Ulrich Mayer, 1983; scholarly spectrum is enriched by the work of Jürgen Baumert, 1996; Gerd Gigerenzer, 1997), colleagues from such fields as mathematics, research at Center for Sociology and the Study of the Life Course (Director: Karl Ulrich Mayer) economics, computer science, evolutionary the Institute has concentrated more and more on biology, and the humanities. -

ITGBL Local Agents
ITGBL Local Agents Country: Afghanistan Post: Kabul Bureau: SCA Local Agents: 2) AES Cargo Share-E-Naw, Charahi Ansari Kabul, Afghanistan POC: Greg Forgrave Tel: 93-70-296-492 Cell: 93-70-274-374 Email: [email protected] 1) PAXTON International House #1, Corner of Shura and Park Streets Karte Seh Kabul, Afghanistan POC: Wali Mohammad Wasif Tel: 93 (0) 70 295 329 Cell: 0093 (0) 700 29 53 29 Email: [email protected] Website: www.paxton.com Country: Albania Post: Tirana Bureau: EUR Local Agents: 1) AES Cargo/ Move One Rruga "Brigada e VIII" P. Teknoprojekt Sh.2 Ap 3/2 Nr. 33/1 Tirana, Albania POC: Glenda Pajo Tel: 355 4 225 8103 Cell: 355 69 206 7269 Email: [email protected] 2) AGS Tirana Ish Kombinati I Tekstileve Fabrika e Ngyrosjes Tirana, Albania POC: Genti Jacellari Tel: 355 4 235 2560 x113 Fax: 355 69 208 6315 Email: [email protected] Wednesday, July 21, 2010 Page 1 of 152 ITGBL Local Agents Country: Algeria Post: Algiers Bureau: NEA Local Agents: 2) Algeria Moving and Shipping 13 Lot Beau Sejour La Sapiniere No. 7 Birmandreis Algers, Algeria POC: Mme. Ahlem Menar, GM Tel/Fax: 213-21-56-48-53 Cell: 213-0770-415-261 1) Deminter Algeria Rue Lakhder Manaa Cite 19 & 2 BT C No. 1 Ben Aknoon Alger, Algerie POC: Mr. Mohamed Meghiref, GM Tel: 213-21-91-57-92/ 213-21-91-57-94 Fax: 213-21-91-67-62/ 213-21-91-24-82 Cell: 213-61-51-27-38 Madjid Meghiref Cell: 213- 550 614 494 Amine Meghiref Email: [email protected] Country: Angola Post: Luanda Bureau: AF Local Agents: 1) EMP-TRANS Cargo Center Lds. -

“To Get Rid of Turks”. the South-Slavic States and Muslim Remigration in the Turn of 1870S and 1880S1
“TO GET RID OF TURKS”. THE SOUTH-SLAVIC STATES AND MUSLIM REMIGRATION IN THE TURN OF 1870S AND 1880S1 Krzysztof Popek Jagiellonian University in Kraków, Institute of History ORCID ID: 0000-0001-5864-5264 Introduction The Great Eastern Crisis (1875–1878) led to migrations on an in- comparable scale in the Balkan Peninsula. The Russian-Turkish War of 1877–1878 forced about 350,000 Muslims to leave the Bulgarian lands, which we will understand as the area covering the Principality of Bulgaria and Eastern Rumelia. Sanjak of Niš’s occupation by the Serbian Army resulted in the exodus of 71,000 Muslims. After the situation in the region had stabilized, the refugees (so-called Muhajirs) wanted to get back to their homes in the newly created Principality of Bulgaria, autonomous Eastern Rumelia (first controlled by Russians and later by Bulgarians), and the lands annexed by Serbia. The return of war refugees was one of the central problems the South-Slavic states faced in the first years after the Great Eastern Cri- sis. It led to serious complications, which had various reasons. Among the most significant ones was the logistic deployment of the remigrants in the areas often settled by Bulgarians of Macedonia and Thrace, and by Serbians of Kosovo and Montenegro. Another one was diplomatic disputes between the Sublime Porte and the Great Powers, the latter 1 ����������������������������������������������������������������������������������������Research presented in this article was financed by the grant of the Polish National Sci- ence Center: The Balkan Migration Processes in the 19th Century. Cases of Bulgaria and Serbia (2017/25/N/HS3/00576). -

LEONARDO PROJECT – English Summary the Project Main Goal Is
Project national LLP-LdV/PAR/2011/RO//129 number Project title “Introducing standards of the best medical practice for the patients with inherited Alpha-1 Antitrypsin Deficiency in Central Eastern Europe” LEONARDO PROJECT – english summary The project main goal is to support development of Central Eastern European Network (CEE) for Alpha-1 Antytrypsin Deficiency (A1ATD) diagnostics and treatment that will function within AIR (Alpha One International Registry) European network of medical centers specializing in A1ATD. Parteners 1. The National Institute of Tuberculosis and Lung Diseases/ Poland (Coordinator) 2. Hannover Medical School/ Germany 3. Institute of Pneumophtysiology “Marius Nasta”/ Romania 4. PJ Safarik University, Faculty of Medicine/ Slovakia 5. Leiden University Medical Center h/o Academisch Ziekenhuis Leiden/ Netherlands 6. UMHAT “Dr.Georgi Stranski” Pleven EAD, Clinic for pneumonology and phthisiatry"/ Bulgaria 7. Vilnius University Faculty of Medicine/ Lithuania 8. Università degli Studi di Pavia/ Italy The project is designed to address specific CEE regional educational needs, therefore its aims are: • to develop individualized training program for respiratory professionals : physicians, physiotherapists, laboratory staff involved in A1ATD diagnostics and medical care in CEE; program will be tailored according to specific country needs • to develop educational materials for respiratory professionals in national CEE languages • to create awareness of A1ATD problem and patient needs in CEE • to promote A1ATD European network in CEE European countries Project Stages: Stage 1: Central Eastern European Network establishment: assessing local needs and potential to launch close cooperation both regionally as well as within the existing European network (AIR)- workshop Stage 2A: Training visits Stage 2B: Focus group workshops Stage 3A: European network AIR conference in Warsaw Stage 3B: Educational materials for respiratory professionals and dissemination of results . -
L Shire 2020 Disclosure Report ENG 21 June.Xlsx
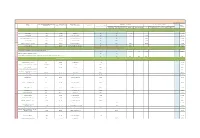
Date of publication: 2021-06-21 HCPs: City of Principal Practice HCOs: city Unique country identifier Full Name Country of Principal Practice Principal Practice Address Contribution to costs of Events Fee for service and consultancy where registered OPTIONAL TOTAL Donations and Grants to HCOs Sponsorship agreements with HCOs / third parties Related expenses agreed in the fee for service or consultancy contract, OPTIONAL Registration Fees Travel & Accomodation Fees appointed by HCOs to manage an Event including travel & accomodation relevant to the contract INDIVIDUAL NAMED DISCLOSURE - one line per HCP (i.e. all transfers of value during a year for an individual HCP will be summed up: itemization should be available for the individual Recipient or public authorities' consultation only, as appropriate) Atanas Banchev Sofia Bulgaria Byalo More 8 N/A N/A 1,706.00 1,706.00 Анна Валериева София Bulgaria ул.Св.Георги Софийски 1 N/A N/A 176.02 5,307.00 5,483.02 Даниела Мирчева Авджиева Тзавелла София Bulgaria ул.Свето Преображение 20 N/A N/A 1,024.00 1,024.00 Емил Паскалев София Bulgaria ул.Св.Георги Софийски 1 N/A N/A 1,173.00 1,173.00 HCPs Мария Тончева Стаевска Коташева София Bulgaria ул.Св.Георги Софийски 1 N/A N/A 176.02 1,227.00 1,403.02 Мила Жекова Байчева София Bulgaria бул.Акад.Иван Евстратиев Гешов 11 N/A N/A 352.05 352.05 OTHER, NOT INCLUDED ABOVE - where information cannot be disclosed on an individual basis for legal reasons Aggregate amount attributable to transfers of value to such Recipients - Art. -

Investbulgaria Agency
InvestBulgaria Agency June 2014 InvestBulgaria Agency issue 6 (9), year 2 Economic News - Business, Investments, Trade Headlines from the European institutions Analysis of Sector Monthly Investment Opportunities of Municipality Electronic Publication Interview Chambers of Commerce in Bulgaria Macroeconomic Indicators Upcoming Events INVESTBULGARIA AGENCY TODAY WE PRESENT: Bulgarian Small and Medium Enterprises Promotion Agency Evgeni Ivanov Executive Director of the Bulgarian Small and Medium Enterprises Promotion Agency (BSMEPA) He graduated from the Technical University of Sofia, Electrical machines and apparatus. He has two Master's degrees - Economics, organization and management of patent law and licensing activity and Complex social and economic development of the urban economy. He is fluent in English and Russian. In his professional career he held the posts of Executive Director of Astera Jsc, Astera Holding Jsc, Sinel Jsc, Chairman of the Board of Directors of Aroma Jsc, member of the Management Board and the Supervisory Board of Aroma Jsc, member of the Commission for Protection of Competition. He was a Member of the 40th National Assembly, where he was a member of the Budget and Finance committee and Economic Policy committee. Until him taking the seat as CEO of BSMEPA, Evgeni Ivanov was Chairman of BNAEOPC (Bulgarian National Association Essential Oils, Perfumery and Cosmetics), board member of EcoBulpack and board member of the Union Made in Bulgaria. Small and Medium Enterprises Promotion Agency is an administrative structure of the Ministry of Economy and Energy and as such it implements the state policy to promote entrepreneurship development and internationalization of SMEs. The Agency is transmission between the state and small and medium-sized companies. -

Conference Abstracts
A Century of Lifesaving - a Challenge to Drowning Prevention Conference Abstracts www.wcdp2013.org 1 ALLE Raumplaene 02_13_A4 02.10.13 11:54 Seite 6 Funktionale An der Pirschheide · 14471 Potsdam Tel. (0331) 9090-0 · Fax (0331) 9090-900 Seminar- und [email protected] · www.seminaris.de Tagungsräume ERDGESCHOSS STC: Seminar, Trainings & Office Center 13 PBA: Plenar- & Bankett Areal EG 14 15 ECC: Executive-Conference-Center 16 17 12 11 Foyers 10 9 Office Center 8 STC Office 7 5 Office 4 6 Eingang »Brandenburg« Office 3 5 Pantry Office »Berlin« 1 Office 2 19 18 »Havel« 4 »Spree« ECC 3 2 “Wellness Area »Potsfit« 1 Reception Eingang “Bar »Captains Corner« PBA »Café Cecile« I “Restaurant STC = Seminar & »feines Brandenburger« Training Center II SeeTerrasse ECC = Executive III Conference Regie Center PBA = Plenary & “Restaurant Banquet Area »Templiners« Forewords ALLE Raumplaene 02_13_A4 02.10.13 11:54 Seite 6 Funktionale An der Pirschheide · 14471 Potsdam Foreword Tel. (0331) 9090-0 · Fax (0331) 9090-900 Seminar- und [email protected] · www.seminaris.de Tagungsräume On behalf of the International Life Saving Federation it gives me great pleasure to welcome all of the participants to the World Conference on Drowning Prevention 2013, in Potsdam Germany. ERDGESCHOSS The International Life Saving Federation (ILS) is the World STC: Seminar, Trainings & Office Center authority on drowning prevention, lifesaving and lifesaving 13 sport. ILS leads, supports and collaborates with national and PBA: Plenar- & Bankett Areal EG 14 international organisations engaged in drowning prevention, 15 ECC: Executive-Conference-Center 16 water safety, water rescue, lifesaving, lifeguarding and lifesa- 17 12 11 ving sport. -

Klaus Herlitz
| PERSÖNLICHKEITEN BERLIN-MACHER DASS BERLIN DAZU VERDAMMT IST, IMMERFORT ZU WERDEN UND NIEMALS ZU SEIN, WUSSTE SCHON IM JAHR 1910 DER PUBLIZIST UND KUNSTKRITIKER KARL SCHEFFLER. EIN OFT ZITIERTER SATZ, DER NOCH HEUTE GILT. UMSO MEHR SIND MENSCHEN GEFRAGT, DIE VOR ODER HINTER DEN KULISSEN ETwaS BEWEGEN UND DIE STADT EIN STÜCK VORANBRINGEN. WIR STELLEN SIE IN JEDER AUSGABE VOR, DIE BERLIN-MACHER. DIESMAL KLAUS HERLITZ. Foto: Buddy Bär Berlin Klaus und Eva Herlitz sind die Erfinder der Buddy Bären Der Bär ist das Wappentier Berlins und motto, mit dem er das Familienunter- Jahren auch getan. Über zwei Millio- angeführt von Klaus und Eva Herlitz, Denn ohne sie wären die Bären nicht unter dem gleichen Motto wie ihre der wohl bekannteste Markenbotschaf- nehmen in der Papier-, Büro- und nen Euro hat die Buddy Bär Berlin seinen Siegeszug um die Welt fort- auch noch ein Verkaufsschlager. großen Vorbilder für ein friedliches ter der deutschen Hauptstadt. Dazu Schreibwarenbranche national wie in- GmbH mit Versteigerungen und di- setzt. 30 Ausstellungen weltweit hat Bevor der erste Prototyp im April 2001 Mit- und Nebeneinander unter den 42 ganz wesentlich beigetragen hat der ternational etablierte und im Jahres- versen Aktivitäten als Gesamterlös er- es bislang schon gegeben, „auf allen überhaupt gezeigt werden konnte, wa- Völkern: „Wir müssen uns besser ken- 43 Buddy Bär, der im Jahr 2001 das Licht rhythmus neue Produkte auf den Markt wirtschaftet, die dann Kinderorganisa- Kontinenten“, wie der unermüdliche ren bereits die ersten 60 Zwei-Meter- nenlernen, dann können wir uns bes- der Welt erblickte. Seine Eltern sozu- brachte. Vor allem im Bereich Umwelt- tionen wie Unicef, SOS Kinderdorf, Bärenanführer betont. -

Convert Finding Aid To
Morris Leopold Ernst: An Inventory of His Papers at the Harry Ransom Center Descriptive Summary Creator: Ernst, Morris Leopold, 1888-1976 Title: Morris Leopold Ernst Papers Dates: 1904-2000, undated Extent: 590 boxes (260.93 linear feet), 47 galley folders (gf), 30 oversize folders (osf) Abstract: The career and personal life of American attorney and author Morris L. Ernst are documented from 1904 to 2000 through correspondence and memoranda; research materials and notes; minutes, reports, briefs, and other legal documents; handwritten and typed manuscripts; galley proofs; clippings; scrapbooks; audio recordings; photographs; and ephemera. The papers chiefly reflect the variety of issues Ernst dealt with professionally, notably regarding literary censorship and obscenity, but also civil liberties and free speech; privacy; birth control; unions and organized labor; copyright, libel, and slander; big business and monopolies; postal rates; literacy; and many other topics. Call Number: Manuscript Collection MS-1331 Language: English Note: The Ransom Center gratefully acknowledges the assistance of the National Endowment for the Humanities, which provided funds for the preservation and cataloging of this collection. Access: Open for research Administrative Information Acquisition: Gifts and purchases, 1961-2010 (R549, R1916, R1917, R1918, R1919, R1920, R3287, R6041, G1431, 09-06-0006-G, 10-10-0008-G) Processed by: Nicole Davis, Elizabeth Garver, Jennifer Hecker, and Alex Jasinski, with assistance from Kelsey Handler and Molly Odintz, 2009-2012 Repository: The University of Texas at Austin, Harry Ransom Center Ernst, Morris Leopold, 1888-1976 Manuscript Collection MS-1331 Biographical Sketch One of the most influential civil liberties lawyers of the twentieth century, Morris Ernst championed cases that expanded Americans' rights to privacy and freedom from censorship. -

Summary INTERNAL DISEASES PLENARY LECTURE Summary
Abstracts from Jubilee Scientific Conference “45 years Medical University – Pleven”, 31 Oct - 2 Nov, 2019 1Institute of Metal Science, Equipment INTERNAL DISEASES and Technologies with Hydro- and Aerodynamics Centrе, PLENARY LECTURE Bulgarian Academy of Sciences, Sofia, Bulgaria CARDIAC SARCOIDOSIS – A NOT SO Corresponding Author: RARE TYPE OF CARDIOMYOPATHY Stefan Valkov Institute of Electronics, WITH RHYTHM DISTURBANCES Bulgarian Academy of Sciences 72, Tsarigradsko Chaussee Blvd. Borislav B. Dinov Sofia, 1784 Bulgaria Heart Center University of Leipzig, e-mail: [email protected] Germany Summary Corresponding Author: Due to the combination of attractive mechanical Borislav B. Dinov properties, biocompatibility and resistance to Heart Center University of Leipzig corrosion, the Co-Cr based alloys are widely Strümpellstraße 39 used for manufacturing of dental joints, implants 04289 Leipzig Germany and other medical devices. However, some e-mail: [email protected] drawbacks related to low hardness and wear resistance can be mentioned. These limitations Summary depend mostly on the surface properties and Cardiac involvement can occur in patients can be overcome by an appropriate technology with pulmonary or systemic sarcoidosis with for surface manufacturing. In recent years, the varying symptoms and severity. It can mimic deposition of coatings has been widely used for virtually every type of cardiomyopathy and is improving the properties of the materials. There therefore frequently misdiagnosed. Even more exist some technologies for depositing thin challenging are the cases of isolated cardiac films and coatings, including physical vapour sarcoidosis which are considered rare, often deposition (PVD), chemical vapour deposition remain unrecognized and have grave prognosis if (CVD), among others. The direct current (DC) left untreated with immunosuppressive therapy.