Journée Municipale Nationale
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
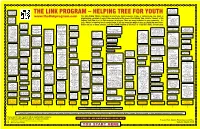
LINK Ptogram Decisional Tree English
School based Free legal advice programs / groups: clinic: Call Chimo Health action groups, 450-HELP (4357) THE LINK PROGRAM – HELPING TREE FOR YOUTH Teen mom groups, etc. or 1-800-667-5005 www.thelinkprogram.com This HELPING TREE is designed to inform you about resources. If you, or someone you care about, is Helplines: School based u Chimo 450-HELP (4357) programs/groups: experiencing a problem in any of the areas listed at the base of the Helping Tree, follow a "branch" of the or 1-800-667-5005 Antibullying, Peer Helping Tree (flow chart) to find resources to help you. There are many resources in your community – it's u Kids Help Phone Helpers, Making 1-800-668-6868 Waves, etc just a matter of knowing how to contact them. If you are uncertain where to turn, or would like more infor- www.kidshelpphone.ca u Telecare 811 Frontier College mation on any of these services, call the CHIMO Helpline at 450-4357 or 1-800-667-5005, 24 hours/day. (Talk to a nurse) (tutoring) Helplines: 450-7923 or School based Employment services/ Q Centre Commun- u Chimo programs/groups: programs for special 1-877-450-7923 autaire Sainte-Anne Helplines: 450-HELP (4357) or specific needs: 453-2731 Birthright 1-800-550-4900 School based Teens Against Tobacco u Chimo 450-HELP (4357) Other local services for grief: programs/groups: or 1-800-667-5005 Use (TATU) u Premier's Council on or 454-1890 u Other services to meet or 1-800-667-5005 Local churches & organizations Clubs, Peer helpers, Sports, Kids Help Phone the Status of Disabled u Sylvan Learning Teens Against Drinking basic needs: Kids Help Phone 1-800-668-6868 Helplines: Support Groups such as Youth Engagement, etc 1-800-668-6868 Persons 444-3000 or Q 1-866-363-6546 & Driving (TADD) Federation des Courthouses: www.kidshelpphone.ca u GriefShare, youth groups, etc. -

DYCD Sites for 8.12
DYCD Sites Operating BCO District 8/12 Address Zip Code Site Type team XFSC 7 X001 335 EAST 152 STREET 10451 DYCD Only Team 1 Bronx XFSC 7 X025 811 EAST 149 STREET 10455 DYCD Only Team 1 Bronx XFSC 10 X033 2424 JEROME AVENUE 10468 DYCD Only Team 1 Bronx XFSC 11 X041 3352 OLINVILLE AVENUE 10467 DYCD Only Team 1 Bronx XFSC 8 X048 1290 SPOFFORD AVENUE 10474 DYCD Only Team 1 Bronx XFSC 9 X058 459 EAST 176 STREET 10457 DYCD Only Team 1 Bronx XFSC 8 X071 3040 ROBERTS AVENUE 10461 DYCD Only Team 1 Bronx XFSC; Charter 8 X093 1535 STORY AVENUE 10473 DYCD Only Team 1 Bronx XFSC 10 X094 3530 KINGS COLLEGE PLACE 10467 DYCD Only Team 1 Bronx XFSC 11 X096 2385 OLINVILLE AVENUE 10467 DYCD Only Team 1 Bronx XFSC 11 X097 1375 MACE AVENUE 10469 DYCD Only Team 1 Bronx XFSC 8 X100 800 TAYLOR AVENUE 10473 DYCD Only Team 1 Bronx XFSC 9 X104 1449 SHAKESPEARE AVENUE 10452 DYCD Only Team 1 Bronx XFSC 11 X106 1514 OLMSTEAD AVENUE 10462 DYCD Only Team 1 Bronx XFSC 8 X107 1695 SEWARD AVENUE 10473 DYCD Only Team 1 Bronx XFSC 11 X121 2750 THROOP AVENUE 10469 DYCD Only Team 1 Bronx XFSC 9 X126 175 WEST 166 STREET 10452 DYCD Only Team 1 Bronx XFSC 8 X130 750 PROSPECT AVENUE 10455 DYCD Only Team 1 Bronx XFSC 12 X134 1330 BRISTOW STREET 10459 DYCD Only Team 1 Bronx XFSC 8 X140 916 EAGLE AVENUE 10456 DYCD Only Team 1 Bronx XFSC 12 X167 1970 WEST FARMS ROAD 10460 DYCD Only Team 1 Bronx XFSC 10 X206 2280 AQUEDUCT AVENUE 10468 DYCD Only Team 1 Bronx XFSC 10 X279 2100 WALTON AVENUE 10453 DYCD Only Team 1 Bronx XFSC 10 X843 2641 GRAND CONCOURSE 10468 DYCD Only Team 1 Bronx -

PO T of the CHIEF CTORAL O FCER DES ELECTIO
THIRTY-FIRST GENERAL EL£CTION OCTOBER 13. 1987 PO T OF THE CHIEF CTORAL o FCER PROVINCE OF NEW BRUNSWICK DES ELECTIO DU WIC SUR LE TRENTE ET UNIEMES ELECTIONS GENERALES TENUES LE 13 OCTOBRE 1987 TO THE LEGISLATIVE ASSEMBLY OF NEW BRUNSWICK MR. SPEAKER: I have the honour to submit to you the Return of the General Election held on October 13th, 1987. The Thirtieth Legislative Assembly was dissolved on August 29th, 1987 and Writs ordering a General Election for October 13th, 1987 were issued on August 29th, 1987, and made returnable on October 26th, 1987. Four By-Elections have been held since the General Election of 1982 and have been submitted under separate cover, plus being listed in this Report. This Office is proposing that consideration be given to having the Chief Electoral Officer and his or her staff come under the Legislature or a Committee appointed by the Legislature made up of all Parties represented in the House. The other proposal being that a specific period of time be attached to the appointments of Returning Officers as found in Section 9 of the Elections Act. Respectfully submitted, February 15, 1988 SCOVIL S. HOYT Acting Chief Electoral Officer A L'ASSEMBLEE LEGISLATIVE DU NOUVEAU-BRUNSWICK MONSIEUR LE PRESIDENT, J'ai I'honneur de vous presenter les resultats des elections generales qui se sont tenues Ie 13 octobre 1987. La trentieme Assemblee legislative a ete dissoute Ie 29 Staff of Chief Elec aoOt 1987 et les brefs ordonnant la tenue d'elections Personnel du bUrE generales Ie 13 octobre 1987 ont ete em is Ie 29 aout 1987 et Election Schedule rapportes Ie 260ctobre 1987. -
2018 Annual Report
Board of Directors The New York Cares Board of Directors are dedicated professionals who bring a wealth of public and private sector experience and are committed to driving community impact through volunteerism. President Board Members Paul J. Taubman James L. Amine, Head of Private Credit Chairman and CEO, PJT Partners Opportunities, Credit Suisse Rene Brinkley, Brand Marketing Manager, CNBC 2018 Vice President Audrey Choi, Chief Marketing Officer and Chief Kathy Behrens Sustainability Officer, Morgan Stanley Annual President, Social Responsibility and Player K. Don Cornwell, Partner, PJT Partners Programs, National Basketball Association Joyce Frost, Partner, Riverside Risk Advisors LLC Report Vice President Gail B. Harris, President Emeritus, John B. Ehrenkranz Board Director and Investor Chief Investment Officer, Julie Turaj Ehrenkranz Partners L.P. Robert Walsh, Chief Financial Officer, Evercore Partners Janet Zagorin, Principal, Opal Strategy LLC Vice President Adam Zotkow, Partner, Goldman Sachs Michael Graham Senior Managing Director & Country Honorary Board Members Head - USA, OMERS Private Equity USA Edward Adler, Partner, RLM Finsbury Richard Bilotti, Head of Technology, Media, Secretary and Telecommunications Research, Keith A. Grossman P. Schoenfeld Asset Management President, TIME Cheryl Cohen Effron Ken Giddon, President, Rothman’s We Co-Treasurer Union Square Neil K. Dhar Partner, Head of Financial Services, Sheldon Hirshon, ESQ, SIH PriceWaterhouseCoopers LLP Enterprises, a Division of MC Acquisitions LLC Co-Treasurer Robert Levitan, Chief Executive Jeanne Straus Officer, Pando Networks, Inc. President, Straus News, Our Town, West David Rabin, Partner, The Lambs Side Spirit, Our Town Downtown Club and Double Seven Michael Schlein, President and believe CEO, Accion International Rising Leaders Council The Rising Leaders Council is a group of 40 young professionals who spearhead volunteer projects and raise funds in support of New York Cares. -

Fredericton and Upper River Valley | Community Resources
PAGE 1 OF 6 NBBWCP | NEW BRUNSWICK BREAST & WOMEN'S CANCER PARTNERSHIP Fredericton and Upper River Valley | Community Resources SERVICE LOCATION CONTACT BREAST CANCER The program encourages women between the ages of 50-74 to SCREENING be screened every two years at one of the 16 mammography sites across the province. Women residing in NB who are 50 - 74 years of age and have no signs, symptoms or previous diagnosis of breast cancer can self- refer to breast cancer screening by contacting one of the screening sites. Women aged 40-49 or over 74 who have no signs, symptoms or previous diagnosis of breast cancer require a referral from a primary health-care provider. Breast cancer screening services are offered at a number of facilities: Breast Cancer Screening Perth-Andover Program Local: 506-273-7181 Hospital Hotel-Dieu of St. Joseph Breast Cancer Screening Waterville Program Toll free: 1-800-656-7575 Upper River Valley Hospital Breast Cancer Screening Oromocto Program, Local: 506-357-4747 Oromocto Public Hospital www.nbbwcp-pcscfnb.ca [email protected] November 01, 2018 10:14:20 AM AST PAGE 2 OF 6 NBBWCP | NEW BRUNSWICK BREAST & WOMEN'S CANCER PARTNERSHIP SERVICE LOCATION CONTACT CERVICAL CANCER Who can access this program? SCREENING Screening for cervical cancer using Pap tests are recommended for NB women aged 21-69 who have ever been sexually active with a partner of either gender: - Even after menopause (no longer having periods) - Even after having the HPV vaccine. Contact your primary health-care provider to discuss cervical cancer screening. Boiestown Health Centre Boiestown Local: 506-369-2700 Brunswick Community Health Fredericton Clinic Local: 506-452-6383 Central Miramichi Community Doaktown Health Centre Local: 506-365-6100 CFB Gagetown Medical Clinic Gagetown, Oromocto Local: 506-422-2000 #3270 Fredericton Junction Health Fredericton Junction Centre Local: 506-368-6501 Harvey Health Centre Harvey Local: 506-366-6400 Hotel Dieu St. -

Her Excellency, the Right Honourable Adrienne Clarkson, Governor General and Commander-In-Chief of Canada
Minister of Health Ministre de la Santé The Honourable/L'honorable Pierre S. Pettigrew Ottawa, Canada K1A 0K9 December, 2003 Her Excellency, the Right Honourable Adrienne Clarkson, Governor General and Commander-in-Chief of Canada May it please Your Excellency: The undersigned has the honour to present to Your Excellency the Annual Report on the administration and operation of the Canada Health Act for the fiscal year that ended March 31, 2003. Pierre S. Pettigrew Preface The late Justice Emmett M. Hall referred to Canada’s Medicare with the words: “Our proudest achievement in the well-being of Canadians has been in asserting that illness is burden enough in itself. Financial ruin must not compound it. That is why Medicare has been called a sacred trust and we must not allow that trust to be betrayed.” The adoption of the Canada Health Act is an important achievement in the evolution of Canada’s health care system. The Act puts into words our commitment to a universal, publicly funded health care system based on the needs of Canadians, not their ability to pay. The five principles of the Act are the cornerstone of the Canadian health care system, and they reflect the values that inspired our system. April 1, 2004, will mark the 20th anniversary of the Act. In 2003, the provincial premiers and territorial leaders reached a historic agreement with Canada’s former Prime Minister, the Right Honourable Jean Chrétien, to improve the quality, accessibility and sustainability of our public health care system. On this occasion, the first ministers reaffirmed their commitment to the five principles of public health insurance in Canada: universality, accessibility, portability, comprehensiveness and public administration. -
![Celebrate National Nursing Week NANB’S NNW Poster Competition [10]](https://docslib.b-cdn.net/cover/3931/celebrate-national-nursing-week-nanb-s-nnw-poster-competition-10-2453931.webp)
Celebrate National Nursing Week NANB’S NNW Poster Competition [10]
infoVolume 42 Issue 1 sprIng 2011 nursing Celebrate National Nursing Week NANB’s NNW Poster Competition [10] ELECTION 2011: MEET THE NANB’S 95TH AGM & RESOLUTIONS TO THE 2011 CANDIDATES [14] CONFERENCE [24] NANB AGM [23] spring 2011 InsIde NANB’s 95th AGM & Conference Juin 8 & 9, 2011 André Picard Dr. Judith Dr. Patricia 24 Ritchie Rodney 14 Meet the Candidates: NANB 26 Proxy Voting: What You Need Election 2011 to Know Cover Participate in NANB’s 2011 poster competition to celebrate National Nursing Week: May 9–15. See details on page 10. 30 Passing the Canadian 37 Meet the Voice on the Other Registered Nurse Examination End of the Phone 2 INFO NURSING SPRING 2011 20 32 10 NANB’s NNW Poster Competition 21 Medication Orders by Telephone Celebrating National Nursing Week By Shauna Figler 13 RN Acquiring Conflict Resolution Skills 29 Are NPs Authorized to Prescribe ‘Off Label’? The College of Extended Learning at UNB By Susanne Priest Offers Program By Leah Prosser 29 MOMS Link Study Sustainable Telephone-Based Support for Mothers 16 Audit Results with Postpartum Depression Continuing Competence Program By Sarah MacLaggan 19 Working Collaboratively 33 Health Centres in New Brunswick: RNs & Registered Midwives Leaders in the Provision of Primary Health Care By Shauna Figler By Joanne Barry & Cheryl Saunders 20 Local Author Captures a Piece of 35 UNBSJ Delivers Bachelor of Nursing Degree Nursing History for Registered Nurses By Shawna Quinn By Cathy O’Brien-Larivée, Rose McCloskey & Dianne McCormack the pulse 5 Message from the President 27 Ask a Practice Advisor 7 Message from the Executive Director 34 Calendar of Events 8 Boardroom Notes 38 Professional Conduct Review Decisions SPRING 2011 INFO NURSING 3 Info Nursing is published three times a year by the Nurses Association of New Brunswick, 165 Regent St., Fredericton, NB, E3B 7B4. -
Seniors'guide to Services and Programs
Seniors’ Guide to Services and Programs Tele-Care 811 is a bilingual, 24 hour, seven-day-a-week service that provides a wide range of health-related information, including advice and assistance on how best to get health- care services for specific needs. Services are provided through trained registered nurses and customer contact agents, depending on the type of information and assistance being sought. Deaf and hard-of-hearing New Brunswickers can now gain access to Tele-Care with TTY systems. TTYs are devices that enable people who are deaf or hard of hearing to use the telephone to communicate by typing messages. The toll-free number for TTY Tele-Care is 1-866-213-7920. Seniors’ Guide to Services and Programs November 2016 Published by: Province of New Brunswick PO Box 6000 Fredericton, NB E3B 5H1 Canada Printed in New Brunswick PRINT (English): ISBN 978-1- 4605-1051-3 PRINT (French): ISBN 978-1- 4605-1052-0 PDF (English): ISBN 978-1-4605-1053-7 PDF (French): ISBN 978-1-4605-1054-4 10769 Toll-Free Seniors’ Information Line New Brunswick has a toll-free number for seniors, their families and caregivers who are seeking information about government programs and services. For additional information about federal and provincial programs and services for seniors, contact the Seniors’ Information Line at 1-855-550-0552 (toll-free) and speak with an agent today! Hours of operation are 8:30 a.m. to 4:30 p.m., Monday to Friday. Seniors’ Guide to Services and Programs Table of contents Elections New Brunswick .................................................................................................................................. -
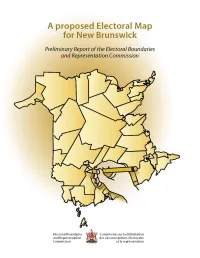
A Proposed Electoral Map for New Brunswick Preliminary Report of the Electoral Boundaries and Representation Commission
A proposed Electoral Map for New Brunswick Preliminary Report of the Electoral Boundaries and Representation Commission Electoral Boundaries Commission sur la délimitation and Representation des circonscriptions électorales Commission et la représentation Preliminary Report of the Electoral Boundaries and Representation Commission November 2005 2 Preliminary Report of the Electoral Boundaries and Representation Commission 3 Preliminary Report of the Electoral Boundaries and Representation Commission 4 Preliminary Report of the Electoral Boundaries and Representation Commission Table of Contents Introduction ..................................................................................................................................................... 1 Historical Overview .......................................................................................................................................... 1 The Electoral Boundaries and Representation Act ................................................................................................. 6 Public Input ..................................................................................................................................................... 9 Regional Approach ............................................................................................................................................ 13 Central New Brunswick ................................................................................................................................... 14 -

Some Historical Images of Health Care in New Brunswick
JOURNAL OF NEW BRUNSWICK STUDIES ISSUE 8 (FALL 2017) Some Historical Images of Health Care in New Brunswick Joshua Green P194-1403: Outdoor portrait of five people affected by leprosy at Tracadie, NB, [1885–1900]. A lazaretto operated in Tracadie from 1849–1964. "Do not call before ten, do not touch anything they have been using, do not even sit down upon their chairs, above all do not inhale their breath" (Dr. A.C. Smith, resident physician at the lazaretto). Mounted albumen print (cabinet card) by G.A. Burkhardt. Image provided with permission of the Provincial Archives of New Brunswick. http://w3.stu.ca/stu/sites/jnbs 5 REVUE D’ÉTUDES SUR LE NOUVEAU-BRUNSWICK ISSUE 8 (FALL 2017) P194-364: Studio portrait of participants of a six-week home nursing course taught by Miss Squires, a nurse from Fredericton’s Victoria Public Hospital, c. 1930. Squires traveled to Marysville to give classes one night a week in a room over Alexander (Boss) Gibson’s general store; the course was offered to help women cope with injured family members at home. Mounted silver gelatin print by Harvey Studio. Image provided with permission of the Provincial Archives of New Brunswick. http://w3.stu.ca/stu/sites/jnbs 6 JOURNAL OF NEW BRUNSWICK STUDIES ISSUE 8 (FALL 2017) P342-1143: Albert Street School children receiving polio vaccination at the time of the opening of the Polio Clinic and Health Centre at Victoria Public Hospital in Fredericton, 1955. The previous wooden polio clinic on the Victoria Public Hospital grounds had become woefully inadequate and was publicly criticized by many, including Dr. -

Fiscal Year 2022 Executive Budget
Queens Borough President Fiscal Year 2022 Executive Budget Response Donovan Richards Jr. Queens Borough President Table of Contents Summary 1 Office of the Queens Borough President 4 Community Boards 6 Department of Education/School Construction Authority 8 Department for the Aging 10 Administration for Children’s Services 17 Department of Youth and Community Development 19 Department of Health and Mental Hygiene 22 Fire Department 29 Police Department 31 Department of Sanitation 33 Department of Housing Preservation and Development 36 Department of Transportation 40 Queens Borough Public Library 42 Department of Cultural Affairs 44 Department of Parks and Recreation 47 Department of Small Business Services 49 Department of Buildings 51 City University of New York 53 Summary Office of the Queens Borough President ● Increase the agency budget to better serve the Borough of Queens Community Boards ● Fund the top budget priorities of each Community Board NYC Department of Education/School Construction Authority ● Dedicate capital funds for the construction and expansion of high schools ● Increase expense funding for Queens Schools ● Increase the number of child care in Queens ● Increase access to technology for students ● Continue City Council Initiatives NYC Department for the Aging ● Increase funding for senior services ● Restore Senior Services – Borough President Discretionary Funding ● Expand Home Delivered Meals to award organizations that provide culturally sensitive meals ● Continue City Council Initiatives NYC Administration for -

Strengthening Our Roots
Strengthening Our Roots A Practical Service Delivery Guide for Community-Based Responses to Sexual Assault Table of Contents Part One: Laying the Groundwork 1. History 6 2. Definitions, Statistics, and Language 7 3. Community Action Towards Ending Sexual Assault 9 a. Beliefs 10 b. Principles 11 c. Action 12 4. Minimum Core Services 13 5. Community Engagement 15 Part Two: Building a Community Response to Sexual Assault 1. A Survivor’s Needs – Minimum Core Services in Action 19 2. General Intervention Principles 25 3. 24 Hour Crisis Support 26 4. Short & Long Term Counselling 27 5. Trained Professionals and Service Providers 28 6. Service Delivery Coordination 29 7. Community Awareness 31 Part Three: Community Based Sexual Assault Responses 1. Branching Out 33 2. Establishing a Sexual Assault Response Team a. What is a SART 35 b. Community Engagement 37 c. Implementation 39 3. Personal Growth Workshops for Survivors of Sexual Assault a. What to consider when providing workshops or support 42 groups b. Sample Agenda 43 4. Establishing 24 Hour Sexual Assault Crisis Support a. From Dream to Reality 47 b. Crisis Support to Short Term Counselling – Filling a Gap 48 Part Four: The Fredericton Sexual Assault Crisis Centre 1. History of FSACC 50 2. Programs and Services 51 3. 24 Hour Crisis Response 52 a. Crisis Intervention Models 53 4. Volunteer Crisis Intervention Program 59 5. Counselling Program 61 a. Counselling Philosophy at FSACC 62 6. FSACC’s Feminist Perspective on Sexual Assault 64 Part Five: Community and Government Resources Provincial Services 67 Region 1 : Kent, Westmorland, and Albert County 69 Region 2 : Kings, St.