Understanding the Spatio-Temporal Dynamics of Meningitis Epidemics Outside the Belt: the Case of the Democratic Republic of Cong
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

With Effect from 1 April 2012 Through 30 June 2012
List of locations where payment of danger pay has been approved' with effect from 1 April 2012 through 30 June 2012: AFGHANISTAN CONGO, DEMOCRATIC REPUBLIC OF - North Kivu Province, South Kivu Province, Orientale Province - (only Bas Uele, Haut Uele and Ituri Districts), Maniema Province ETHIOPIA - Somali Region IRAQ - Entire country except Erbil KENYA - North Eastern Province (Garissa, Dadaab, Mandera, Wajir, Ijara) LEBANON - South Lebanon (UNIFIL Area of Operations, except the Tyre pocket) PAKISTAN - Balochistan Province, Khyber Pakhtunkhawa Province (formerly, North-West Frontier Province) and Federally Administrated Tribal Areas SOMALIA SOUTH SUDAN - Unity State, Upper Nile State, Jonglei State, Warrap State (except Tonji South county), in Lakes State (only Awerial, Yirol East, Rumbek Centre, Rumbek North and Rumbek East counties), in Northern Bar El Gazal State (only Aweil East and Aweil North counties), in Western Bar El Gazal State (all locations north of the road Kafia-Gabir-Kosho-Raja, excluding Raga town), Western Equatoria (only all locations south of the road Morobo-Yei-Maridi- Yambio-Nadi-Tambura, except Yambio town) SUDAN - the Darfurs (West, South and North Darfur), Abyei Administered Area, South Kordofan State and Blue Nile State SYRIA ARAB REPUBLIC - Entire country except Damascus (city boundaries) and UNDOF Area of Operations • YEMEN Addendum Please note that in addition to the approved locations above, on 3 July 2012, Danger Pay was also approved for the location below with retroactive effective date of 1 to 30 June 2012: ® Damascus, Syria. -

Deforestation and Forest Degradation Activities in the DRC
E4838 V5 DEMOCRATIC REPUBLIC OF THE CONGO MINISTRY FOR THE ENVIRONMENT, NATURE CONSERVATION AND TOURISM Public Disclosure Authorized STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ PROCESS Public Disclosure Authorized BASELINE REPORT STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ Public Disclosure Authorized PROCESS Public Disclosure Authorized October 2014 STRATEGIC ENVIRONMENTAL AND SOCIAL ASSESSMENT OF THE REDD+ PROCESS in the DRC INDEX OF REPORTS Environmental Analysis Document Assessment of Risks and Challenges REDD+ National Strategy of the DRC Strategic Environmental and Social Assessment Report (SESA) Framework Document Environmental and Social Management Framework (ESMF) O.P. 4.01, 4.04, 4.37 Policies and Sector Planning Documents Pest and Pesticide Cultural Heritage Indigenous Peoples Process Framework Management Management Planning Framework (FF) Resettlement Framework Framework (IPPF) O.P.4.12 Policy Framework (PPMF) (CHMF) O.P.4.10 (RPF) O.P.4.09 O.P 4.11 O.P. 4.12 Consultation Reports Survey Report Provincial Consultation Report National Consultation of June 2013 Report Reference and Analysis Documents REDD+ National Strategy Framework of the DRC Terms of Reference of the SESA October 2014 Strategic Environmental and Social Assessment SESA Report TABLE OF CONTENTS Introductory Note ........................................................................................................................................ 9 1. Preface ............................................................................................................................................ -

Mai-Ndombe Province: a REDD+ Laboratory in the Democratic Republic of the Congo
RIGHTS AND RESOURCES INITIATIVE | MARCH 2018 Rights and Resources Initiative 2715 M Street NW, Suite 300 Washington, DC 20007 P : +1 202.470.3900 | F : +1 202.944.3315 www.rightsandresources.org About the Rights and Resources Initiative RRI is a global coalition consisting of 15 Partners, 7 Affiliated Networks, 14 International Fellows, and more than 150 collaborating international, regional, and community organizations dedicated to advancing the forestland and resource rights of Indigenous Peoples and local communities. RRI leverages the capacity and expertise of coalition members to promote secure local land and resource rights and catalyze progressive policy and market reforms. RRI is coordinated by the Rights and Resources Group, a non-profit organization based in Washington, DC. For more information, please visit www.rightsandresources.org. Partners Affiliated Networks Sponsors The views presented here are not necessarily shared by the agencies that have generously supported this work, or all of the Partners and Affiliated Networks of the RRI Coalition. This work is licensed under a Creative Commons Attribution License CC BY 4.0. – 2 – Contents Acknowledgements ............................................................................................................................................ 4 Acronyms ............................................................................................................................................................. 5 Executive summary ........................................................................................................................................... -
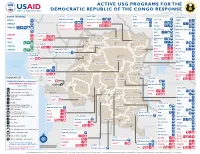
ACTIVE USG PROGRAMS for the DEMOCRATIC REPUBLIC of the CONGO RESPONSE Last Updated 07/27/20
ACTIVE USG PROGRAMS FOR THE DEMOCRATIC REPUBLIC OF THE CONGO RESPONSE Last Updated 07/27/20 BAS-UELE HAUT-UELE ITURI S O U T H S U D A N COUNTRYWIDE NORTH KIVU OCHA IMA World Health Samaritan’s Purse AIRD Internews CARE C.A.R. Samaritan’s Purse Samaritan’s Purse IMA World Health IOM UNHAS CAMEROON DCA ACTED WFP INSO Medair FHI 360 UNICEF Samaritan’s Purse Mercy Corps IMA World Health NRC NORD-UBANGI IMC UNICEF Gbadolite Oxfam ACTED INSO NORD-UBANGI Samaritan’s WFP WFP Gemena BAS-UELE Internews HAUT-UELE Purse ICRC Buta SCF IOM SUD-UBANGI SUD-UBANGI UNHAS MONGALA Isiro Tearfund IRC WFP Lisala ACF Medair UNHCR MONGALA ITURI U Bunia Mercy Corps Mercy Corps IMA World Health G A EQUATEUR Samaritan’s NRC EQUATEUR Kisangani N Purse WFP D WFPaa Oxfam Boende A REPUBLIC OF Mbandaka TSHOPO Samaritan’s ATLANTIC NORTH GABON THE CONGO TSHUAPA Purse TSHOPO KIVU Lake OCEAN Tearfund IMA World Health Goma Victoria Inongo WHH Samaritan’s Purse RWANDA Mercy Corps BURUNDI Samaritan’s Purse MAI-NDOMBE Kindu Bukavu Samaritan’s Purse PROGRAM KEY KINSHASA SOUTH MANIEMA SANKURU MANIEMA KIVU WFP USAID/BHA Non-Food Assistance* WFP ACTED USAID/BHA Food Assistance** SA ! A IMA World Health TA N Z A N I A Kinshasa SH State/PRM KIN KASAÏ Lusambo KWILU Oxfam Kenge TANGANYIKA Agriculture and Food Security KONGO CENTRAL Kananga ACTED CRS Cash Transfers For Food Matadi LOMAMI Kalemie KASAÏ- Kabinda WFP Concern Economic Recovery and Market Tshikapa ORIENTAL Systems KWANGO Mbuji T IMA World Health KWANGO Mayi TANGANYIKA a KASAÏ- n Food Vouchers g WFP a n IMC CENTRAL y i k -
A Life of Fear and Flight
A LIFE OF FEAR AND FLIGHT The Legacy of LRA Brutality in North-East Democratic Republic of the Congo We fled Gilima in 2009, as the LRA started attacking there. From there we fled to Bangadi, but we were confronted with the same problem, as the LRA was attacking us. We fled from there to Niangara. Because of insecurity we fled to Baga. In an attack there, two of my children were killed, and one was kidnapped. He is still gone. Two family members of my husband were killed. We then fled to Dungu, where we arrived in July 2010. On the way, we were abused too much by the soldiers. We were abused because the child of my brother does not understand Lingala, only Bazande. They were therefore claiming we were LRA spies! We had to pay too much for this. We lost most of our possessions. Once in Dungu, we were first sleeping under a tree. Then someone offered his hut. It was too small with all the kids, we slept with twelve in one hut. We then got another offer, to sleep in a house at a church. The house was, however, collapsing and the owner chased us. He did not want us there. We then heard that some displaced had started a camp, and that we could get a plot there. When we had settled there, it turned out we had settled outside of the borders of the camp, and we were forced to leave. All the time, we could not dig and we had no access to food. -

Drc): Case Studies from Katanga, Ituri and Kivu
CONFLICT BETWEEN INDUSTRIAL AND ARTISANAL MINING IN THE DEMOCRATIC REPUBLIC OF CONGO (DRC): CASE STUDIES FROM KATANGA, ITURI AND KIVU Ruben de Koning Introduction The mining sector in the Democratic Republic of Congo (DRC) is widely regarded as the key engine for post-conflict reconstruction. To attract for- eign investment, the government in 2002 enacted a new mining code that makes it easier for foreign companies to obtain industrial mining titles. Within a few years exploration concessions covered about a third of the country. Meanwhile, exploitation rights to the most important proven deposits were converted to new joint-ventures between foreign investors and Congolese state mining companies. The rapid attribution of min- ing titles has, however, not lead to a resumption of industrial mining on the scale the central government and its foreign donors had hoped for. Apart from a few copper and cobalt mines in the southern Katanga prov- ince, mineral production in the rest of the country, but also in Katanga, remains largely artisanal. Artisanal mining employs up to two million people across the country and largely takes place on concessions where industrial mining is supposed happen (Wold Bank 2009). In many of these artisanal mining areas and particularly in the eastern DRC state functions have almost completely eroded during two consecutive civil wars. Arti- sanal miners often work in dangerous conditions and are forced to pay numerous illegal taxes or to work for the military and rebel forces that control mines. At the same time, the local power complexes that emerged around artisanal mining operations have withheld large scale industrial investment, thereby preventing displacement of artisanal miners from concessions. -

Democratic Republic of Congo Democratic Republic of Congo Gis Unit, Monuc Africa
Map No.SP. 103 ADMINISTRATIVE MAP OF THE DEMOCRATIC REPUBLIC OF CONGO DEMOCRATIC REPUBLIC OF CONGO GIS UNIT, MONUC AFRICA 12°30'0"E 15°0'0"E 17°30'0"E 20°0'0"E 22°30'0"E 25°0'0"E 27°30'0"E 30°0'0"E Central African Republic N N " " 0 0 ' Sudan ' 0 0 ° ° 5 5 Z o n g oBangui Mobayi Bosobolo Gbadolite Yakoma Ango Yaounde Bondo Nord Ubangi Niangara Faradje Cameroon Libenge Bas Uele Dungu Bambesa Businga G e m e n a Haut Uele Poko Rungu Watsa Sud Ubangi Aru Aketi B u tt a II s ii rr o r e Kungu Budjala v N i N " R " 0 0 ' i ' g 0 n 0 3 a 3 ° b Mahagi ° 2 U L ii s a ll a Bumba Wamba 2 Orientale Mongala Co Djugu ng o R i Makanza v Banalia B u n ii a Lake Albert Bongandanga er Irumu Bomongo MambasaIturi B a s a n k u s u Basoko Yahuma Bafwasende Equateur Isangi Djolu Yangambi K i s a n g a n i Bolomba Befale Tshopa K i s a n g a n i Beni Uganda M b a n d a k a N N " Equateur " 0 0 ' ' 0 0 ° Lubero ° 0 Ingende B o e n d e 0 Gabon Ubundu Lake Edward Opala Bikoro Bokungu Lubutu North Kivu Congo Tshuapa Lukolela Ikela Rutshuru Kiri Punia Walikale Masisi Monkoto G o m a Yumbi II n o n g o Kigali Bolobo Lake Kivu Rwanda Lomela Kalehe S S " KabareB u k a v u " 0 0 ' ' 0 Kailo Walungu 0 3 3 ° Shabunda ° 2 2 Mai Ndombe K ii n d u Mushie Mwenga Kwamouth Maniema Pangi B a n d u n d u Bujumbura Oshwe Katako-Kombe South Kivu Uvira Dekese Kole Sankuru Burundi Kas ai R Bagata iver Kibombo Brazzaville Ilebo Fizi Kinshasa Kasongo KasanguluKinshasa Bandundu Bulungu Kasai Oriental Kabambare K e n g e Mweka Lubefu S Luozi L u s a m b o S " Tshela Madimba Kwilu Kasai -
CAP 2004 Drcongo SCREEN.Pdf
In Tribute In 2003 many United Nations, International Organisation, and Non-Governmental Organisation staff members died while helping people in several countries struck by crisis. Scores more were attacked and injured. Aid agency staff members were abducted. Some continue to be held against their will. In recognition of our colleagues’ commitment to humanitarian action and pledging to continue the work we began together We dedicate this year’s appeals to them. FOR ADDITIONAL COPIES, PLEASE CONTACT: UN OFFICE FOR THE COORDINATION OF HUMANITARIAN AFFAIRS PALAIS DES NATIONS 8-14 AVENUE DE LA PAIX CH - 1211 GENEVA, SWITZERLAND TEL.: (41 22) 917.1972 FAX: (41 22) 917.0368 E-MAIL: [email protected] THIS DOCUMENT CAN ALSO BE FOUND ON HTTP://WWW.RELIEFWEB.INT/ UNITED NATIONS New York and Geneva, November 2003 TABLE OF CONTENTS 1. EXECUTIVE SUMMARY.............................................................................................................................. 1 Summary of Requirements – By Appealing Organisation .............................................................................2 Summary of Requirements – By Sector ........................................................................................................ 3 2. THE YEAR IN REVIEW................................................................................................................................ 4 2.1 Changes In the Humanitarian Situation................................................................................................ 4 2.2 Financial -
The Mai Ndombe Redd+ Project Second Monitoring & Implementation Report (M2)
MONITORING REPORT: CCB Version 2, VCS Version 3 THE MAI NDOMBE REDD+ PROJECT SECOND MONITORING & IMPLEMENTATION REPORT (M2) Document Prepared by Wildlife Works Carbon Project Title The Mai Ndombe REDD+ Project Project ID 934 Version 4.3 Report ID 1 Date of Issue 22-October-2017 Project Location Democratic Republic of the Congo, Mai Ndombe Province Wildlife Works Carbon Project Proponent(s) Jeremy T. Freund [email protected]; 415-331-8081 Jeremy T. Freund, Simon Bird and Mike Korchinsky Prepared By Wildlife Works Carbon CCB v2.0, VCS v3.4 1 MONITORING REPORT: CCB Version 2, VCS Version 3 EPIC Sustainability Services K. Suryanarayana Murthy Validation/Verification Body [email protected] +91 9845759000 GHG Accounting/Crediting 14 March 2011 – 13 March 2041 Period 30-year crediting period Monitoring Period of this 01 November 2012 – 31 December 2016 Report Validation: 06 December 2011 History of CCB Status Verification (m1): 06 December 2011 Climate and Biodiversity Gold Level Criteria The Project will conserve flora and fauna within the Project Area. Protecting these 2 former logging concessions will maintain critical forested area and the ecosystem services that it provides, as well as rehabilitate habitat for endangered charismatic animals such as the Bonobo and Forest Elephant. By protecting the native forest, the Project will also increase the resilience of the ecosystem to the effects of climate change. Section GL1.4 of the CCB PDD exemplifies many additional Project Activities that will help both local communities and biodiversity to minimize and adapt to expected climate change impacts. Improved seed distribution and training on improved Gold Level Criteria agricultural methods will lead to increased yields and adaptation to changes in rainfall, the timing of growing seasons, and changing temperatures. -

Review of the National Program for Onchocerciasis Control in the Democratic Republic of the Congo
Tropical Medicine and Infectious Disease Review Review of the National Program for Onchocerciasis Control in the Democratic Republic of the Congo Jean-Claude Makenga Bof 1,* , Fortunat Ntumba Tshitoka 2, Daniel Muteba 2, Paul Mansiangi 3 and Yves Coppieters 1 1 Ecole de Santé Publique, Université Libre de Bruxelles (ULB), Route de Lennik 808, 1070 Brussels, Belgium; [email protected] 2 Ministry of Health: Program of Neglected Tropical Diseases (NTD) for Preventive Chemotherapy (PC), Gombe, Kinshasa, DRC; [email protected] (F.N.T.); [email protected] (D.M.) 3 Faculty of Medicine, School of Public Health, University of Kinshasa (UNIKIN), Lemba, Kinshasa, DRC; [email protected] * Correspondence: [email protected]; Tel.: +32-493-93-96-35 Received: 3 May 2019; Accepted: 30 May 2019; Published: 13 June 2019 Abstract: Here, we review all data available at the Ministry of Public Health in order to describe the history of the National Program for Onchocerciasis Control (NPOC) in the Democratic Republic of the Congo (DRC). Discovered in 1903, the disease is endemic in all provinces. Ivermectin was introduced in 1987 as clinical treatment, then as mass treatment in 1989. Created in 1996, the NPOC is based on community-directed treatment with ivermectin (CDTI). In 1999, rapid epidemiological mapping for onchocerciasis surveys were launched to determine the mass treatment areas called “CDTI Projects”. CDTI started in 2001 and certain projects were stopped in 2005 following the occurrence of serious adverse events. Surveys coupled with rapid assessment procedures for loiasis and onchocerciasis rapid epidemiological assessment were launched to identify the areas of treatment for onchocerciasis and loiasis. -

Democratic Republic of the Congo Complex Emergency 09-30-2013
DEMOCRATIC REPUBLIC OF THE CONGO - COMPLEX EMERGENCY FACT SHEET #3, FISCAL YEAR (FY) 2013 SEPTEMBER 30, 2013 NUMBERS AT USAID/OFDA 1 F U N D I N G HIGHLIGHTS A GLANCE BY SECTOR IN FY 2013 U.S. Government (USG) provided nearly $165 million of humanitarian assistance in 6.4 5% the Democratic Republic of the Congo 7% 25% (DRC) in FY 2013 million 8% Insecurity and poor transportation People in Need of Food infrastructure continue to hinder and Agriculture Assistance 8% humanitarian access across eastern DRC U.N. Office for the Coordination of Humanitarian Affairs (OCHA) – August 2013 8% HUMANITARIAN FUNDING 23% TO DRC TO DATE IN FY 2013 16% 2.6 USAID/OFDA $48,352,484 USAID/FFP2 $56,471,800 million Health (25%) 3 Logistics & Relief Commodities (23%) State/PRM $60,045,000 Total Internally Displaced Water, Sanitation, & Hygiene (16%) Persons (IDPs) in the DRC Economic Recovery & Market Systems (8%) U.N. – August 2013 Humanitarian Coordination & Information Management (8%) $164,869,284 Agriculture & Food Security (8%) TOTAL USAID AND STATE Protection (7%) HUMANITARIAN ASSISTANCE TO DRC 434,306 Other (5%) Congolese Refugees in Africa Office of the U.N. High Commissioner for Refugees KEY DEVELOPMENTS (UNHCR) – August 2013 During FY 2013, violence intensified and humanitarian conditions deteriorated across eastern DRC, with the spread of a secessionist movement in Katanga Province, escalating 185,464 clashes and related displacement in Orientale Province, and worsening instability resulting Total Refugees in the DRC in tens of thousands of new displacements in North Kivu and South Kivu provinces. UNHCR – August 2013 Conflict continues to cause displacement, raise protection concerns, and constrain humanitarian access to populations in need of assistance. -

Democratic Republic of the Congo (DRC) Situation Update 22 September 2014
Democratic Republic of the Congo (DRC) Situation Update 22 September 2014 LOCATION: Kinshasa, DRC DATE: 22 September 2014 Situation Overview The Democratic Republic of Congo (DRC) is a high-risk country for the Ebola Virus Disease (EVD). The current outbreak has been confirmed by the Minister of Health (MoH) on 26 August 2014. As of 21 September 2014, 68 confirmed cases have been to have contracted Ebola, out of which 41 were fatal. So far, all cases point to a different strain of the virus than currently encountered in West Africa. All cases have been located in Djera county of Boende territory in the Equateur Province, 1,200 km northeast of the capital Kinshasa and 300 km east of the province’s capital Mbandaka. Cases have been reported in WatsiKengo, Lokolia, Boende and Boende Moke. The government has assumed overall coordination and implementation of the Ebola response, with UN agencies and NGOs providing assistance. It has published a response plan in August 2014 that serves as road map and defines the overall coordination and the strategy of implementation for three months, from September to November 2014. Emergency measures include: ○ A quarantine area, 100km around the epicentre of the outbreak, has been established by the government, restricting the movement of the 30,000 to 40,000 people living in the affected areas. ○ A National Coordination Committee (CNC, Comité National de Coordination) has been established to coordinate the Ebola response under the leadership of the Minister of Health (MoH), with the Office for the Coordination of Humanitarian Affairs (OCHA) as focal point for the humanitarian response.