OMS Opsoclonus-Myoclonus Protocol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RAMBAMHCC Pictured on Cover and Facing Page: Bone Marrow Transplant Patients and Medical Staff Exercise at Daybreak on the Haifa Beach Promenade RAMBAMHCC
RAMBAMHCC Pictured on cover and facing page: Bone marrow transplant patients and medical staff exercise at daybreak on the Haifa beach promenade RAMBAMHCC ANNUAL REPORT 2015 RAMBAM HEALTH CARE CAMPUS RAMBAMHCC l 2015 ANNUAL REPORT WELCOME TO HAIFA THE ISRAELI BIOTECH MEGA CENTER 3 RAMBAM MEDTECH The digital healthcare market is projected to exceed $50 billion by the year 2020 and to catalyze an economic and quality revolution on the global medicine map. Rambam MedTech, along with medical technology leaders IBM Watson Health, Medtronic, and Pitango Venture Capital, was selected to establish a new digital medicine incubator in Haifa. MindUP is expected to cultivate over 40 new companies over the next decade, having a rippling impact on the future of digital medicine locally, nationally, and worldwide. INTRODUCING THE HAIFA BIOTECH INCUBATOR 6 HAIFA MUNICIPALITY ISRAEL Architect’s design for the new complex to be built in the Haifa Life Sciences Park 6 FROM THE DIRECTOR Professor Rafi Beyar MD, DSc, MPH Director & CEO Rambam Health Care Campus WELCOME TO RAMBAM RAMBAMHCC l 2015 ANNUAL REPORT Esteemed friends and benefactors, for professional excellence and innovation, placing patients at the center of every endeavor. Almost ten years have passed since the Second Professor Itay Shavit, Director of the Pediatric Lebanon War delivered its resounding wake-up Emergency Unit at the Ruth Rappaport call, reminding us of our responsibility to provide Children’s Hospital, observed, “when you offer a secure environment during wartime for the excellent services in an attractive facility, people population of Northern Israel, and for our staff will come.” This has been borne out by the rise who are charged with their care. -
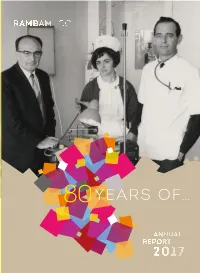
Years Of… Years Of…
YEARS OF… YEARS OF… RAMBAMHCC ANNUAL REPORT 2017 American Friends of Rambam www.aforam.org [email protected] (212) 292-4499 Australian Friends of Rambam www.ausforam.org.au [email protected] (61) 0410 531 593 British Friends of Rambam (Rambam UK) www.rambamuk.co.uk [email protected] (208) 343-8749 Canadian Friends of Rambam www.cfram.ca [email protected] (416) 481-5552 French Friends of Rambam [email protected] (33) 7 82 53 71 10 Friends of Rambam in India [email protected] (98) 191-113-40 Spanish Friends of Rambam www.amigosderambam.org [email protected] (609) 580-268 Israeli Friends of Rambam www.rambam.org.il [email protected] (04) 852-0670 Israel Main Office & All Other Countries www.rambam.org.il [email protected] +972 (4) 777-2919 Pictured on cover: Prof. David Ehrlich (l) and Prof. Ori Better, inducted into the Rambam Leadership Circle in 2017, with Nurse Ilana Ungerman-Tamir. Photo: December 1965 1940 1945 1938-48 Dr. John Herbert Thompson First Hospital Director The graphic relief adorning the hospital’s I O A T N first building in 1938 was designed by the R U world-renowned British sculptor and G type designer Eric Gill U A N I 1938 December 22 YEARS New Government Hospital OF Inaugurated in Bat Galim, Haifa EXCELLENCE, INNOVATION AND HUMANITY ’38 German Jewish expressionist architect Erich Mendelsohn 1950 1955 1948-63 Dr. Raphael Gjebin Second Hospital Director 1948-58 Elsa Yellin - First Head Nurse I O A T N 1948 R U School of Nursing Established, G Headed by Elsa Yellin U A N I I O 1952 A T N R U Government Hospital G Becomes Rambam U A N I 1948 Following an attack on Kibbutz Gesher it was decided to evacuate all the mothers and children to the Carmelite convent next to the hospital Declaration of ’48 Independence of the State of Israel 1960 1965 Dr. -
2016 Annual Report
Pictured on cover: Rambam’s new state-of-the-art Joseph Fishman Oncology Center opens its doors. BEATING CANCER RAMBAMHCC l 2016 ANNUAL REPORT FISHMAN OPENS And ushers in a new era of hope and healing for cancer patients throughout Israel. A look inside Rambam’s new state-of-the-art Joseph Fishman Oncology Center. A West Campus Landmark Opened in June 2016, the eight-story Joseph Fishman Oncology Center is the newest addition to Rambam’s dynamic West Campus. The only full-service cancer center in all of northern Israel, the Joseph Fishman Oncology Center welcomes its patients with a modern, comfortable facility designed to promote healing and wellbeing. At 100,000 m2, the new center is double the size of the former facility, and houses hospitalization and outpatient departments for chemotherapy, radiation therapy and brachytherapy, as well as research labs and space for a state-of- the-art Radiation Therapy Institute and a Complementary Care Center, planned for construction as resources become available. 3 FISHMAN IS: An Environmentally-Conscientious “Green” Building From initial conceptual and architectural planning, through the selection of sustainable materials and resource-saving systems, the Joseph Fishman Oncology Center was built with the wellbeing of the patients, staff and the environment in mind. From structure to function, the building complies with the Israel Standards Institute’s stringent “Green Building” standard for medical institutions. FISHMAN IN NUMBERS 2016 33,562 21,241 DAY CARE CLINIC VISITS VISITS 2,607 1,248 NEW CLINIC NEW DAY CARE VISITORS VISITORS Patient Privacy and Dignity Patients in the new Joseph Fishman Oncology Center benefit from thoughtfully designed treatment and hospitalization areas that are spacious, private, and can comfortably accommodate accompanying family members and visitors. -
Corporate Responsibility Report for Stakeholders
Corporate Responsibility Report for Stakeholders Israel Chemicals Ltd. CONTENTS CEO Letter .................................................................................................................................................... 3 1 - Corporate Responsibility at ICL .................................................................................... 4 2 - Organizational profile ............................................................................................................. 8 3 - Opportunities and Risks - Chemical Industry ............................................20 4 - Products & Responsibility - Along the Value Chain .............................28 5 - Environmental aspects .......................................................................................................34 6 - Social aspects ...............................................................................................................................48 1 "Throughout our history, ICL has never wavered in its efforts to uphold and promote its core values. They include respect for the law, protecting the environment, ensuring the safety and health of our workers and taking into consideration the interests of our customers, our suppliers and the communities in which we operate" 2 CEO LETTER I am very pleased to present you with ICL's first Corporate Responsibility Report. As someone who has been affiliated with ICL for more than three decades, I can testify to the enormous changes that the Company has undergone - and the challenges it has faced -

Characterization and Genotype-Phenotype Correlation of Patients with Fanconi Anemia in Ferrata Storti Foundation a Multi-Ethnic Population
Bone Marrow Failure ARTICLE Characterization and genotype-phenotype correlation of patients with Fanconi anemia in Ferrata Storti Foundation a multi-ethnic population Orna Steinberg-Shemer,1,2,3* Tracie A. Goldberg,1* Joanne Yacobovich,1,2 Carina Levin,4,5 Ariel Koren,4,5 Shoshana Revel-Vilk,6 Tal Ben-Ami,7 Amir A. Kuperman,8,9 Vered Shkalim Zemer,1,2 Amos Toren,2,10 Joseph Kapelushnik,11 Ayelet Ben-Barak,12 Hagit Miskin,6 Tanya Krasnov,3 Sharon Noy-Lotan,3 Orly Dgany3 and Hannah Tamary1,2,3 1 Haematologica 2020 Department of Hematology-Oncology, Schneider Children's Medical Center of Israel, Volume 105(7):1825-1834 Petach Tikva; 2Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv; 3Pediatric Hematology Laboratory, Felsenstein Medical Research Center, Petach Tikva; 4Pediatric Hematology Unit, Emek Medical Center, Afula; 5The Ruth and Bruce Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Haifa; 6Pediatric Hematology/Oncology Unit, Shaare Zedek Medical Center, Jerusalem, affiliated with Hadassah- Hebrew University Medical School, Jerusalem; 7Pediatric Hematology Unit, Kaplan Medical Center, Rehovot; 8Blood Coagulation Service and Pediatric Hematology Clinic, Galilee Medical Center, Nahariya; 9Azrieli Faculty of Medicine, Bar-Ilan University, Safed; 10Department of Pediatric Hemato-Oncology, Children's Hospital (Edmond and Lily), Sheba Medical Center, Tel-Hashomer; 11Pediatric Hematology, Soroka University Medical Center, Ben-Gurion University, Beer Sheva and 12Pediatric Hematology-Oncology Department, Rambam Medical Center, Haifa, Israel *OS-S and TAG contributed equally as co-first authors. ABSTRACT ANCONI ANEMIA (FA), AN INHERITED BONE MARROW FAILURE (BMF) SYNDROME, CAUSED BY MUTATIONS IN DNA REPAIR GENES, IS CHARACTERIZED BY CONGENI- Correspondence: FTAL ANOMALIES, APLASTIC ANEMIA, HIGH RISK OF MALIGNANCIES AND EXTREME HANNAH TAMARY SENSITIVITY TO ALKYLATING AGENTS. -

New Ruth Rappaport Children's Hospital
Celebrating the New Ruth RambamISSUE No. 15 | March 2015 Rappaport Children's on call Hospital The Doctors, the Departments, the Services and the Smiles all in this SPECIAL ISSUE Rambam on call so badly need. With the opening of the Ruth Rappaport Children’s Hospital, this heart-rending and complex picture has become immeasurably brighter. The Ruth Rappaport Children’s Hospital represents the compassionate vision of Bruce (z”l) and Ruth Rappaport, who saw Rambam’s old, outmoded and overcrowded children’s hospital and decided to give new hope to the children of Northern Israel. Consistent with that vision, every Dear Friends, detail in the new hospital is attuned to the healing The mother of a tiny premature infant takes process, as you will see in the pages of this special a moment to rest in the family waiting room issue of Rambam on Call. of the Neonatal Intensive Care Department. It is my passionate wish that no child will ever A young girl carrying a backpack heavy with need the services of our hospital. But if they do, I books and toys makes her familiar way to the am proud to say that one of the most outstanding Oncology Department for a treatment. A small children’s hospitals in Israel and the world is at boy injured in a bicycle accident is sent home, their service. sutured and bandaged, relief spread across his tear-stained face. Sincerely, A children’s hospital is a human mosaic, PROF. RAFI BEYAR encompassing anguish and hope, children’s smiles and parent’s stress-drawn faces, doctors whose split-second d ecisions save young lives and Director and CEO nurses who provide the comfort young patients Rambam Health Care Campus With the arrival of spring and Passover, we wish you and your loved ones a year of innovation, health, and freedom. -

Discount Bank 019 ICC - Services in the Credit Card 72 Profile, Corporate Field Governance and Values 013 Social Networks
Content 7 Greetings from the Chairman and the 19 The Customers President & CEO 97 General policy 9 A Corporate Responsibility Report – what is it? 99 Retail Customers - household segment 01 Challenges and opportunities in the 017 Customers of the small business field of social responsibility segment 01 Discount's fifth Corporate 011 Private Banking customers Responsibility Report 011 Service to corporate customers 01 The process of identification of 001 Customers of middle market banking material Aspects segment 01 Aspects defined as material 001 Additional services 01 Reporting to the Global Compact 010 Technological improvements and 10 Control over the appropriateness of innovation reporting - Discount Bank 019 ICC - services in the credit card 72 Profile, Corporate field Governance and Values 013 Social networks 19 The Discount Group - general overview 011 Financial education and structure of the Group 070 Business continuity 73 Communication with investors in 077 Accessibility to handicapped persons securities of the Bank 071 Proper disclosure - information 79 Issues regarding corporate governance regarding products and services 99 Principal control functions 073 Communication with customers - 62 Vision and Values improvement of service 11 The code of ethics 011 Confidentiality and privacy 13 Corporate Governance Code for the 097 Appendix: Suppliers Discount Group 951 The Employees 11 Prevention of bribery, fraud and embezzlement 010 Human Resources Policy 30 Additional Ethical Aspects 031 Employment terms and remuneration 33 Financial -

Corporate Responsibility Report 2017
Corporate 2017 Responsibility Report Corporate Responsibility Report 2017 This report is a translation from the Hebrew and has been prepared for convenience only. In case of any discrepancy the Hebrew will prevail. The Employees 100 Table of 05 Nurturing of Discount Bank’s human capital 102 Discount Bank’s employees 104 Diversity and equal opportunity 112 Investing more in employees 118 Contents Maintaining employee rights 137 Goals 144 About the report 06 Suppliers 148 Greetings from the Chairman and the President & CEO 08 Promotion of responsible purchasing 150 01 Discount's Seventh Corporate Social Responsibility Report 10 06 Goals 155 Dialogue with stakeholders 13 The process of identification of material Topics 13 Discount for the community 156 Discount for the community 158 Reporting to the Global Compact 16 07 "Discount Sprint for the Future" 159 Discount Bank and the United Nations' sustainable development goals 16 Discount volunteering in the community 164 Assurance examination 19 Investment in the community 166 Group profile and financial data 22 "Herzelilinblum" 170 02 Discount Bank - General Overview 24 Goals 173 Mercantile Discount Bank - General Overview 30 Green Discount 176 Israel Credit Cards Ltd. ("ICC") - General Overview 33 08 Policy 178 IDB Bank - General Overview 37 "Green credit" 179 Membership of organizations and external Initiatives 38 Promoting green building 180 Social Responsibility Ratings 39 Responsible consumption of resources 182 Commendations and prizes 40 Goals 193 Contributing to the economy 41 Corporate -

2014 ANNUAL REPORT Pictured on Cover: the Ruth Rappaport Children’S Hospital RAMBAMHCC 2014 ANNUAL REPORT HOPE STARTS HERE
RAMBAMHCC 2014 ANNUAL REPORT Pictured on cover: The Ruth Rappaport Children’s Hospital RAMBAMHCC 2014 ANNUAL REPORT HOPE STARTS HERE The new Ruth Rappaport Children’s Hospital opens JUNE 2014 RUTH RAPPAPORT CHILDREN’S HOSPITAL IN NUMBERS 110% OCCUPANCY 99% 97% 83% 78% 81% 77% 58,056 53% HOSPITALIZATION DAYS Oncology Newborn Surgery Pediatric A Pediatric B NeonatologyIntensive Care Bone marrow Transplants 23,243 26% EMERGENCY HOSPITALIZED ADMISSIONS 3,534 ON 1,100 ONCOLOGY OUTPATIENT CHILDREN TREATMENTS 7,701 ON 53 Dialysis TREATMENTS CHILDREN AGE 0-1 YRS 17% 11-18 YRS 32% 1-5 YRS 33% 44,132 6-10 YRS CHILDREN TREATED 18% in 2014 AGE 0-1 YRS 7% 11-18 YRS 1-5 YRS 43% 28% 5,334 SURGERIES 6-10 YRS 22% <750gr 751- 24 1000gr 19 1001- 1500gr 49 >2501gr 524 222 PREMATURE BIRTHS 1501- 2500gr 210 ON BEHALF OF NORTHERN ISRAEL’S 600,000 CHILDREN WE WOULD LIKE TO THANK: Ruth & Bruce Rappaport and Family Ariela & Eitan Wertheimer Joan & Sanford Weill and the Weill Family Foundation Meri & Sol J. Barer Herta & Paul Amir Relly & Brent Dibner Irma & Aaron Spencer The David & Jacqueline Simon Family The Israel Cancer Association (R.A) Effi & Eli Goldhar The D. Dan & Betty Kahn Foundation Goldie Feldman, Barry & Laurie Green and Family, David Green, Daphne Wagner, Lita & Mickey Green Harry & Sara Gorman, Hy & Bertha Shore David A. Cohen Family Alice & Maurice Benard Women’s League for Israel Dream Doctors The Leir Charitable Foundations Anonymous, Switzerland Tatyana & Alan J. Forman The Greidinger Family Michelle Kahn Zahava & Yoram Cedar Fondation Adelis Pierre Mandel Erna Feist-Elzas …and 981 donors worldwide for helping make the Ruth Rappaport Children’s Hospital a reality 7 7 Professor Rafi Beyar MD, DSc, MPH Director & CEO Rambam Health Care Campus RAMBAMHCC l 2014 ANNUAL REPORT FROM THE DIRECTOR FROM VISION TO REALITY Esteemed friends and benefactors… In front of our eyes, Rambam is undergoing an extraordinary transformation. -

Investigation of the Role of Dinutuximab Beta-Based Immunotherapy in the SIOPEN High-Risk Neuroblastoma 1 Trial (HR-NBL1)
cancers Article Investigation of the Role of Dinutuximab Beta-Based Immunotherapy in the SIOPEN High-Risk Neuroblastoma 1 Trial (HR-NBL1) 1, , 2, 3 4 Ruth Ladenstein * y, Ulrike Pötschger y, Dominique Valteau-Couanet , Roberto Luksch , Victoria Castel 5 , Shifra Ash 6, Geneviève Laureys 7 , Penelope Brock 8, Jean Marie Michon 9, Cormac Owens 10, Toby Trahair 11, Godfrey Chi Fung Chan 12, Ellen Ruud 13, Henrik Schroeder 14, Maja Beck-Popovic 15, Guenter Schreier 16 , Hans Loibner 17, Peter Ambros 2, Keith Holmes 18, Maria Rita Castellani 4, Mark N. Gaze 19 , Alberto Garaventa 20, Andrew D.J. Pearson 21 and Holger N. Lode 22 1 St. Anna Children‘s Hospital and Children’s Cancer Research Institute (CCRI), Department of Paediatrics, Medical University, 1090 Vienna, Austria 2 Children’s Cancer Research Institute (CCRI), St. Anna Kinderkrebsforschung, Department of Paediatrics, Medical University, 1090 Vienna, Austria; [email protected] (U.P.); [email protected] (P.A.) 3 Children and Adolescent Oncology Department, Gustave Roussy, Paris-Sud, University, 94805 Villejuif, France; [email protected] 4 Fondazione IRCCS Istituto Nazionale dei Tumori, 20133 Milan, Italy; [email protected] (R.L.); [email protected] (M.R.C.) 5 Hospital Universitario y Politecnico La Fe, 46026 Valencia, Spain; [email protected] 6 Schneider Children‘s Medical Center of Israel, Sackler Faculty of Medicine Tel Aviv University, Petach, Tikvah 49202, Israel; [email protected] 7 University Hospital Ghent, -

Corporate Responsibility Report 2017
Corporate 2017 Responsibility Report Dummy Text Corporate Responsibility Report 2017 This report is a translation from the Hebrew and has been prepared for convenience only. In case of any discrepancy the Hebrew will prevail. Dummy Text The Employees 100 Table of 05 Nurturing of Discount Bank’s human capital 102 Discount Bank’s employees 104 Diversity and equal opportunity 112 Investing more in employees 118 Contents Maintaining employee rights 137 Goals 144 About the report 06 Suppliers 148 Greetings from the Chairman and the President & CEO 08 Promotion of responsible purchasing 150 01 Discount's Seventh Corporate Social Responsibility Report 10 06 Goals 155 Dialogue with stakeholders 13 The process of identification of material Topics 13 Discount for the community 156 Discount for the community 158 Reporting to the Global Compact 16 07 "Discount Sprint for the Future" 159 Discount Bank and the United Nations' sustainable development goals 16 Discount volunteering in the community 164 Assurance examination 19 Investment in the community 166 Group profile and financial data 22 "Herzelilinblum" 170 02 Discount Bank - General Overview 24 Goals 173 Mercantile Discount Bank - General Overview 30 Green Discount 176 Israel Credit Cards Ltd. ("ICC") - General Overview 33 08 Policy 178 IDB Bank - General Overview 37 "Green credit" 179 Membership of organizations and external Initiatives 38 Promoting green building 180 Social Responsibility Ratings 39 Responsible consumption of resources 182 Commendations and prizes 40 Goals 193 Contributing -

Israel Chemicals Ltd Corporate Responsibility Report 2013
Israel Chemicals Ltd. Corporate Responsibility Report 2013 Foreword Foreword We are honored to present the Corporate Responsibility Report increasing population. The task of solving them are among the of Israel Chemicals (ICL) for 2013. ICL’s tradition of reporting, issues that can be read in detail in this report, including the which began in 2006, continues to develop and improve critical need to produce increasing quantities of food without every year, demonstrating the comprehensive operational the availability of a corresponding increase in the amount of strategy for sustainability and corporate responsibility that we land allocated for agriculture; an effort to protect open spaces; are implementing at ICL. This report is the fourth written and guarantee quality food for the world’s population; and ensure published according to the international guidelines of the Global a supply of engineered materials required to meet humanity’s Reporting Initiative (GRI). It covers our work and progress during most basic needs. ICL’s extensive activities cover the entire 2013. We intend to continue reporting, and even to expand, this life cycle of the products and materials that we manufacture, format in the future as part of our Company’s enhanced strategic from raw materials and manufacturing through end sales. This thinking and activity on social and environmental issues in all breadth of activity allows ICL to offer appropriate solutions aspects of our activities. for the varying needs of humanity, through three critical end markets: agriculture, foods and engineered materials. For more than a decade, the environmental-social strategy of ICL has been woven throughout the fabric of our business and is The many challenges faced by human society obligate ICL, implemented in all of ICL’s business activities around the world.