Malnutrition in the Philippines - Perhaps a Double Burden?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OCULAR MANIFESTATIONS of VITAMIN a DEFICIENCY*T
Br J Ophthalmol: first published as 10.1136/bjo.51.12.854 on 1 December 1967. Downloaded from Brit. J. Ophthal. (1967) 51, 854 OCULAR MANIFESTATIONS OF VITAMIN A DEFICIENCY*t BY G. VENKATASWAMY Department of Ophthalmology, Madurai Medical College, Madurai, India NUTRITIONAL deficiencies are a frequent cause of serious eye disease in India. Oomen (1961) reported a mortality of nearly 30 per cent. in young children with keratomalacia and an even higher proportion in those with protein malnutrition; about 25 per cent. of the survivors became totally blind, and about 60 per cent. were left with reduced vision in one or both eyes. Deficiency diseases revealed by dietary surveys have included xerophthalmia, Bitot's spots, angular stomatitis, and phrynoderma. Gilroy (1951) observed xerophthalmia in 250 out of 4,191 children from 44 estates in Assam. Sundararajan (1963) found signs of vitamin A deficiency in 35 to 45 per cent. of schoolchildren in Calcutta. Chandra, Venkatachalam, Belavadi, Reddy, and Gopalan (1960) reported that lack of protein and vitamin A was the most frequent cause of nutritional deficiency disorders in India; out of copyright. 14,563 children examined in a 5-year period, 2,245 showed malnutrition, 551 vitamin A deficiency, and 157 keratomalacia. Rao, Swaminathan, Swarup, and Patwardhan (1959) observed two to five cases ofvitamin A deficiency for every case ofkwashiorkor. A world-wide survey ofxerophthalniia carried out in nearly fifty countries (including countries in Asia) by WHO in 1962-1963 revealed that this was often the most important cause of blindness in young children. Scrimshaw (1959), McLaren (1963), and UNICEF (1963) concluded that vitamin A deficiency was one of the http://bjo.bmj.com/ main nutritional problems in tropical and subtropical areas. -

Kwashiokorl. Description of Kwashiorkor Kwashiorkor Is a Life-Threatening and Debilitating Form of Malnutrition. It's Caused B
Name ;OLAWUYI MUQTADIR OREDOLAPO COUSE AFE 101 DEPARTMENT ;ACCOUNTING KWASHIOKORl. Description of kwashiorkor kwashiorkor is a life-threatening and debilitating form of malnutrition. It’s caused by a lack of protein in your diet. Kwashiorkor is also commonly seen in low- and lower-middle-income regions facing famine. Signs and symptoms of kwashiorkor The symptoms of kwashiorkor include; • damaged immune system, which can lead to more frequent and severe infections • irritability. • flaky rash • shock. • change in skin and hair colour (to a rust colour) and texture • fatigue • diarrhea • loss of muscle mass • failure to grow or gain weight • edema (swelling) of the ankles, feet, and belly SUSCEPTIBLES If kwashiorkor is suspected, your doctor will first examine you to check for an enlarged liver (hepatomegaly) and swelling. Next, blood and urine tests may be ordered to measure the level of protein and sugar in your blood. Other tests may be performed on your blood and urine to measure signs of malnutrition and lack of protein. These tests may look for muscle breakdown and assess kidney function, overall health, and growth. These tests include: arterial blood gas, blood urea nitrogen , urinalysis e.t.c. TREATMENT Kwashiorkor can be corrected by eating more protein and more calories overall, especially if treatment is started early. You may first be given more calories in the form of carbohydrates, sugars, and fats. Once these calories provide energy, you will be given foods with proteins. Foods must be introduced and calories should be increased slowly because you have been without proper nutrition for a long period. Your body may need to adjust to the increased intake. -

Involvement of the Eye in Protein Malnutrition * -303
Bull. Org. mond. Sante 1958, 19, 303-314 Bull. Wld Hith Org. INVOLVEMENT OF THE EYE IN PROTEIN MALNUTRITION * D. S. McLAREN, M.D., Ph.D., D.T.M. & H. Medical Research Officer, East African Institute for Medical Research, Mwanza, Tanganyika Formerly at the MRC Human Nutrition Research Unit, National Institute for Medical Research, London SYNOPSIS An extensive review of the literature on protein malnutrition, with special reference to the frequency of involvement of the eyes, has been made by the author. Consideration of accounts from all parts of the world and in many different languages, including early as well as more recent descriptions of the syndrome, indicates that this important complication has not received sufficient attention hitherto. The evidence available suggests that it is nearly always an accompanying deficiency of vitamin A that is responsible. Less commonly reported-and producing less severe effects-is deficiency of the B-complex vitamins, and there is no clear evidence to date that protein deficiency itself damages the eyes in these cases. The ways in which protein lack might interfere with various aspects of vitamin-A metabolism are discussed, but it is pointed out that their actual significance in human disease is not yet known. A low dietary intake of vitamin A is regarded by the author as being the prime factor in the causation of eye complications, and attention is drawn to the necessity to correct this as part of any prophylactic or therapeutic programme aimed primarily at combat- ing protein malnutrition. The syndrome known by such various names as kwashiorkor, nutritional oedema syndrome, sindrome pluricarencial, and many others (Trowell, Davies & Dean, 1954), and characterized chiefly by a dietary deficiency ofprotein, has been reported as occurring amongst most of the malnourished communities of the world. -

Vitamins a and E and Carotenoids
Fat-Soluble Vitamins & Micronutrients: Vitamins A and E and Carotenoids Vitamins A (retinol) and E (tocopherol) and the carotenoids are fat-soluble micronutrients that are found in many foods, including some vegetables, fruits, meats, and animal products. Fish-liver oils, liver, egg yolks, butter, and cream are known for their higher content of vitamin A. Nuts and seeds are particularly rich sources of vitamin E (Thomas 2006). At least 700 carotenoids—fat-soluble red and yellow pigments—are found in nature (Britton 2004). Americans consume 40–50 of these carotenoids, primarily in fruits and vegetables (Khachik 1992), and smaller amounts in poultry products, including egg yolks, and in seafoods (Boylston 2007). Six major carotenoids are found in human serum: alpha-carotene, beta-carotene, beta-cryptoxanthin, lutein, trans-lycopene, and zeaxanthin. Major carotene sources are orange-colored fruits and vegetables such as carrots, pumpkins, and mangos. Lutein and zeaxanthin are also found in dark green leafy vegetables, where any orange coloring is overshadowed by chlorophyll. Trans-Lycopene is obtained primarily from tomato and tomato products. For information on the carotenoid content of U.S. foods, see the 1998 carotenoid database created by the U.S. Department of Agriculture and the Nutrition Coordinating Center at the University of Minnesota (http://www.nal.usda.gov/fnic/foodcomp/Data/car98/car98.html). Vitamin A, found in foods that come from animal sources, is called preformed vitamin A. Some carotenoids found in colorful fruits and vegetables are called provitamin A; they are metabolized in the body to vitamin A. Among the carotenoids, beta-carotene, a retinol dimer, has the most significant provitamin A activity. -
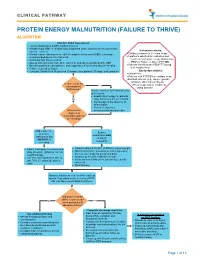
Protein Energy Malnutrition (Failure to Thrive) Algorithm
CLINICAL PATHWAY PROTEIN ENERGY MALNUTRITION (FAILURE TO THRIVE) ALGORITHM Conduct Initial Assessment • History and physical (H&P), nutrition focused • Weight height, BMI, % of ideal body weight and exam: assess severity (symmetric edema = severe) Inclusion criteria: • • Consider basic labs based on H&P; A complete blood count (CBC) is strongly Children newborn to 21 years of age • recommended due to risk of anemia Inpatients admitted for evaluation and • Additional labs based on H&P treatment of Protein Energy Malnutrition • Assess micronutrients: iron, zinc, vitamin D, and others as indicated by H&P (PEM) or Failure to thrive (FTT) OR • • Baseline potassium, phosphorus, and magnesium if concerned about re-feeding Patients identified with PEM/FTT during • Calorie count up to 3 days their hospital stay. • Consults: Social Work, Registered Dietician, Occupational Therapy, and Lactation Exclusion criteria: • Outpatients • Patients with FTT/PEM secondary to an identified concern (e.g., cancer, genetic condition, other chronic illness). Is there a risk for •Pts w/ suspected or confirmed micronutrient Yes eating disorder deficiencies? Initiate treatment for micronutrients deficiencies: • Empiric zinc therapy for patients No older than 6 months for 1 month • Iron therapy in the absence of inflammation • Vitamin D and other What are the micronutrients based on labs degrees of malnutrition and risk of refeeding? Mild, moderate, Severe or severe malnutrition AND malnutrition but at risk of NO RISK of refeeding refeeding • • Initiate feeding per recommended Initiate feeding at 30-50% of RDA for current weight • daily allowance (RDA) for current Monitor potassium, phosphorus, and magnesium weight and age once to twice a day for a total of 4 days • • Use PO route if patient is able to Advance by 10-20% if labs are normal • take 70% of estimated calories If labs abnormal hold off on advancing feed until orally corrected • Start thiamine Advance calories to meet level for catch up growth. -

Nutritional Dermatoses in the Hospitalized Patient
HOSPITAL CONSULT IN PARTNERSHIP WITH THE SOCIETY FOR DERMATOLOGY HOSPITALISTS Nutritional Dermatoses in the Hospitalized Patient Melissa Hoffman, MS; Robert G. Micheletti, MD; Bridget E. Shields, MD Nutritional deficiencies may arise from inadequate nutrient intake, abnormal nutrient absorption, or improper nutrient PRACTICE POINTS utilization.4 Unfortunately, no standardized algorithm for • Nutritional deficiencies are common in hospitalized screening and diagnosing patients with malnutrition exists, patients and often go unrecognized. making early physical examination findings of utmost • Awareness of the risk factors predisposing patients importance. Herein, we present a review of acquired nutri- to nutritional deficiencies and the cutaneous manifes- tional deficiency dermatoses in the inpatient setting. tations associated with undernutrition can promote copy early diagnosis. Protein-Energy Malnutrition • When investigating cutaneous findings, undernutri- tion should be considered in patients with chronic Protein-energy malnutrition (PEM) refers to a set of infections, malabsorptive states, psychiatric illness, related disorders that include marasmus, kwashiorkor and strict dietary practices, as well as in those using (KW), and marasmic KW. These conditions frequently are certain medications. seen in developing countries but also have been reported 5 • Prompt nutritional supplementation can prevent patient in developed nations. Marasmus occurs from a chronic morbidity and mortality and reverse skin disease. deficiencynot of protein and calories. Decreased insulin pro- duction and unopposed catabolism result in sarcopenia and loss of bone and subcutaneous fat.6 Affected patients include children who are less than 60% ideal body weight Cutaneous disease may be the first manifestation of an underlying nutri- 7 tional deficiency, highlighting the importance of early recognition by der- (IBW) without edema or hypoproteinemia. -

Vitamin a Information Vitamin a Deficiency (VAD) Is the Leading
Vitamin A Information Vitamin A deficiency (VAD) is the leading cause of preventable blindness in children. Xerophthalmia, which is abnormal dryness of the conjunctiva and cornea of the eye, is associated with VAD and when left untreated can lead to blindness. The World Health Organization estimates that worldwide there are “at least 254 million children under the age of five that are at-risk in terms of their health and survival”. An estimated 250,000 to 500,000 vitamin A deficient children become blind each year. Half of these children die within 12 months of losing their sight. Although this problem is most prevalent in Africa and South East Asia, it is certainly existent throughout the developing nations. According to UNICEF, “Of 82 countries deemed ‘priorities’ for national-level vitamin A supplementation programs, 57 had coverage estimates available for 2014. Half of these 57 countries achieved the recommended coverage of 80 percent.” As a result, half did not receive the 80 percent level, and for those that did, a significant number of children remained untreated. While the problem is most prevalent in Africa and South East Asia, central American countries are also at risk. “About 40% of Mexican children in rural areas had deficient values of plasma vitamin A” (Rosado, 1995). Furthermore, it was noted as far back as 1989 that vitamin A deficient Guatemalan children grow poorly, are more anemic, have more infections and are more likely to die than their peers (Sommer, 1989). The World Health Organization recommends that all children between the ages of six months and six years in developing nations that are at risk receive vitamin A supplementation. -

A Case of Kwashiorkor Presenting with Pericardial Effusion
orts & Ca Taheri et al., Med Rep Case Stud 2017, 2:2 ep se R S l t a u DOI: 10.4172/2572-5130.1000134 c d i i d e s e M + Medical Reports & Case Studies ISSN: 2572-5130 CaseResearch Report Article Open Access A Case of Kwashiorkor Presenting with Pericardial Effusion Taheri S*, Surak A, Bravo G, McMurray A and Altamirano-Diaz L Department of Paediatrics, Children’s Hospital, London Health Sciences Centre, Western University, London, UK Abstract Introduction: Kwashiorkor is a type of protein-calorie malnutrition often seen in children of impoverished countries and famine. It is a result of insufficient protein intake in the context of adequate caloric intake. Case report: We report a case of a 13-year-old male with trisomy 21 in Southwestern Ontario, Canada who presented with bilateral pneumonia, pericardial effusion and peripheral edema. Evaluation revealed severe dietary restriction, consistent with kwashiorkor. Child was placed on severely restrictive diet, particularly limiting dairy intake to one daily cup of plain, unfortified yogurt. His hospital course was complicated with severe hypocalcemia, hypomagnesemia and hypophosphatemia. These findings resolved gradually upon slow introduction of well-balanced diet and adequate caloric and protein intake. Conclusion: Malnutrition is often underdiagnosed or misdiagnosed in developed countries with devastating outcomes if unrecognized. This makes it imperative to consider this diagnosis, recognize potential risk factors and be prepared to accurately assess overall nutritional status. Keywords: Malnutrition; Kwashiorkor; Case report; pneumonia; in Canada. He is the first child born to parents of East Indian descent Respiratory; Pericardial effusion (unknown exact geographic region). -

Serum and Red Cell Folates, and Serum Vitamin B12 in Protein Calorie Malnutrition
Arch Dis Child: first published as 10.1136/adc.48.5.366 on 1 May 1973. Downloaded from Archives of Disease in Childhood, 1973, 48, 366. Serum and red cell folates, and serum vitamin B12 in protein calorie malnutrition M. KHALIL, A. TANIOS, M. MOGHAZY, M. K. AREF, S. MAHMOUD, and M. EL LOZY From the Departments of Paediatrics, Clinical Pathology, and Physiology, Faculty of Medicine, University of Alexandria, Alexandria, Egypt Khalil, M., Tanios, A., Moghazy, M., Aref, M. K., Mahmoud, S., and el Lozy, M. (1973). Archives of Disease in Childhood, 48, 366. Serum and red cell folates, and serum vitamin B12 in protein calorie malnutrition. In 22 cases of kwashiorkor, 19 cases of marasmus, and 16 normal controls, red cell folate, serum folate, and serum vitamin B1, were estimated, and the bone marrow and peripheral blood examined. Erythrocyte folate deficiency was shown in 9 cases of kwashiorkor and 7 cases of marasmus. Serum folate deficiency was present in 14 cases of kwashi- orkor and 7 cases of marasmus. Megaloblastosis was found in 45% of cases of kwashiorkor and 37% of cases of marasmus. Megaloblastosis and macrocytosis correlated more with erythrocyte than with serum folate deficiency. Serum vitamin B1, levels in children with kwashiorkor or marasmus did not differ from those of normal controls. The role of folate deficiency in the pathogenesis of megaloblastosis in protein calorie malnutrition was confirmed. copyright. A hypochromic anaemia of iron deficiency is a Material and methods salient finding in patients with protein calorie The study was carried out on 22 infants (12 males and malnutrition (Khalil, Awwad, and Hafez, 1968). -

A Child with Kwashiorkor Misdiagnosed As Atopic Dermatitis
Volume 23 Number 5 | May 2017 Dermatology Online Journal || Letter DOJ 23 (5): 17 A child with kwashiorkor misdiagnosed as atopic dermatitis Marcus Henrique de S B Xavier MD, MsC, Eduardo de Magalhães MD, Gilmar Ferraz Oliveira MD, Mariana Keltke Magalhães MD, Cláudio Prates de Almeida e Oliveira MD, Natália Bragança Oliveira MD Affiliations: Hospital Infantil Padre Anchieta, Belo Horizonte, Minas Gerais, Brazil Corresponding Author: Marcus H. Xavier,MD, MSC, 465 Mangabeira street, Suite 601, Belo Horizonte, MG 30350-170, Brazil, Email: marcus_ [email protected] Abstract The condition is a type of protein-calorie malnutrition most often seen in children of impoverished countries Although uncommon, kwashiorkor continues to occur or areas of famine. Causes are controversial, but the in developed, but mainly in developing nations. It is a most commonly accepted theory is inadequate type of protein-calorie malnutrition that occurs in the dietary protein in the presence of sufficient caloric setting of insufficient protein intake in the presence of intake [1-4]. Children placed on restrictive diets by sufficient caloric intake. Skin and hair changes should ‘‘well-intending’’ parents, as a result of concern for prompt a thorough dietary history and appropriate food allergies, have been reported to be previously dietary intervention. We report a case of a 12-month- at risk of nutritional deficiency, such as kwashiorkor old girl in Belo Horizonte, Minas Gerais, Brazil, who [3, 4]. presented with diffuse edema, desquamation, and irritability misdiagnosed as atopic dermatitis. The Case Synopsis diagnosis was consistent with kwashiorkor as a result A 12-month-old girl presented with a 3-month of severe dietary restriction. -

Micronutrient Malnutrition – Detection, Measurement and Intervention: a Training Package for Field Staff Handouts for Group Tr
Micronutrient Malnutrition – Detection, Measurement and Intervention: A Training Package for Field Staff Compiled by the Institute of Child Health Handouts for Group Training For UNHCR Version 1 2003 ICH/UNHCR Handout Contents Section 1: Section 2: Section 3: Important Micronutrient Detection Nutrition Concepts Deficiency Diseases and Prevention 1. Food and Nutrition 1. Anaemia 1. Detection of Deficiencies 2. Nutritional Requirements 2. Vitamin A Deficiency 2. Intervention 3. Nutritional Deficiencies 3. Iodine Deficiency Disorders 4. Micronutrient Deficiency Disease 4. Beriberi 5. Nutritional Assessments 5. Ariboflavinosis 6. Causes of Malnutrition 6. Pellagra 7. Scurvy 8. Rickets ICH/UNHCR Handout 2 Section 1 Food and Nutrition • All people and animals need food to live, grow and be healthy. • Food contains different types of nutrients. • Food contains certain nutrients called macronutrients: – Fat – Carbohydrate – Protein • Food also contains nutrients called micronutrients: – Vitamins – Minerals • A good diet is made up of foods that contain all these types of nutrients – macronutrients and micronutrients. ICH/UNHCR Handout 3 Section 1 Nutritional Requirements For people to be healthy and productive they need a certain amount of nutrients. This is called their nutritional requirement. • The amount of energy that people get from their food is measured in kilo calories (kcal). • The average person needs about 2100 kcal each day • 17-20 % of this energy should come from fat • At least 10 % of this energy should come from protein • People also need certain amounts of vitamins and minerals • For example the average person should have at least 12 mg of the B vitamin niacin, 28 mg of vitamin C, and 22 mg of iron each day. -

Kwashiorkor in Africa * J
Bull. Org. mond. Sante 1952, 5, 1-71 Bull. World Hlth Org. KWASHIORKOR IN AFRICA * J. F. BROCK, D.M., F.R.C.P. Professor of the Practice of Medicine, University of Cape Town, Union of South Africa Consultant in Nutrition, World Health Organization M. AUTRET, Dr Pharm. Chief, Area and Field Branch, Nutrition Division, Food and Agriculture Organization Manuscript received in July 1951 Page Introduction ...... .. .. .. .. 2 1. Medical aspects of kwashiorkor ..... 5 1.1 Definition, and description of individual clinical characters .5... S 1.2 General clinical picture ..... 24 1.3 Nutritional cirrhosis and primary carcinoma of the liver .... 25 1.4 Frequency of the syndrome ..... 27 1.5 Treatment ....... .. .. .. .. .. 28 2. Kwashiorkor and diet ..... 29 2.1 Food consumption and feeding practices ... 29 2.2 Relation between kwashiorkor and diet .... 39 3. Etiology of kwashiorkor ..... 47 4. Prevention of kwashiorkor ..... 51 4.1 Increasing the supply of proteins ..... 51 4.2 The hungry months ...... 56 4.3 Supplementary feeding of infants and young children .... 57 4.4 Education ....... .. .. .. .. .. 59 4.5 Immediate action ...... .. 60 Recommendations ...... .. 60 Summary Resume|62 . Annex 1. Recent and current clinical and biochemical studies in Africa 65 References ....... .. .. .. .. .. .. .. .. 69 * This paper will also be published, in English and in French, in the Monograph Series of the World Health Organization. it was published in Spanish by the Food and Agriculture Organizatian of the United Nations, in September 1951, as FAQ - Estudios de Nutricidn, No. 8. - ED. 102 - 1 - 2 J. F. BROCK & M. AUTRET INTRODUCTION This report is the result of a recommendation made by the Joint FAO/WHO Expert Committee on Nutrition at its first session in Geneva in October 1949.