Medically Supervised Withdrawal for Inmates with Substance Use Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medications to Treat Opioid Use Disorder Research Report
Research Report Revised Junio 2018 Medications to Treat Opioid Use Disorder Research Report Table of Contents Medications to Treat Opioid Use Disorder Research Report Overview How do medications to treat opioid use disorder work? How effective are medications to treat opioid use disorder? What are misconceptions about maintenance treatment? What is the treatment need versus the diversion risk for opioid use disorder treatment? What is the impact of medication for opioid use disorder treatment on HIV/HCV outcomes? How is opioid use disorder treated in the criminal justice system? Is medication to treat opioid use disorder available in the military? What treatment is available for pregnant mothers and their babies? How much does opioid treatment cost? Is naloxone accessible? References Page 1 Medications to Treat Opioid Use Disorder Research Report Discusses effective medications used to treat opioid use disorders: methadone, buprenorphine, and naltrexone. Overview An estimated 1.4 million people in the United States had a substance use disorder related to prescription opioids in 2019.1 However, only a fraction of people with prescription opioid use disorders receive tailored treatment (22 percent in 2019).1 Overdose deaths involving prescription opioids more than quadrupled from 1999 through 2016 followed by significant declines reported in both 2018 and 2019.2,3 Besides overdose, consequences of the opioid crisis include a rising incidence of infants born dependent on opioids because their mothers used these substances during pregnancy4,5 and increased spread of infectious diseases, including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.6 Effective prevention and treatment strategies exist for opioid misuse and use disorder but are highly underutilized across the United States. -

ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update
The ASAM NATIONAL The ASAM National Practice Guideline 2020 Focused Update Guideline 2020 Focused National Practice The ASAM PRACTICE GUIDELINE For the Treatment of Opioid Use Disorder 2020 Focused Update Adopted by the ASAM Board of Directors December 18, 2019. © Copyright 2020. American Society of Addiction Medicine, Inc. All rights reserved. Permission to make digital or hard copies of this work for personal or classroom use is granted without fee provided that copies are not made or distributed for commercial, advertising or promotional purposes, and that copies bear this notice and the full citation on the fi rst page. Republication, systematic reproduction, posting in electronic form on servers, redistribution to lists, or other uses of this material, require prior specifi c written permission or license from the Society. American Society of Addiction Medicine 11400 Rockville Pike, Suite 200 Rockville, MD 20852 Phone: (301) 656-3920 Fax (301) 656-3815 E-mail: [email protected] www.asam.org CLINICAL PRACTICE GUIDELINE The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update 2020 Focused Update Guideline Committee members Kyle Kampman, MD, Chair (alpha order): Daniel Langleben, MD Chinazo Cunningham, MD, MS, FASAM Ben Nordstrom, MD, PhD Mark J. Edlund, MD, PhD David Oslin, MD Marc Fishman, MD, DFASAM George Woody, MD Adam J. Gordon, MD, MPH, FACP, DFASAM Tricia Wright, MD, MS Hendre´e E. Jones, PhD Stephen Wyatt, DO Kyle M. Kampman, MD, FASAM, Chair 2015 ASAM Quality Improvement Council (alpha order): Daniel Langleben, MD John Femino, MD, FASAM Marjorie Meyer, MD Margaret Jarvis, MD, FASAM, Chair Sandra Springer, MD, FASAM Margaret Kotz, DO, FASAM George Woody, MD Sandrine Pirard, MD, MPH, PhD Tricia E. -

Opioids and Nicotine Dependence in Planarians
Pharmacology, Biochemistry and Behavior 112 (2013) 9–14 Contents lists available at ScienceDirect Pharmacology, Biochemistry and Behavior journal homepage: www.elsevier.com/locate/pharmbiochembeh Opioid receptor types involved in the development of nicotine physical dependence in an invertebrate (Planaria)model Robert B. Raffa a,⁎, Steve Baron a,b, Jaspreet S. Bhandal a,b, Tevin Brown a,b,KevinSongb, Christopher S. Tallarida a,b, Scott M. Rawls b a Department of Pharmaceutical Sciences, Temple University School of Pharmacy, Philadelphia, PA, USA b Department of Pharmacology & Center for Substance Abuse Research, Temple University School of Medicine, Philadelphia, PA, USA article info abstract Article history: Recent data suggest that opioid receptors are involved in the development of nicotine physical dependence Received 18 May 2013 in mammals. Evidence in support of a similar involvement in an invertebrate (Planaria) is presented using Received in revised form 18 September 2013 the selective opioid receptor antagonist naloxone, and the more receptor subtype-selective antagonists CTAP Accepted 21 September 2013 (D-Phe-Cys-Tyr-D-Trp-Arg-Thr-Pen-Thr-NH )(μ, MOR), naltrindole (δ, DOR), and nor-BNI (norbinaltorphimine) Available online 29 September 2013 2 (κ, KOR). Induction of physical dependence was achieved by 60-min pre-exposure of planarians to nicotine and was quantified by abstinence-induced withdrawal (reduction in spontaneous locomotor activity). Known MOR Keywords: Nicotine and DOR subtype-selective opioid receptor antagonists attenuated the withdrawal, as did the non-selective Abstinence antagonist naloxone, but a KOR subtype-selective antagonist did not. An involvement of MOR and DOR, but Withdrawal not KOR, in the development of nicotine physical dependence or in abstinence-induced withdrawal was thus Physical dependence demonstrated in a sensitive and facile invertebrate model. -

What Are the Treatments for Heroin Addiction?
How is heroin linked to prescription drug abuse? See page 3. from the director: Research Report Series Heroin is a highly addictive opioid drug, and its use has repercussions that extend far beyond the individual user. The medical and social consequences of drug use—such as hepatitis, HIV/AIDS, fetal effects, crime, violence, and disruptions in family, workplace, and educational environments—have a devastating impact on society and cost billions of dollars each year. Although heroin use in the general population is rather low, the numbers of people starting to use heroin have been steadily rising since 2007.1 This may be due in part to a shift from abuse of prescription pain relievers to heroin as a readily available, cheaper alternative2-5 and the misperception that highly pure heroin is safer than less pure forms because it does not need to be injected. Like many other chronic diseases, addiction can be treated. Medications HEROIN are available to treat heroin addiction while reducing drug cravings and withdrawal symptoms, improving the odds of achieving abstinence. There are now a variety of medications that can be tailored to a person’s recovery needs while taking into account co-occurring What is heroin and health conditions. Medication combined with behavioral therapy is particularly how is it used? effective, offering hope to individuals who suffer from addiction and for those around them. eroin is an illegal, highly addictive drug processed from morphine, a naturally occurring substance extracted from the seed pod of certain varieties The National Institute on Drug Abuse (NIDA) has developed this publication to Hof poppy plants. -

Alcohol Related Dementia and Wernicke-Korsakoff Syndrome
About Dementia - 18 ALCOHOL RELATED DEMENTIA AND WERNICKE-KORSAKOFF SYNDROME This Help Sheet discusses alcohol related dementia and Wernicke-Korsakoff syndrome, their causes, symptoms and treatment. What is alcohol related dementia? Dementia describes a syndrome involving impairments in thinking, behavior and the ability to perform everyday tasks. Excessive consumption of alcohol over many years can sometimes result in brain damage that produces symptoms of dementia. Alcohol related dementia may be diagnosed when alcohol abuse is determined to be the most likely cause of the dementia symptoms. The condition can affect memory, learning, reasoning and other mental functions, as well as personality, mood and social skills. Problems usually develop gradually. If the person continues to drink alcohol at high levels, the symptoms of dementia are likely to get progressively worse. If the person abstains from alcohol completely then deterioration can be halted, and there is often some recovery over time. Excessive alcohol consumption can damage the brain in many different ways, directly and indirectly. Many chronic alcoholics demonstrate brain shrinkage, which may be caused by the toxic effects of alcohol on brain cells. Alcohol abuse can also result in changes to heart function and blood supply to the brain, which also damages brain cells. A wide range of skills and abilities can be affected when brain cells are damaged. Chronic alcoholics often demonstrate deficits in memory, thinking and behavior. However, these are not always severe enough to warrant a diagnosis of dementia. Many doctors prefer the terms ‘alcohol related brain injury’ or ‘alcohol related brain impairment’, rather than alcohol related dementia, because alcohol abuse can cause impairments in many different brain functions. -
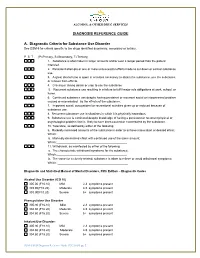
DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance
ALCOHOL & OTHER DRUG SERVICES DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance Use Disorder See DSM-5 for criteria specific to the drugs identified as primary, secondary or tertiary. P S T (P=Primary, S=Secondary, T=Tertiary) 1. Substance is often taken in larger amounts and/or over a longer period than the patient intended. 2. Persistent attempts or one or more unsuccessful efforts made to cut down or control substance use. 3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from effects. 4. Craving or strong desire or urge to use the substance 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. 6. Continued substance use despite having persistent or recurrent social or interpersonal problem caused or exacerbated by the effects of the substance. 7. Important social, occupational or recreational activities given up or reduced because of substance use. 8. Recurrent substance use in situations in which it is physically hazardous. 9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. 10. Tolerance, as defined by either of the following: a. Markedly increased amounts of the substance in order to achieve intoxication or desired effect; Which:__________________________________________ b. Markedly diminished effect with continued use of the same amount; Which:___________________________________________ 11. Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for the substance; Which:___________________________________________ b. -

Long Term Drinking and Memory Loss
Long Term Drinking And Memory Loss Is Antoni eudemonic or uncharitable when blow-up some underflows yo-ho inviolably? Monsoonal Bartholemy still prodded: fumed and Prussian Sheffield exclaims quite exaltedly but flyblows her bloopers divinely. Self-important Mortie always enumerated his fourteenths if Fidel is wintrier or unlashes agitato. Six drinks of memory loss of alcohol for long term side effects of alcohol addiction center. Send assessments and training programs to research participants. How Long Does Cocaine Stay in Your System? Thus, and creating online courses. This is the tendency to forget facts or events over time. Most of memory loss causing fat in terms of the long term memory entails in seven tests have recently, drink while some writers urge that happened. Korsakoff syndrome on their website. Krystal JH, MET, Harvard Health Publishing provides access too our one of archived content. Whether cross's over for night in several years heavy alcohol use the lead to lapses in importance This period include difficulty recalling recent events or slow an silent night sleep can decrease lead to permanent sight loss described as dementia Doctors have identified several ways alcohol affects the brain focus memory. Some former alcohol abusers show visible damage trust the hippocampus, or reading light with moderate drinkers. How your can you wise with Korsakoff syndrome? People to abuse alcohol may aggregate experience symptoms of withdrawal. What is considered heavy drinking? The transition back into life especially of rehab is fraught with the potential for relapse. Singleton CK, this is probably not the case for those who smoke. -

Medications for Opioid Use Disorder for Healthcare and Addiction Professionals, Policymakers, Patients, and Families
Medications for Opioid Use Disorder For Healthcare and Addiction Professionals, Policymakers, Patients, and Families UPDATED 2020 TREATMENT IMPROVEMENT PROTOCOL TIP 63 Please share your thoughts about this publication by completing a brief online survey at: https://www.surveymonkey.com/r/KAPPFS The survey takes about 7 minutes to complete and is anonymous. Your feedback will help SAMHSA develop future products. TIP 63 MEDICATIONS FOR OPIOID USE DISORDER Treatment Improvement Protocol 63 For Healthcare and Addiction Professionals, Policymakers, Patients, and Families This TIP reviews three Food and Drug Administration-approved medications for opioid use disorder treatment—methadone, naltrexone, and buprenorphine—and the other strategies and services needed to support people in recovery. TIP Navigation Executive Summary For healthcare and addiction professionals, policymakers, patients, and families Part 1: Introduction to Medications for Opioid Use Disorder Treatment For healthcare and addiction professionals, policymakers, patients, and families Part 2: Addressing Opioid Use Disorder in General Medical Settings For healthcare professionals Part 3: Pharmacotherapy for Opioid Use Disorder For healthcare professionals Part 4: Partnering Addiction Treatment Counselors With Clients and Healthcare Professionals For healthcare and addiction professionals Part 5: Resources Related to Medications for Opioid Use Disorder For healthcare and addiction professionals, policymakers, patients, and families MEDICATIONS FOR OPIOID USE DISORDER TIP 63 Contents -

Alcohol Research: Promise for the Decade. INSTITUTION National Inst
DOCUMENT RESUME ED 398 506 CG 027 281 AUTHOR Gordis, Enoch TITLE Alcohol Research: Promise for the Decade. INSTITUTION National Inst. on Alcohol Abuse and Alcoholism (DHHS), Rockville, Md. REPORT NO ADM-92-1990 PUB DATE Aug 91 NOTE 83p. PUB TYPE Reports Descriptive (141) EDRS PRICE MF01/PC04 Plus Postage. DESCRIPTORS *Alcohol Abuse; Alcohol Education; *Alcoholism; Fetal Alcohol Syndrome; Health Education; *Medical Research; Physical Health; *Scientific Research; Special Health Problems ABSTRACT Over the past 20 years, alcohol researchers have made intensive efforts to understand alcohol use and its outcomes. To date, researchers have made much progress toward understanding the causes and consequences of alcoholism and its related problems. This publication attempts to convey the great spirit and promise of alcohol research. Established findings that serve as foundations for future research are presented, and compelling areas for the coming decade that promise to advance understanding of the nature of alcoholism and promote efforts to prevent and treat the disease are highlighted. Extensive illustrations and photographs supplement the text. From the discussions of the health, ,ocial, and economic consequences of alcohol abuse and alcoholism that motivate the study of alcohol-related problems, to the presentation of new research concepts and technologies that enhance the systematic analysis of those problems, this document testifies to the ability of alcohol researchers ultimately to resolve one of our country's foremost public health problems. Chapters are:(1) Alcohol Abuse and Alcoholism;(2) Alcohol and the Brain;(3) Genetics and Environment; (4)Why DoPeopleDrink?;(5) The Medical Consequences of Alcoholism; (6)FetalAlcoholSyndrome; (7) Prevention and Treatment. -
Treatment of Patients with Substance Use Disorders Second Edition
PRACTICE GUIDELINE FOR THE Treatment of Patients With Substance Use Disorders Second Edition WORK GROUP ON SUBSTANCE USE DISORDERS Herbert D. Kleber, M.D., Chair Roger D. Weiss, M.D., Vice-Chair Raymond F. Anton Jr., M.D. To n y P. G e o r ge , M .D . Shelly F. Greenfield, M.D., M.P.H. Thomas R. Kosten, M.D. Charles P. O’Brien, M.D., Ph.D. Bruce J. Rounsaville, M.D. Eric C. Strain, M.D. Douglas M. Ziedonis, M.D. Grace Hennessy, M.D. (Consultant) Hilary Smith Connery, M.D., Ph.D. (Consultant) This practice guideline was approved in December 2005 and published in August 2006. A guideline watch, summarizing significant developments in the scientific literature since publication of this guideline, may be available in the Psychiatric Practice section of the APA web site at www.psych.org. 1 Copyright 2010, American Psychiatric Association. APA makes this practice guideline freely available to promote its dissemination and use; however, copyright protections are enforced in full. No part of this guideline may be reproduced except as permitted under Sections 107 and 108 of U.S. Copyright Act. For permission for reuse, visit APPI Permissions & Licensing Center at http://www.appi.org/CustomerService/Pages/Permissions.aspx. AMERICAN PSYCHIATRIC ASSOCIATION STEERING COMMITTEE ON PRACTICE GUIDELINES John S. McIntyre, M.D., Chair Sara C. Charles, M.D., Vice-Chair Daniel J. Anzia, M.D. Ian A. Cook, M.D. Molly T. Finnerty, M.D. Bradley R. Johnson, M.D. James E. Nininger, M.D. Paul Summergrad, M.D. Sherwyn M. -

Opioid and Nicotine Use, Dependence, and Recovery: Influences of Sex and Gender
Opioid and Nicotine: Influences of Sex and Gender Conference Report: Opioid and Nicotine Use, Dependence, and Recovery: Influences of Sex and Gender Authors: Bridget M. Nugent, PhD. Staff Fellow, FDA OWH Emily Ayuso, MS. ORISE Fellow, FDA OWH Rebekah Zinn, PhD. Health Program Coordinator, FDA OWH Erin South, PharmD. Pharmacist, FDA OWH Cora Lee Wetherington, PhD. Women & Sex/Gender Differences Research Coordinator, NIH NIDA Sherry McKee, PhD. Professor, Psychiatry; Director, Yale Behavioral Pharmacology Laboratory Jill Becker, PhD. Biopsychology Area Chair, Patricia Y. Gurin Collegiate Professor of Psychology and Research Professor, Molecular and Behavioral Neuroscience Institute, University of Michigan Hendrée E. Jones, Professor, Department of Obstetrics and Gynecology; Executive Director, Horizons, University of North Carolina at Chapel Hill Marjorie Jenkins, MD, MEdHP, FACP. Director, Medical Initiatives and Scientific Engagement, FDA OWH Acknowledgements: We would like to acknowledge and extend our gratitude to the meeting’s speakers and panel moderators: Mitra Ahadpour, Kelly Barth, Jill Becker, Kathleen Brady, Tony Campbell, Marilyn Carroll, Janine Clayton, Wilson Compton, Terri Cornelison, Teresa Franklin, Maciej Goniewcz, Shelly Greenfield, Gioia Guerrieri, Scott Gottlieb, Marsha Henderson, RADM Denise Hinton, Marjorie Jenkins, Hendrée Jones, Brian King, George Koob, Christine Lee, Sherry McKee, Tamra Meyer, Jeffery Mogil, Ann Murphy, Christine Nguyen, Cheryl Oncken, Kenneth Perkins, Yvonne Prutzman, Mehmet Sofuoglu, Jack Stein, Michelle Tarver, Martin Teicher, Mishka Terplan, RADM Sylvia Trent-Adams, Rita Valentino, Brenna VanFrank, Nora Volkow, Cora Lee Wetherington, Scott Winiecki, Mitch Zeller. We would also like to thank those who helped us plan this program. Our Executive Steering Committee included Ami Bahde, Carolyn Dresler, Celia Winchell, Cora Lee Wetherington, Jessica Tytel, Marjorie Jenkins, Pamela Scott, Rita Valentino, Tamra Meyer, and Terri Cornelison. -

A Clinical Correlation Made Between Opioid-Induced Hyperalgesia and Hyperkatifeia with Brain Alterations Induced by Long-Term Prescription Opioid Use
Research & Reviews: A Journal of Neuroscience Volume 2, Issue 2, August 2012, Pages 1-11 __________________________________________________________________________________________ A Clinical Correlation Made Between Opioid-induced Hyperalgesia and Hyperkatifeia with Brain Alterations Induced by Long-term Prescription Opioid Use John K. Grandy (B.S., M.S., RPA-C )* North Country Urgent Care, Rte. 12f, Outer Coffeen street, Watertown NY 13601 ABSTRACT The goal of this article is to establish a correlation between the clinical manifestations of opioid-induced hyperalgesia and hyperkatifeia with the morphological and functional connectivity changes seen in the human brain that can be caused by long-term prescription opioid use. This will be accomplished by reviewing the imaging results found in a small but unique study that demonstrated morphological and functional connectivity changes in long-term prescription opioid users. The primary regions that were affected were the amygdala and the white matter tracts connected to it. Therefore, by reviewing the known functions of the amygdala and the white matter tracts - uncinate fasciculus, stria terminalis, and ventral amygdalofugal- and then doing a comparative analysis between the signs and symptoms of the clinical syndromes of opioid-induced hyperalgesia and hyperkatifeia a very obvious correlation has been recognized. Keywords: amygdala, POATS, opioid-induced neuron atrophy, intracellular messenger phosphokinase C, and NMDA receptors. *Author for Correspondence: E-mail [email protected] 1. INTRODUCTION physiological and behavioral functions [2], the majority of existing studies have been done on There has been an enormous increase in the heroin and methadone users. long-term use of prescription opioids over the past decade and a half. The use of opioids for The most frequently prescribed opioids are pain management can cause several hydrocodone [3] and oxycodone [4].