Distributed Healthcare Framework Using Patient-Centric Role-Based Security Modelling and Workflow
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Civil Syllabus 1St &
Diploma in Civil Engineering 2020-21 C20 Vision [(To be drafted individually at institution level)] Develop global civil engineering professionals who serve competently, collaboratively, and ethically as master to create a sustainable world and enhance the global quality of life Mission (To be drafted individually at institution level) M1:To develop a specialized professional by imparting quality education and practical training in collaboration with industry, through competitive curriculum M2:To develop professionally skilled and ethical planners, designers, constructors, and operators of society’s economic and social engine M3: To develop leadership skills in discussions and decisions shaping public environmental and infrastructure policy M4:To nurture innovators and integrators as entrepreneurs of ideas and technology across the public, private, and academic sectors Programme Educational Objectives (PEOs) (To be drafted individually at institution level) (After 2/3 years of graduation, the students will have the ability to) Civil Engineering Programme is committed to transform students into competent professionals, responsible citizens. On completing the diploma programme, the students should have acquired the following characteristics. To apply technical knowledge in analyzing problems in the field of Civil PEO1 Engineering, in the view of ensuring maximization of economic benefits to society and minimization of damage to ecology and environment. To enhance entrepreneurial, communication and other soft skills, which will enable them to work globally as leaders, team members and contribute to nation PEO2 building for the betterment of the societywithout overexploitation of natural resources. To make them strongly committed to the highest levels of professional ethics and PEO3 focus on ensuring quality, adherence to public policy and law, safety, reliability and environmental sustainability in all their professional activities. -

Case Studies of Transitional Korean Adolescents' Literacy Practices
Different Literacies in Different Contexts of Use: Case Studies of Transitional Korean Adolescents’ Literacy Practices DISSERTATION Presented in partial fulfillment of the requirements for the Degree doctor of Philosophy in the Graduate School of The Ohio State University Jeongsoo Pyo, MA TESL Graduate Program in Education The Ohio State University 2015 Dissertation Committee: Professor Alan Hirvela, advisor Professor Youngjoo Yi Professor Francis Troyan ii Copyright by Jeongsoo Pyo 2015 iii Abstract As new technology has changed adolescents’ literate life pathways outside school in remarkable ways, new uses of terminology, such as “mutiliteracies” (The New London Group, 1996), are necessary to capture the multi-dimensional nature of current encounters with what was long called “literacy,” a term that reflects a more limited presence in a print- mediated environment. However, there has been relatively little interest in the multliteracies experiences of Korean adolescents in the U.S., especially I the framing of them as transitional youth. This study asserts that the term “transitional youth” best captures the nature of their movement from the native language and culture they are moving from to a very new language and culture. This study examined the literacy practices of transitional Korean adolescents across three contexts—school, home, and community— from a sociocultural perspective. I conducted multiple case studies of three transitional Korean adolescents in a Midwestern city in the U.S. Over a six month period, I used multiple approaches -

Blogs, Wikis, Webcasts
Blogs, Wikis, Webcasts: Utilization of State-of-the-Art Communication Instruments for Project Management Simone Happ, PMP, Program Manager, T-Systems Multimedia Solutions GmbH Anett Wünsche, PMP, Project Management Office, T-Systems Multimedia Solutions GmbH Dirk Röhrborn, PMP, CEO, Communardo GmbH Falk Henkel, PMP, Head of Innovation & Internationalization, T-Systems Multimedia Solutions GmbH Introduction As information technology is evolving communication behaviour is changing. Today, project communication is based on tools like e-mail, shared document folders or project management software. Thereby the internet is a crucial source for information gathering as well as for information exchange. Web 2.0 marks a new internet generation where applications are easy to use, accessible for anybody and covering nearly every information area. Its technologies and services influence and change private and business communication. The paper analyses impacts on and opportunities for the special area of project communication. Web 2.0 Paradigm Shift Web 2.0 is used for a new paradigm of web applications. Whereas Web 1.0 focused on information distribution mainly driven by universities, research institutes, and more or less large companies, Web 2.0 improved accessibility and easiness of use so that communication and collaboration are core value. O’Reilly who designed the phrase in 2004 lists design patterns which explain the paradigm change (O’Reilly, 2005). An example can be shown in the field of e-commerce. A classical web shop is driven by a central seller; and he lists his products with prices. Added Web 2.0 functionality is well-known from E-Bay.com or Amazon.com. -

Construction Manual
Mississippi Department of Transportation Construction Manual INTRODUCTION This manual has been prepared to inform and assist construction inspection personnel in the performance of their duties and in the documentation of project activities. This is not a specification document and its content is not legally binding upon any Department contract and should be recognized as a guide only. Reference to certain sections of the Standard Specifications appear throughout in order to relate certain inspection activities to an applicable section of the Standard Specification. Recognizing that any manual of this type must undergo continuous revisions, each recipient is encouraged to submit suggested changes through appropriate channels to the Construction Division. Approved changes, additions, or deletions will be issued as the need arises. Each recipient of the Construction Manual is responsible for keeping the contents of their copy up to date. Revisions will be posted on the Construction Division Intranet site. This Construction Manual is presented with the sincere belief that it will aid in maintaining the high- quality construction standards which have been established over the years by the Department. ii Mississippi Department of Transportation Construction Manual iii Mississippi Department of Transportation Construction Manual CONTENTS Introduction ................................................................................................................................... ii Contents ....................................................................................................................................... -
6X9 End of World Msalphabetical
THE END OF THE WORLD PROJECT Edited By RICHARD LOPEZ, JOHN BLOOMBERG-RISSMAN AND T.C. MARSHALL “Good friends we have had, oh good friends we’ve lost, along the way.” For Dale Pendell, Marthe Reed, and Sudan the white rhino TABLE OF CONTENTS Editors’ Trialogue xiii Overture: Anselm Hollo 25 Etel Adnan 27 Charles Alexander 29 Will Alexander 42 Will Alexander and Byron Baker 65 Rae Armantrout 73 John Armstrong 78 DJ Kirsten Angel Dust 82 Runa Bandyopadhyay 86 Alan Baker 94 Carlyle Baker 100 Nora Bateson 106 Tom Beckett 107 Melissa Benham 109 Steve Benson 115 Charles Bernstein 117 Anselm Berrigan 118 John Bloomberg-Rissman 119 Daniel Borzutzky 128 Daniel f Bradley 142 Helen Bridwell 151 Brandon Brown 157 David Buuck 161 Wendy Burk 180 Olivier Cadiot 198 Julie Carr / Lisa Olstein 201 Aileen Cassinetto and C. Sophia Ibardaloza 210 Tom Cohen 214 Claire Colebrook 236 Allison Cobb 248 Jon Cone 258 CA Conrad 264 Stephen Cope 267 Eduardo M. Corvera II (E.M.C. II) 269 Brenda Coultas 270 Anne Laure Coxam 271 Michael Cross 276 Thomas Rain Crowe 286 Brent Cunningham 297 Jane Dalrymple-Hollo 300 Philip Davenport 304 Michelle Detorie 312 John DeWitt 322 Diane Di Prima 326 Suzanne Doppelt 334 Paul Dresman 336 Aja Couchois Duncan 346 Camille Dungy 355 Marcella Durand 359 Martin Edmond 370 Sarah Tuss Efrik and Johannes Göransson 379 Tongo Eisen-Martin 397 Clayton Eshleman 404 Carrie Etter 407 Steven Farmer 409 Alec Finlay 421 Donna Fleischer 429 Evelyn Flores 432 Diane Gage 438 Jeannine Hall Gailey 442 Forrest Gander 448 Renée Gauthier 453 Crane Giamo 454 Giant Ibis 459 Alex Gildzen 460 Samantha Giles 461 C. -
Kee, Kevin. Pastplay: Teaching and Learning History with Technology
Kee, Kevin. Pastplay: Teaching and Learning History with Technology. E-book, Ann Arbor, MI: University of Michigan Press, 2014, https://doi.org/10.3998/dh.12544152.0001.001. Downloaded on behalf of Unknown Institution Pastplay Kee, Kevin. Pastplay: Teaching and Learning History with Technology. E-book, Ann Arbor, MI: University of Michigan Press, 2014, https://doi.org/10.3998/dh.12544152.0001.001. Downloaded on behalf of Unknown Institution Digital Humanities The Digital Humanities series provides a forum for ground- breaking and benchmark work in digital humanities, lying at the intersections of computers and the disciplines of arts and humanities, library and information science, media and communications studies, and cultural studies. Series Editors: Julie Thompson Klein, Wayne State University Tara McPherson, University of Southern California Paul Conway, University of Michigan Teaching History in the Digital Age T. Mills Kelly Hacking the Academy: New Approaches to Scholarship and Teaching from Digital Humanities Daniel J. Cohen and Tom Scheinfeldt, Editors Writing History in the Digital Age Jack Dougherty and Kristen Nawrotzki, Editors Pastplay: Teaching and Learning History with Technology Kevin Kee, Editor diGitalculturebooks, an imprint of the University of Michigan Press, is dedicated to publishing work in new media studies and the emerging field of digital humanities. Kee, Kevin. Pastplay: Teaching and Learning History with Technology. E-book, Ann Arbor, MI: University of Michigan Press, 2014, https://doi.org/10.3998/dh.12544152.0001.001. Downloaded on behalf of Unknown Institution Pastplay Teaching and Learning History with Technology Kevin Kee, Editor The University of Michigan Press Ann Arbor Kee, Kevin. Pastplay: Teaching and Learning History with Technology. -

From the Bedroom to LA: Revisiting the Settings of Early Video Blogs on Youtube
EUROPEAN JOURNAL OF MEDIA STUDIES www.necsus-ejms.org From the bedroom to LA: Revisiting the settings of early video blogs on YouTube Rainer Hillrichs NECSUS 5 (2), Autumn 2016: 107–131 URL: https://necsus-ejms.org/from-the-bedroom-to-la-revisiting- the-settings-of-early-video-blogs-on-youtube/ Keywords: audiovisual media, digital culture, genre, home, online video, Web 2.0 The home is only one of many settings in contemporary YouTube videos. On professionalised video blogs, domestic settings are only used when they are motivated by particular video projects. Videos of the popular Let’s Play genre may be recorded in the home, but the true settings of the videos are the worlds of the games in which the user acts through an avatar. Music videos on channels by mainstream pop stars, such as RihannaVEVO, obvi- ously feature diverse settings.[1] However, as crucial works of online video studies point out, the home and the bedroom in particular were common settings of early YouTube videos.[2] This article revisits the settings of early video blogs on YouTube and the arguments made about these settings and their cultural meanings thus far. Video bloggers’ use of domestic and other settings is a far more complex issue than it may initially appear. Conven- ience, creative ambitions, viewers’ expectations, and emerging conventions intersected in this dimension of video blogging. In contrast with the notion of ‘private spaces’ that were ‘simply’ shown ‘as ‘they are’,[3] I suggest that bedrooms were locations which were willingly, consciously, and performatively put into the scene on video blogs. -
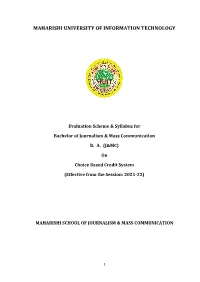
Ba(Jmc) Theory3
MAHARISHI UNIVERSITY OF INFORMATION TECHNOLOGY Evaluation Scheme & Syllabus for Bachelor of Journalism & Mass Communication B. A. (J&MC) On Choice Based Credit System (Effective from the Session: 2021-22) MAHARISHI SCHOOL OF JOURNALISM & MASS COMMUNICATION 1 Evaluation Scheme B. A. (J& MC) First Semester S. Course Course Code Course Title L-T- CIA ESE Total Credits NO. Category P Marks Marks 1 BA(J&MC)101 Basics of Mass 4-0- 30 70 100 4 Communication 0 2 BA(J&MC)102 Understanding 4-0- 30 70 100 4 of media 0 Core Courses language 3 BA(J&MC)103 Print media 4-0- 30 70 100 4 0 4 BA(J&MC)104 Basics of design 4-0- 30 70 100 4 & graphics 0 5 BA(J&MC)105 Print Media Lab 0-0- 30 70 100 1 2 6 Practical/Lab BA(J&MC)106 Basics of 0-0- 30 70 100 1 Design & 2 Graphics Lab TOTAL 180 420 600 18 Qualifying non-credit course 5 Self- BA(J&MC)107 Basics of 2-1- 70 30 100 0 Development Transcendental 1 courses/ Meditation and Science for Yoga Consciousness (SOC) 2 TEACHING-LEARNING PLAN Course Title: BASICS OF MASS COMMUNICATION Course Code: BA (J&MC) 101 L T P C.U. Pre-requisites, if any: Sound knowledge of Journalism and Mass 4 0 0 4 Communication as a subject is desirable. Course Description: The course is designed to discuss all aspects of any Communication along with developing an understanding of their models and theory. This course deals with the fundamentals of communication models and theory. -
Download This PDF File
Library Technology R E P O R T S Expert Guides to Library Systems and Services Podcast Literacy: Educational, Accessible, and Diverse Podcasts for Library Users Nicole Hennig alatechsource.org American Library Association About the Author Library Technology Nicole Hennig is an independent user experience pro- REPORTS fessional, helping librarians and educators effectively use mobile technologies. See her educational offerings ALA TechSource purchases fund advocacy, awareness, and at http://nicolehennig.com. She is the author of sev- accreditation programs for library professionals worldwide. eral books, including Apps for Librarians: Using the Best Volume 53, Number 2 Mobile Technology to Educate, Create, and Engage. Her Podcast Literacy: Educational, Accessible, and Diverse online courses, such as Apps for Librarians & Educators, Podcasts for Library Users have enabled librarians from all types of institutions to ISBN: 978-0-8389-5985-5 effectively implement mobile technologies in their pro- American Library Association grams and services. Her newsletter, Mobile Apps News, 50 East Huron St. helps librarians stay current with mobile technologies. Chicago, IL 60611-2795 USA Hennig worked for the MIT Libraries for fourteen years alatechsource.org as head of user experience and web manager. She is the 800-545-2433, ext. 4299 312-944-6780 winner of several awards, including the MIT Excellence 312-280-5275 (fax) Award for Innovative Solutions. Advertising Representative Samantha Imburgia [email protected] Abstract 312-280-3244 Editors Podcasts are experiencing a renaissance today. More Patrick Hogan high-quality programming is available for more [email protected] diverse audiences than ever before. 312-280-3240 When librarians are knowledgeable about pod- Samantha Imburgia casts, how to find the best ones, and what purposes [email protected] they serve, we can point our users to the very best 312-280-3244 content and help increase digital literacy. -
Best Practices in Project Delivery Management
SCAN TEAM REPORT NCHRP Project 20-68A, Scan 07-01 Best Practices in Project Delivery Management Supported by the National Cooperative Highway Research Program The information contained in this report was prepared as part of NCHRP Project 20-68A U.S. Domestic Scan, National Cooperative Highway Research Program. SPECIAL NOTE: This report IS NOT an offi cial publication of the National Cooperative Highway Research Program, Transportation Research Board, National Research Council, or The National Academies. Acknowledgment The work described in this document was conducted as part of NCHRP Project 20-68A, the U.S. Domestic Scan program. This program was requested by the American Association of State Highway and Transportation Officials (AASHTO), with funding provided through the National Cooperative Highway Research Program (NCHRP). The NCHRP is supported by annual voluntary contributions from the state departments of transportation. Additional support for selected scans is provided by the U.S. Federal Highway Administration and other agencies. The purpose of each scan and of Project 20-68A as a whole is to accelerate beneficial innovation by facilitating information sharing and technology exchange among the states and other transportation agencies, and identifying actionable items of common interest. Experience has shown that personal contact with new ideas and their application is a particularly valuable means for such sharing and exchange. A scan entails peer-to-peer discussions between practitioners who have implemented new practices and others who are able to disseminate knowledge of these new practices and their possible benefits to a broad audience of other users. Each scan addresses a single technical topic selected by AASHTO and the NCHRP 20-68A Project Panel. -
Bachelor of Technology Computer Science & Engineering
Study & Evaluation Scheme Of Bachelor of Technology Computer Science & Engineering With Specialization in Artificial Intelligence (In Collaboration with iNurture) (Based on Choice Based Credit System) [Applicable w.e.f. Academic Session 2019-20] COLLEGE OF COMPUTING SCIENCES AND INFORMATION TECHNOLOGY TEERTHANKER MAHAVEERUNIVERSITY N.H.-24, Delhi Road, Moradabad, UttarPradesh- 244001 Website:www.tmu.ac.in TEERTHANKER MAHAVEERUNIVERSITY (EstablishedunderGovt.ofU.P.ActNo.30,2008) Delhi Road, Bagarpur, Moradabad (U.P) Study & Evaluation Scheme SUMMARY Institute Name College of Computing Sciences and Information Technology (CCSIT), Delhi Road, Moradabad Programme B.Tech. CSE (Artificial Intelligence) Duration Four Years full time(Eight Semesters) Medium English Minimum Required 75% Attendance Credits Maximum Credits 180 Minimum Credits 172 Required for Degree Assessment: Evaluation Internal External Total Theory 40 60 100 Practical/ Dissertations/ Project Reports/ Viva- Voce 50 50 100 Class Test-1 Class Test-2 Class Test-3 Assignment(s) Attendance & Total Best two out of three Participation 10 10 10 10 10 40 External Internal Duration of Examination 3 Hours 1.5 Hours To qualify the course a student is required to secure a minimum of 45% marks in aggregate including the semester end examination and teachers continuous evaluation.(i.e. both internal and external).A candidate who secures less than 45% of marks in a course shall be deemed to have failed in that course. The student should have at least 45% marks in aggregate to clear the semester. # Provision for delivery of 25% content through online mode. # Policy regarding promoting the students from semester to semester & year to year. No specific condition to earn the credit for promoting the students from one semester to next semester. -

Earthwork Manual • Erosion Control Manual This Book Should Be Kept by the Pipe Installation Inspector As a Reference Guide During the Performance of His Duties
FY2016 Earthwork CHAPTER 1 INTRODUCTION - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 3 THE ROLE OF AN INSPECTOR - - - - - - - - - - - - - - - - - - - - - - - - - - - 3 COMMUNICATIONS AND ATTITUDE - - - - - - - - - - - - - - - - - - - - - - - 3 QUALIFICATIONS OF THE INSPECTOR - - - - - - - - - - - - - - - - - - - - - - 4 SAMPLING AND TESTING - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 5 RECORDS - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 5 INSPECTOR EQUIPMENT AND MATERIALS - - - - - - - - - - - - - - - - - - - - 5 SUMMARY - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 6 CHAPTER 2 PREPARATION FOR CONSTRUCTION - - - - - - - - - - - - - - - - - - - - - - - 7 PLAN REVIEW - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 7 PROPOSAL REVIEW - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - 8 PRELIMINARY PROJECT INSPECTION - - - - - - - - - - - - - - - - - - - - - - - 8 MATERIALS AND CERTIFICATION REVIEW - - - - - - - - - - - - - - - - - - - 8 PRE-CONSTRUCTION MEETING - - - - - - - - - - - - - - - - - - - - - - - - - -10 CHAPTER 3 CONSTRUCTION DOCUMENTATION- - - - - - - - - - - - - - - - - - - - - - - 12 FIELD DIARY - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -12 EXTRA WORK AUTHORIZATION - - - - - - - - - - - - - - - - - - - - - - - - -14 FORCE ACCOUNT - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -15 FORCE ACCOUNT SUMMARY - - - - - - - - - - - - - - - - - - - - - - - -