Hypocretin Receptor Antagonists for Insomnia: Rationale and Clinical Data
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neuroendocrine and Sympathetic Responses to an Orexin Receptor Antagonist, SB-649868, and Alprazolam Following Insulin-Induced Hypoglycemia in Humans
Psychopharmacology (2014) 231:3817–3828 DOI 10.1007/s00213-014-3520-7 ORIGINAL INVESTIGATION Neuroendocrine and sympathetic responses to an orexin receptor antagonist, SB-649868, and Alprazolam following insulin-induced hypoglycemia in humans Ameera X. Patel & Sam R. Miller & Pradeep J. Nathan & Ponmani Kanakaraj & Antonella Napolitano & Philip Lawrence & Annelize Koch & Edward T. Bullmore Received: 8 October 2013 /Accepted: 24 February 2014 /Published online: 26 April 2014 # The Author(s) 2014. This article is published with open access at Springerlink.com Abstract it has previously been validated using the insulin tolerance test Rationale The orexin-hypocretin system is important for (ITT) model in humans. translating peripheral metabolic signals and central neuronal Results Of the primary endpoints, ITT induced defined in- inputs to a diverse range of behaviors, from feeding, motiva- creases in pulse rate, plasma cortisol, and adrenocorticotropic tion and arousal, to sleep and wakefulness. Orexin signaling is hormone in the placebo condition, but these responses were thus an exciting potential therapeutic target for disorders of not significantly impacted by alprazolam or SB-649868 pre- sleep, feeding, addiction, and stress. treatment. Of the secondary endpoints, ITT induced a defined Objectives/methods Here, we investigated the low dose phar- increase in plasma concentrations of adrenaline, noradrena- macology of orexin receptor antagonist, SB-649868, on neu- line, growth hormone (GH), and prolactin in the placebo roendocrine, sympathetic nervous system, and behavioral re- condition. Alprazolam pre-treatment significantly reduced sponses to insulin-induced hypoglycemic stress, in 24 healthy the GH response to ITT (p<0.003), the peak electromyogra- male subjects (aged 18–45 years; BMI 19.0–25.9 kg/m2), phy (p<0.0001) and galvanic skin response (GSR, p=0.04)to using a randomized, double-blind, placebo-controlled, acoustic startle, the resting GSR (p=0.01), and increased within-subject crossover design. -

Orexin Receptor Antagonists As Therapeutic Agents for Insomnia
REVIEW ARTICLE published: 25 December 2013 doi: 10.3389/fphar.2013.00163 Orexin receptor antagonists as therapeutic agents for insomnia Ana C. Equihua 1, Alberto K. De La Herrán-Arita 2 and Rene Drucker-Colin 1* 1 Neuropatología Molecular, Instituto de Fisiología Celular, Universidad Nacional Autónoma de México, Mexico City, México 2 Center for Sleep Sciences and Medicine, Stanford University, Palo Alto, CA, USA Edited by: Insomnia is a common clinical condition characterized by difficulty initiating or maintaining Christopher J. Winrow, Merck, USA sleep, or non-restorative sleep with impairment of daytime functioning. Currently, Reviewed by: treatment for insomnia involves a combination of cognitive behavioral therapy (CBTi) Matthew R. Ebben, Weill Medical and pharmacological therapy. Among pharmacological interventions, the most evidence College of Cornell University, USA Gabriella Gobbi, McGill University, exists for benzodiazepine (BZD) receptor agonist drugs (GABAA receptor), although Canada concerns persist regarding their safety and their limited efficacy. The use of these Matt Carter, University of hypnotic medications must be carefully monitored for adverse effects. Orexin (hypocretin) Washington, USA neuropeptides have been shown to regulate transitions between wakefulness and Michihiro Mieda, Kanazawa University, Japan sleep by promoting cholinergic/monoaminergic neural pathways. This has led to the *Correspondence: development of a new class of pharmacological agents that antagonize the physiological Rene Drucker-Colin, Departamento effects of orexin. The development of these agents may lead to novel therapies for de Neurociencias, Instituto de insomnia without the side effect profile of hypnotics (e.g., impaired cognition, disturbed Fisiología Celular, Universidad arousal, and motor balance difficulties). However, antagonizing a system that regulates Nacional Autónoma de México, Circuito exterior S/N, Apdo. -

204569Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 204569Orig1s000 MEDICAL REVIEW(S) Cross Discipline Team Leader Review 3. CMC/Device Dr. Khairuzzaman found the drug product portion of the NDA to be acceptable, and without need for phase 4 commitments. Dr. Sapru’s review stated that with the exception of a pending issue concerning the control of potential genotoxic impurity (b) (4) the NDA was approvable in terms of drug substance. Dr. Suarez found that the NDA was acceptable from a biopharmaceutics perspective. The Office of Compliance issuance of an acceptable recommendation for drug substance manufacturing and testing facilities was pending at the time of this review. 4. Nonclinical Pharmacology/Toxicology Dr. Richard Siarey completed the primary nonclinical review, and Dr. Lois Freed completed a supervisory memo. Dr. Siarey’s overall conclusion was that from a nonclinical perspective, approval of the suvorexant NDA was recommended. However, he found evidence that catapelxy was observed in dogs exposed to MK-4305 (suvorexant) near Tmax, although he concluded that additional information could have been gained by studying the drug in an experimental model that has been used for diagnosing cataplexy in dogs. Dr. Siarey suggested that since cataplexy occurred in dogs near Tmax, a time at which if used for insomnia patients would ordinarily be in bed, safety concern for humans was reduced. Dr. Siarey also found that the neurobehavioral assessment in the pre- and post-natal developmental study was not complete, as the passive avoidance tests was performed too early in development, while learning/acquisition tests and retention/memory tests were not conducted. -

Anti-Infectives Industry Over the Next 5 Years and Beyond
Bridging the innovation gap... New Drug Futures: Products that could change the pharma market to 2013 and beyond Over 70 pipeline prospects This new major and insightful 450 page in 8 major therapy areas analysis evaluates, compares and contrasts the are analysed in this report prospects for the development compounds that could revolutionise the pharmaceutical Anti-infectives industry over the next 5 years and beyond. Cardiovascular CNS The report provides: Gastrointestinal Detailed background and market context for Metabolic each therapy area covered: Musculoskeletal Addressable patient population Oncology Current treatments Sales drivers Respiratory Sales breakers Future treatments Market dynamics – winners and losers Key drug launches by 2013 Unique sales forecasts by major product to 2013 Over 70 key products assessed Unique evaluation scores for key areas such as novelty of mechanism, clinical data and competition Critical and detailed appraisal of each product‟s research and development Extensive pipeline listings, putting the profiled products into their competitive context The search – and need – for new products has never been greater and what’s in the development pipeline has never generated more interest. That is why this analysis is so important! GLOBAL PHARMA MARKET IN CONTEXT THE Are there too many prophets of doom ready to write-off the research-based pharma industry in the future? Too few novel There is plenty on which to base such anxiety. The research-based industry products and an must achieve a fair price in the face of greater cost control, while the aggressive generic burden of regulation is setting the bar high for successful product sector are taking introduction. -

The Dual Orexin Receptor Antagonist TCS1102 Does Not Affect Reinstatement of Nicotine- Seeking
RESEARCH ARTICLE The dual orexin receptor antagonist TCS1102 does not affect reinstatement of nicotine- seeking Shaun Yon-Seng Khoo, Gavan P. McNally, Kelly J. Clemens* School of Psychology, University of New South Wales, Sydney, Australia * [email protected] a1111111111 a1111111111 a1111111111 Abstract a1111111111 a1111111111 The orexin/hypocretin system is important for appetitive motivation towards multiple drugs of abuse, including nicotine. Both OX1 and OX2 receptors individually have been shown to influence nicotine self-administration and reinstatement. Due to the increasing clinical use of dual orexin receptor antagonists in the treatment of disorders such as insomnia, we OPEN ACCESS examined whether a dual orexin receptor antagonist may also be effective in reducing nico- Citation: Khoo SY-S, McNally GP, Clemens KJ tine seeking. We tested the effect of intracerebroventricular (i.c.v.) administration of the (2017) The dual orexin receptor antagonist potent and selective dual orexin receptor antagonist TCS1102 on orexin-A-induced food TCS1102 does not affect reinstatement of nicotine- self-administration, nicotine self-administration and reinstatement of nicotine-seeking in seeking. PLoS ONE 12(3): e0173967. https://doi. org/10.1371/journal.pone.0173967 rats. Our results show that 30 μg of TCS1102 i.c.v. abolishes orexin-A-induced increases in food self-administration but does not reduce nicotine self-administration. Neither i.c.v. 10 μg Editor: Judith Homberg, Radboud University Medical Centre, NETHERLANDS nor 30 μg of TCS1102 reduced compound reinstatement after short-term (15 days) self- administration nicotine, but 30 μg transiently reduced cue/nicotine compound reinstatement Received: November 24, 2016 after chronic self-administration (29 days). -

Annual HFHS Publications List 2017 This Bibliography Aims to Recognize
Annual HFHS Publications List 2017 This bibliography aims to recognize the scholarly activity and provide ease of access to journal articles, meeting abstracts, book chapters, books and other works published by Henry Ford Health System personnel. Searches were conducted in PubMed, Embase, Web of Science, and Google Scholar during 2017, and then imported into EndNote for formatting. The searches captured over 1,500 unique publications from Henry Ford Health System authors for 2017. Click the “Full Text” link to view the articles to which Sladen Library provides access. If the full-text of the article is not available, you may request it through ILLiad by clicking on the “Article Request Form,” or by calling us at 313-916-2550. If you would like to be added to the monthly email distribution list to automatically receive a PDF of this bibliography in your inbox, or you have any questions or comments, please contact Angela Cabrera at [email protected]. Administration Omar J, Heidemann DL, Blum-Alexandar B, Uju-Eke C, Alam Z, Willens DE, and Wisdom K. Fresh prescription: Improving nutrition education and access to fresh produce in Detroit J Gen Intern Med 2017; 32(2):S752. PMID: Not assigned. Abstract Administration Smith KL, Fedel P, and Heitman J. Incapacitated surrogates: A new and increasing dilemma in hospital care J Clin Ethics 2017; 28(4):279-289. PMID: 29257763. Article Request Form Allergy Brown KR, Krouse RZ, Calatroni A, Visness CM, Sivaprasad U, Kercsmar CM, Matsui EC, West JB, Makhija MM, Gill MA, Kim H, Kattan M, Pillai D, Gern JE, Busse WW, Togias A, Liu AH, and Khurana Hershey GK. -

OREXIN ANTAGONISTS BELSOMRA (Suvorexant), DAYVIGO (Lemborexant)
OREXIN ANTAGONISTS BELSOMRA (suvorexant), DAYVIGO (lemborexant) RATIONALE FOR INCLUSION IN PA PROGRAM Background Belsomra (suvorexant) and Dayvigo (lemborexant) are orexin receptor antagonists used to treat difficulty in falling and staying asleep (insomnia). Orexins are chemicals that are involved in regulating the sleep-wake cycle and play a role in keeping people awake (1-2). Regulatory Status FDA-approved indication: Orexin receptor antagonists are indicated for the treatment of insomnia, characterized by difficulties with sleep onset and/or sleep maintenance (1-2). Orexin Antagonists are contraindicated in patients with narcolepsy (1-2). Orexin Antagonists are central nervous system (CNS) depressants that can impair daytime wakefulness even when used as prescribed. Medications that treat insomnia can cause next-day drowsiness and impair driving and other activities that require alertness. Orexin Antagonists can impair driving skills and may increase the risk of falling asleep while driving. People can be impaired even when they feel fully awake. Patients should also be made aware of the potential for next-day driving impairment, because there is individual variation in sensitivity to the drug (1-2). The failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or mental illness that should be evaluated (1-2). Warnings and precautions that should be discussed with the patient on Orexin Antagonist therapy include adverse reactions on abnormal thinking and behavioral changes (such as amnesia, anxiety, hallucinations and other neuropsychiatric symptoms), complex behaviors (such as sleep- driving, preparing and eating food, or making phone calls), dose-dependent increase in suicidal ideation, and sleep paralysis which is the inability to move or speak for up to several minutes during sleep-wake transitions (1-2). -
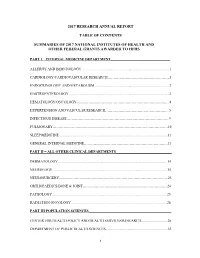
2017 Research Annual Report Table of Contents Summaries of 2017
2017 RESEARCH ANNUAL REPORT TABLE OF CONTENTS SUMMARIES OF 2017 NATIONAL INSTITUTES OF HEALTH AND OTHER FEDERAL GRANTS AWARDED TO HFHS PART I – INTERNAL MEDICINE DEPARTMENT_________________________________ ALLERGY AND IMMUNOLOGY ................................................................................................. 1 CARDIOLOGY/CARDIOVASCULAR RESEARCH…………………………………………….1 ENDOCRINOLOGY AND METABOLISM .................................................................................. 2 GASTROENTEROLOGY ............................................................................................................. .3 HEMATOLOGY/ONCOLOGY…………………………………………………………………...4 HYPERTENSION AND VASCULAR RESEARCH……………………………………………...5 INFECTIOUS DISEASE…………………………………………………………………………..9 PULMONARY……………………………………………………………………………………10 SLEEP MEDICINE ....................................................................................................................... 11 GENERAL INTERNAL MEDICINE…………………………………………………………….13 PART II – ALL OTHER CLINICAL DEPARTMENTS_______________________________ DERMATOLOGY ........................................................................................................................ 14 NEUROLOGY .............................................................................................................................. 15 NEUROSURGERY……………………………………………………………………………….23 ORTHOPAEDICS/BONE & JOINT……………………………………………………………..24 PATHOLOGY .............................................................................................................................. -

Merck & Co., Inc
As filed with the Securities and Exchange Commission on February 25, 2021 UNITED STATES SECURITIES AND EXCHANGE COMMISSION WASHINGTON, D. C. 20549 _________________________________ FORM 10-K (MARK ONE) ☒ Annual Report Pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 For the Fiscal Year Ended December 31, 2020 OR ☐ Transition Report Pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 For the transition period from to Commission File No. 1-6571 _________________________________ Merck & Co., Inc. 2000 Galloping Hill Road Kenilworth New Jersey 07033 (908) 740-4000 New Jersey 22-1918501 (State or other jurisdiction of incorporation) (I.R.S Employer Identification No.) Securities Registered pursuant to Section 12(b) of the Act: Title of Each Class Trading Symbol(s) Name of Each Exchange on which Registered Common Stock ($0.50 par value) MRK New York Stock Exchange 1.125% Notes due 2021 MRK/21 New York Stock Exchange 0.500% Notes due 2024 MRK 24 New York Stock Exchange 1.875% Notes due 2026 MRK/26 New York Stock Exchange 2.500% Notes due 2034 MRK/34 New York Stock Exchange 1.375% Notes due 2036 MRK 36A New York Stock Exchange Number of shares of Common Stock ($0.50 par value) outstanding as of January 31, 2021: 2,530,315,668. Aggregate market value of Common Stock ($0.50 par value) held by non-affiliates on June 30, 2020 based on closing price on June 30, 2020: $195,461,000,000. Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. -

Role of the Orexin Receptor System in Stress, Sleep and Cocaine Use
Role of the orexin receptor system in stress, sleep and cocaine use NCT02785406 Version Date: 04/25/2017 IRB NUMBER: HSC-MS-16-0120 IRB APPROVAL DATE: 04/25/2017 Title: Role of the orexin receptor system in stress, sleep and cocaine use Principal Investigator: Scott D. Lane Co-Investigators: Joy M. Schmitz, Charles E. Green, Jin H. Yoon, Michael F. Weaver ABSTRACT Preclinical research has established important functions for the orexin system in mediating arousal/sleep, stress, and cue-induced reinstatement of drug taking (e.g., relapse). The role of stress/anxiety and drug cue reactivity in human drug relapse is well established, but to date, the role of the orexin system in modulating these phenomena has not been examined in humans with substance use disorders (e.g., cocaine). The goal of the present first-in-human study will be to examine the effects of an orexin antagonist (suvorexant) on interactions among stress/anxiety, sleep, and drug-cue reactivity. We will utilize a battery of highly sensitive, drug-specific, laboratory measures of drug cue reactivity (a relapse risk model), and well-established metrics of stress/anxiety and sleep. We hypothesize that antagonism of the orexin system will attenuate the link between (1) stress/anxiety and drug cue reactivity, and (2) sleep and drug cue reactivity. These results will elucidate a unique biochemical mechanism for understanding relapse, and provide a potential medication target for relapse prevention SCIENTIFIC IMPACT Given the promising preclinical data on the orexin system in modulating sleep, anxiety, and drug cue reactivity, this research project has high translational scientific value. -

Study Protocol
Confidential Page 1 Protocol No. Everolimus Investigator-initiated Protocol Template RAD001 (Everolimus) Clinical evaluation of everolimus (a rapamycin analog) in restoring salivary gland function to patients treated with radiotherapy for head and neck cancer CRAD001XUS274T Authors: Panayiotis Savvides, MD PhD MPH (Principal Investigator) Kirsten Limesand, PhD (co-Investigator) Denise Roe, DrPH (co-Investigator) Sun Yi, MD (co-Investigator) Julie Bauman, MD (co-Investigator) Daruka Mahadevan, MD PhD (co-Investigator) Version number: 1.2 Release date 06/22/2018 Referenced Investigator Brochure 15, release date 27-April-2016 Edition IRB NUMBER: PHXB-17-0072-70-15 IRB APPROVAL DATE: 07/03/2018 Confidential Page 2 Protocol No. Table of contents Table of contents..................................................................................................................2 List of figures.......................................................................................................................3 List of tables.........................................................................................................................3 List of abbreviations ............................................................................................................4 Glossary of terms.................................................................................................................6 Schema.................................................................................................................................8 1 -

G Protein-Coupled Receptors
S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2015/16: G protein-coupled receptors. British Journal of Pharmacology (2015) 172, 5744–5869 THE CONCISE GUIDE TO PHARMACOLOGY 2015/16: G protein-coupled receptors Stephen PH Alexander1, Anthony P Davenport2, Eamonn Kelly3, Neil Marrion3, John A Peters4, Helen E Benson5, Elena Faccenda5, Adam J Pawson5, Joanna L Sharman5, Christopher Southan5, Jamie A Davies5 and CGTP Collaborators 1School of Biomedical Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK, 2Clinical Pharmacology Unit, University of Cambridge, Cambridge, CB2 0QQ, UK, 3School of Physiology and Pharmacology, University of Bristol, Bristol, BS8 1TD, UK, 4Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK, 5Centre for Integrative Physiology, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2015/16 provides concise overviews of the key properties of over 1750 human drug targets with their pharmacology, plus links to an open access knowledgebase of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. The full contents can be found at http://onlinelibrary.wiley.com/doi/ 10.1111/bph.13348/full. G protein-coupled receptors are one of the eight major pharmacological targets into which the Guide is divided, with the others being: ligand-gated ion channels, voltage-gated ion channels, other ion channels, nuclear hormone receptors, catalytic receptors, enzymes and transporters. These are presented with nomenclature guidance and summary information on the best available pharmacological tools, alongside key references and suggestions for further reading.