Food Choices for Gestational Diabetes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brochure-World of Flavors.Pdf
SZECHWAN SHRIMP OVER COCONUT RICE Ingredients 4 Servings 12 Servings SAVORING Weights Measures Weights Measures Calrose or New Variety, uncooked medium grain rice 6 oz 1 cup 1 lb 2 oz 3 cups Water 3/4 cup 2 1/4 cups Coconut milk 3/4 cup 2 1/4 cups CALIFORNIA Butter 1 tbsp 3 tbsp TO MAKE SURE YOU RE Salt 1/2 tsp 1 1/2 tsp ’ Honey 1/3 cup 1 cup USING THE FINEST CALIFORNIA RICE… Soy sauce 3 tbsp 1/2 cup Chili garlic paste 3 tbsp 1/2 cup Shrimp, large and peeled 1 lb 3 lbs RICE LOOK FOR OUR CALIFORNIA PREMIUM RICE SEAL OR CHOOSE ONE OF THESE BRANDS THROUGH YOUR AREA SUPPLIER Vegetable oil 1 tbsp 3 tbsp Bell peppers, any color, matchstick strips 3 oz 1 cup 9 oz 3 cups Carrots, matchstick strips 3 1/2 oz 1 cup 10 1/2 oz 3 cups Snow peas, strips 2 3/4 oz 1 cup 8 3/4 oz 3 cups SWEET &SAVORY PILAF Sliced green onions 1/4 cup 3/4 cup DIRECTIONS: Ingredients 4 Servings 12 Servings TM Weights Measures Weights Measures 1. To prepare rice, combine rice, water, coconut milk, butter and salt in a large pot. Bring to a boil; reduce heat and simmer, covered, Butter 1 oz 2 tbsp 3 oz 6 tbsp for 20 minutes. Remove from heat and let stand for 10 minutes. Calrose uncooked medium grain rice 7 oz 1 cup 1 lb 5 oz 3 cups 2. To prepare shrimp, whisk together honey, soy sauce and chili TM Shallots, sliced 2 oz 2 medium 6 oz 6 medium garlic paste in a large bowl. -

Identification and Utilization of Elite Genes from Elite Germplasms for Yield Improvement
Chapter 5 Identification and Utilization of Elite Genes from Elite Germplasms for Yield Improvement Dawei Xue, Qian Qian and Sheng Teng Additional information is available at the end of the chapter http://dx.doi.org/10.5772/56390 1. Introduction Rice is a major food crop in the world. Half of the world's population relies on rice as their staple food. Due to continuous growth of human population, the area of arable land decreases every year. Therefore, ensuring adequate grain production has become a challenge for many countries. Rice production has an important role in global food security, poverty alleviation and rural employment. The current rate of increase in mean rice yield per annum is only 0.8%, which falls behind the rate of population growth annually. An annual mean increase in rice production of 1.2% is required between 2001 and 2030 in order to catch up with the growing food demand resulting from increase in population[1,2]. Constrained by lack of water resources and arable land, the area for rice cultivation has decreased in the context of economic development and urbanization. It is evident that rice yield cannot be increased by simply expanding the cultivation area. In light of this, it is important to pay attention to increasing rice yield per unit area. There are two major ap‐ proaches for achieving this goal: improving cultivation conditions and technology, and breeding rice varieties with higher yield potential. In order to improve the cultivation techni‐ que, selecting superior cultivars is essential. Practices in rice science and production have shown that high-yield breeding of rice is essential for yield increase, and a breakthrough is usually made through discovery and effective utilization of specific germplasm (gene). -

Serving Glycemic Load White Rice, Boiled, Low-Amylose
Glycemic Index and Glycemic Load Glycemic index measures the rise in blood glucose produced by eating a specific food. Glycemic load builds on the glycemic index concept to provide a more accurate measure of total glycemic response to a food or meal. Glycemic load is equal to the glycemic index multiplied by the grams of carbohydrate per serving. This allows you to sum the GL of all the foods in a meal, for the whole day or even longer. Why is this important? Foods with a high glycemic load elevate triglycerides and small-dense LDLs, reduce HDL cholesterol and increase C-reactive Proteins. In other words, the higher the glycemic Index and Glycemic load, the worse it is for your body and your heart. A good rule of thumb is to try and avoid foods with an index higher than 60. But this is a rule of thumb only, because as you can see from this chart, foods with a lower index can pack a higher load, because of the quantity of carbohydrate in each serving. Glycemic Index and Glycemic Loads of Typical American Foods Food Index Serving Carbs/ Glycemic Size Serving Load White rice, boiled, low-amylose 139 150 42 58.4 Tofu-based frozen dessert, chocolate with high- 115 - - - fructose Glucose 114 10 9.9 11.3 Fruity-Bix™ breakfast cereal, berry 113 - - - White rice, type not specified, boiled 112 150 42 47 Glucose dextrose 111 10 9.9 11 Potato, Russet Burbank, baked without fat 111 150 21.8 24.1 Sucrose 110 10 10 11 Maize meal porridge/gruel 109 - - - Jasmine rice, white long grain, cooked in rice 109 150 42 45.8 cooker Millet flour porridge 107 -
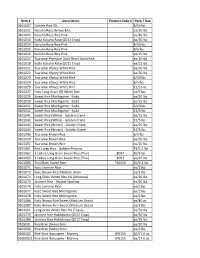
Item # Description Product Code # Pack / Size 0101007 Calrose Rice
Item # Description Product Code # Pack / Size 0101007 Calrose Rice 4% 4/10 lbs 0101011 Kokuho Rose Brown Rice ea/20 lbs 0101012 Kokuho Rose Rice Pink ea/40 lbs 0101013 Koda Kokuho Rose (2011 Crop) ea/20 lbs 0101014 Kokuho Rose Rice Pink 4/10 lbs 0101015 Kokuho Rose Rice Pink 8/5 lbs 0101016 Kokuho Rose Rice Pink ea/15 lbs 0101017 Tsurumai Premium Gold Short Grain Rice ea/20 lbs 0101018 Koda Kokuho Rose (2012 Crop) ea/15 lbs 0101021 Tsurumai Xfancy White Rice ea/50 lbs 0101022 Tsurumai Xfancy White Rice ea/20 lbs 0101023 Tsurumai Xfancy White Rice 4/10 lbs 0101024 Tsurumai Xfancy White Rice 8/5 lbs 0101025 Tsurumai Xfancy White Rice 12/16 oz 0101027 Koto Long Grain 4% White Rice ea/5 lbs 0101029 Sweet Rice Mochigome - Koda ea/50 lbs 0101030 Sweet Rice Mochigome - Koda ea/25 lbs 0101031 Sweet Rice Mochigome - Koda 6/10 lbs 0101032 Sweet Rice Mochigome - Koda 12/5 lbs 0101041 Sweet Rice (White) - Golden Crane ea/25 lbs 0101042 Sweet Rice (White) - Golden Crane 12/5 lbs 0101043 Sweet Rice (Brown) - Golden Crane ea/25 lbs 0101044 Sweet Rice (Brown) - Golden Crane 12/5 lbs 0101046 Tsurumai Brown Rice 6/5 lbs 0101050 Tsurumai Brown Rice ea/50 lbs 0101051 Tsurumai Brown Rice ea/20 lbs 0101061 Red Cargo Rice - Golden Phoenix 15/2.2 lbs 0101062 3 Ladies Long Grain Sweet Rice (Thai) 8094 10/5 lbs 0101063 3 Ladies Long Grain Sweet Rice (Thai) 8092 ea/25 lbs 0101066 Thai Black Sweet Rice TL0234 10/2.2 lbs 0101071 Koto Jasmine Rice ea/2 lbs 0101072 Koto Brown Rice Medium Grain ea/2 lbs 0101074 Long Grain White Rice 4% (Arkansas) ea/50 lbs 0101075 Jasmine -
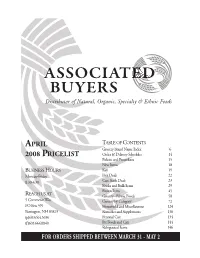
08 APRIL Cat Smaller.Indd
ASSOCIATEDEEDD BUYERS Distributor of Natural, Organic, Specialty & Ethnic Foods APRIL TABLE OF CONTENTS Grocery Brand Name Index 6 2008 PRICELIST Order & Delivery Schedules 14 Policies and Procedures 15 New Items 18 BUSINESS HOURS Key 19 Monday-Friday Hot Deals 22 8:30-4:30 Case Stack Deals 23 Books and Bulk Items 29 Frozen Items 45 REACH US AT Grocery - Ethnic Foods 58 5 Commerce Way Grocery by Category 72 PO Box 399 Household and Miscellaneous 124 Barrington, NH 03825 Remedies and Supplements 130 (p)603.664.5656 Personal Care 134 (f)603.664.8840 Pet Foods and Care 144 Refrigerated Items 146 FOR ORDERS SHIPPED BETWEEN MARCH 31 - MAY 2 TABLE OF CONTENTS PASTA 105 ANNIE’S HOMEGROWN PASTA SAUCES 107 cookies BRAND NAME INDEX 6 PIZZA SAUCES & CRUSTS 107 crackers, bread sticks & rice cakes ORDER & DELIVERY SCHEDULE 14 PREPARED FOODS, CANNED 108 prepared foods, canned POLICIES & PROCEDURES 15 PREPARED FOODS, PACKAGED 108 prepared foods, packaged NEW ITEMS 18 PRESERVES, SWEETENED 109 ANNIE’S NATURALS BOOKS & BULK ITEMS 29 PRESERVES, UNSWEETENED 110 condiments, cooking BBQ sauces FROZEN FOODS 45 PRESERVES & SPREADS, BUTTERS 111 condiments, cooking marinades RICE 111 condiments, cooking worcestershire GROCERY - ETHNIC FOODS 58 condiments, salad dressings GROCERY BY CATEGORY 72 SEA VEGETABLES 112 SEAFOOD 112 condiments, sandwich spd, mustard HOUSEHOLD & MISC. 124 SNACK & SNACK BARS 112 condiments, sandwich sprd, ketchup REMEDIES & SUPPLEMENTS 130 SOUPS, CANNED & ASCEPTIC 115 APPALACHIAN NATURALS PERSONAL CARE 134 SOUPS, CUPS & DRY MIXES 115 condiments, -
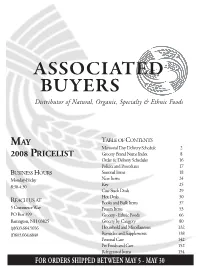
08 MAY CAT Copy.Indd
ASSOCIATED BUYERS Distributor of Natural, Organic, Specialty & Ethnic Foods MAY TABLE OF CONTENTS Memorial Day Delivery Schedule 2 2008 PRICELIST Grocery Brand Name Index 8 Order & Delivery Schedules 16 Policies and Procedures 17 BUSINESS HOURS Seasonal Items 18 Monday-Friday New Items 24 8:30-4:30 Key 25 Case Stack Deals 29 Hot Deals 30 REACH US AT Books and Bulk Items 37 5 Commerce Way Frozen Items 53 PO Box 399 Grocery - Ethnic Foods 66 Barrington, NH 03825 Grocery by Category 80 (p)603.664.5656 Household and Miscellaneous 132 (f)603.664.8840 Remedies and Supplements 138 Personal Care 142 Pet Foods and Care 152 Refrigerated Items 154 FOR ORDERS SHIPPED BETWEEN MAY 5 - MAY 30 Memorial Day 2008 Delivery Schedule Area route #‛s 100, 101 & 150 Area route #‛s 503 Order Thurs., May 22 by 4 pm Order Wed., May 28 by 1 pm Deliver Tues. & Wed., May 27 & 28 Deliver Fri., May 30 Area route #‛s 200 & 201 Area route #‛s 516 Order Friday, May 23 by 4 pm Order Tues., May 27 by 4 pm Deliver Wed., Thurs., May 28 & 29 Deliver Thurs. & Fri., May 29 & 30 Area route #‛s 300 & 301 Area route #‛s 600, 602 & 603 Order Friday, May 23 by 11 am Order Tues., May 27 by 4 pm Deliver Tues., Wed., May 27 & 28 Deliver Thurs., Fri. & Sat., May 29, 30 & June 1 Area route #‛s 400 & 402 Order Wed., May 28 by 4 pm Area route #‛s 900 Deliver Friday, May 30 Order Tues., May 27 by 11 am Deliver Wed., May 28 Area route #‛s 401 Order Tues., May 27 by 4 pm Area route #‛s 950 & 951 Deliver Thurs., May 29 Order Friday, May 23 by 2 pm Deliver Tues., May 27 Area route #‛s 450 & 451 -

Evaluation of 2-Acetyl-1-Pyrroline in Foods, with an Emphasis on Rice Flavour
Evaluation of 2-acetyl-1-pyrroline in foods, with an emphasis on rice flavour Article Accepted Version Creative Commons: Attribution-Noncommercial-No Derivative Works 4.0 Wei, X., Handoko, D. D., Pather, L., Methven, L. and Elmore, J. S. (2017) Evaluation of 2-acetyl-1-pyrroline in foods, with an emphasis on rice flavour. Food Chemistry, 232. pp. 531-544. ISSN 0308-8146 doi: https://doi.org/10.1016/j.foodchem.2017.04.005 Available at http://centaur.reading.ac.uk/69971/ It is advisable to refer to the publisher’s version if you intend to cite from the work. See Guidance on citing . To link to this article DOI: http://dx.doi.org/10.1016/j.foodchem.2017.04.005 Publisher: Elsevier All outputs in CentAUR are protected by Intellectual Property Rights law, including copyright law. Copyright and IPR is retained by the creators or other copyright holders. Terms and conditions for use of this material are defined in the End User Agreement . www.reading.ac.uk/centaur CentAUR Central Archive at the University of Reading Reading’s research outputs online 1 Evaluation of 2-acetyl-1-pyrroline in foods, with an emphasis on rice 2 flavour 3 Xuan Weia, Dody D. Handokob, Leela Pathera, Lisa Methvena, J. Stephen Elmorea* 4 a Department of Food and Nutritional Sciences, University of Reading, Whiteknights, 5 Reading RG6 6AP, UK 6 b Indonesian Centre for Rice Research, Cikampek, Subang 41256, West Java, Indonesia 7 8 * Corresponding author. Tel.: +44 118 3787455; fax: +44 118 3787708. 9 E-mail address: [email protected] (J.S. -
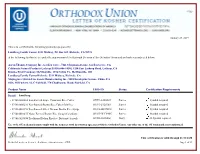
View Certificate
January 23, 2019 This is to certify that the following product(s) prepared by Lundberg Family Farms, 5311 Midway, PO Box 369, Richvale, CA 95974 at the following facilitie(s) are under the supervision of the Kashruth Division of the Orthodox Union and are kosher as indicated below. Aaron Thomas Company Inc.-Garden Grove, 7421 Chapman Avenue, Garden Grove, CA California Natural Products-Lathrop [USDA #06-1430], 1250 East Lathrop Road, Lathrop, CA Dundee Fruit Company-McMinnville, 1974 Colvin Ct., McMinnville, OR Lundberg Family Farms-Richvale, 5311 Midway, Richvale, CA Maplegrove Gluten Free Foods Manufacturing Inc., 5010 Eucalyptus Avenue, Chino, CA Olive Oil Factory, LLC-Fairfield, 770 Chadbourne Road, Fairfield, CA Product Name UKD-ID Status Certification Requirements Brand: Lundberg • 073416000063 Eco-Farmed Apple Cinnamon Rice Cakes OUV3-1400A89 Pareve Symbol required. • 073416000216 Eco-Farmed Brown Rice Cakes Salt-Free OUV3-F326360 Pareve Symbol required. • 073416001558 Eco-Farmed Sweet Dreams Brown Rice Syrup OUV3-BF278C8 Pareve Symbol required. • 073416001855 Nutra-Farmed Brown Rice Syrup (Canadian) OUV3-9FCE4EC Pareve Symbol required. • 073416020054 Traditional Italian Risotto - Butternut Squash OUD3-38C0866 Dairy -D Symbol required. Use of the OU trademark must comply with the terms set forth in a written agreement with the Orthodox Union. Any other use of the OU trademark is not authorized. This certification is valid through 01/31/2020 Rabbi Menachem Genack, Rabbinic Administrator, CEO Page 1 of 19 January 23, 2019 Lundberg Family Farms (continued) This is to certify that the following product(s) prepared by this company at the facilitie(s) listed above are under the supervision of the Kashruth Division of the Orthodox Union and are kosher as indicated below. -
Temperate Rice in Korea. In
2012 TTP-Citation.inddP-Citation.indd i 55/28/2012/28/2012 33:17:13:17:13 PPMM The International Rice Research Institute (IRRI) was established in 1960 by the Ford and Rockefeller Foundations with the help and approval of the Government of the Philippines. Today, IRRI is one of the 15 nonprofi t international research centers that is a member of the CGIAR Consortium (www.cgiar.org). It is supported in part by government funding agencies, foundations, the private sector, and nongovernment organizations. The responsibility for this publication rests with the International Rice Research Institute. Copyright International Rice Research Institute 2012 This publication is copyrighted by the International Rice Research Institute (IRRI) and is licensed for use under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License (Unported). Unless otherwise noted, users are free to copy, duplicate, or reproduce, and distribute, display, or transmit any of the articles or portions of the articles, and to make translations, adaptations, or other derivative works under the following conditions: Attribution: The work must be attributed, but not in any way that suggests endorsement by IRRI or the author(s). NonCommercial: This work may not be used for commercial purposes. ShareAlike: If this work is altered, transformed, or built upon, the resulting work must be distributed only under the same or similar license to this one. For any reuse or distribution, the license terms of this work must be made clear to others. Any of the above conditions can be waived if permission is obtained from the copyright holder. Nothing in this license impairs or restricts the author’s moral rights. -
2015 Annual Report
2015 RICE BREEDING PROGRESS REPORT California Cooperative riCe researCh foundation January 30, 2016 Rice Experiment Station P.O. Box 306, Biggs, CA 95917-0306 www.crrf.org [email protected] RICE EXPERIMENT STATION STAFF Administration Kent S. McKenzie, Ph.D. ................................................................................... Director Plant Breeding Virgilio C. Andaya, Ph.D. ..................................................... Director of Plant Breeding Farman Jodari, Ph.D. ................................................................................. Plant Breeder Stanley Omar PB. Samonte, Ph.D. ............................................................ Plant Breeder Paul L. Sanchez, Ph.D. ........................................................................ Plant Pathologist Cynthia B. Andaya, Ph.D. .................................................................. Research Scientist Plant Breeding Support Matthew A. Calloway ........................................................... Breeding Nursery Manager Baldish K. Deol ........................................................................... Plant Breeder Assistant Ravinder Singh Gakhal ............................................................... Plant Breeder Assistant Davinder Singh .......................................................................... Plant Breeder Assistant Christopher A. Putz .................................................................... Plant Breeder Assistant Michael J. Lynch ....................................................................... -

We Really Have Many Drinks. Please Enjoy Each One
We really have many drinks. Please enjoy each one. HOW TO BEGIN BLENDED/SINGLE MALT YOUR EVENING 1oz / 2oz Nikka From the Barrel, Japan $14 / 22 Japanese G&T $12 gin, Fentiman’s tonic, yuzu honey, grapefruit oil Nikka Coffey Grain, Japan $16 / 25 Nikka Coffey Malt, Japan $16 / 25 Whisky Highball $12 Nikka Pure Malt Red, Japan $18 / 27 Suntory Toki whisky, soda water, lemon oil Nikka Pure Malt Black, Japan $18 / 27 Amaro Long Island Iced Tea $14 Nikka Super Rare Old, Japan $16 / 25 Averna, Cynar, Fernet Branca, and Amaro Montenegro Hibiki Harmony, Japan $21 / 32 served long over ice, topped up with Chinotto soda Toki Suntory, Japan $9 / 14 Mars Iwai Tradition, Japan $18 / 27 Akashi White Oak, Japan $14 / 22 KT COCKTAILS Aberlour A’bunadh Cask Strength, Speyside $14 / 21 Dark End of the Street $16 Port Charlotte Heavy Peat, Islay $12 / 18 Suntory Toki whisky, Cynar, Takara plum wine, Boker’s bitters, lemon oil, Amarena cherry Oban 14, Highlands $20 / 31 The Arran 14yr, Islands $20 / 31 Flowers on the Wall $14 Suntory Roku gin, Cocchi Rosa vermouth, Aperol, orange twist BRANDY Shore Leave Martini $14 Calvados Père Magloire VSOP $12 / 19 Sheringham Seaside gin, Yamagata Junmai sake, Dolin Blanc vermouth, orange bitters, nori olive Pierre Ferrand 1840 VS $14 / 20 Remy Martin XO $40 / 70 My Private Tokyo $15 Amaretto Disaronno, Takara plum wine, Martini Dry, lemon, egg white, plum sea salt GIN White Sbagliato $13 Aviation $8 / 13 Cocchi Americano, Luxardo Bitter Bianco, Bittermen’s Ampersand $8 / 13 Gentian, sparkling wine Botanist, Islay Dry -

Non-GMO Project Verified Products
Non-GMO Project Verified Products Chamblee Store, South Region Whole Foods Market, as a part of its mission to offer food in its most natural state, has created a Non-GMO Project Verified Product shopping list. Developed in partnership with the Non-GMO Project, a non-profit organization dedicated to allowing consumers to make informed choices and to ensuring sustained availability of non-GMO options, this shopping list highlights products that have been reviewed and verified by an independent third party to ensure that food production follows rigorous best practices for GMO avoidance. We hope that this proves to be a valuable shopping tool for you! Products that have been verified have the easy -to-recognize seal featured at the top of this shopping list. Unfortunately, due to cross-contamination and pollen drift, very few products in the U.S. are completely free of GMOs. The Non-GMO Project standard is a process-based standard that avoids the intentional use of GMO ingredients by providing suppliers with procedures and best practices for minimizing the presence of GMO ingredients. Thank you for shopping Whole Foods Market and your support of the Non-GMO Project! Baby & Child Products Earth's Best (Cont'd) Sweet Potatoes First Stage Dr. Bronner's Mild Liquid Baby Soap - 32 oz. Multi-Grain Cereal Oats, Spelt And Barley Blend Mild Liquid Baby Soap - 16 oz. Organic Sweet Potatoes Mild Liquid Baby Soap Whole Grain Oatmeal Cereal Mild Baby Bar Soap Baby Food 2nd Breakfast Blueberry Banana Baby & Infant Food HAPPYBABY Pouches Apricot & Sweet