Medical Marijuana Program Practitioner Guidance for the Use of Medical Marijuana to Treat Opioid Use Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medications to Treat Opioid Use Disorder Research Report
Research Report Revised Junio 2018 Medications to Treat Opioid Use Disorder Research Report Table of Contents Medications to Treat Opioid Use Disorder Research Report Overview How do medications to treat opioid use disorder work? How effective are medications to treat opioid use disorder? What are misconceptions about maintenance treatment? What is the treatment need versus the diversion risk for opioid use disorder treatment? What is the impact of medication for opioid use disorder treatment on HIV/HCV outcomes? How is opioid use disorder treated in the criminal justice system? Is medication to treat opioid use disorder available in the military? What treatment is available for pregnant mothers and their babies? How much does opioid treatment cost? Is naloxone accessible? References Page 1 Medications to Treat Opioid Use Disorder Research Report Discusses effective medications used to treat opioid use disorders: methadone, buprenorphine, and naltrexone. Overview An estimated 1.4 million people in the United States had a substance use disorder related to prescription opioids in 2019.1 However, only a fraction of people with prescription opioid use disorders receive tailored treatment (22 percent in 2019).1 Overdose deaths involving prescription opioids more than quadrupled from 1999 through 2016 followed by significant declines reported in both 2018 and 2019.2,3 Besides overdose, consequences of the opioid crisis include a rising incidence of infants born dependent on opioids because their mothers used these substances during pregnancy4,5 and increased spread of infectious diseases, including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.6 Effective prevention and treatment strategies exist for opioid misuse and use disorder but are highly underutilized across the United States. -
The Opioid Epidemic: What Labs Have to Do with It?
The Opioid Epidemic: What labs have to do with it? Ewa King, Ph.D. Associate Director of Health RIDOH State Health Laboratories Analysis. Answers. Action. www.aphl.org Overview • Overdose trends • Opioids and their effects • Analytical testing approaches • Toxicology laboratories Analysis. Answers. Action. www.aphl.org Opioid overdose crisis 1 Analysis. Answers. Action. www.aphl.org Opioid overdose crisis 2 Analysis. Answers. Action. www.aphl.org Opiates and Opioids • Opiates vs. Opioids • Opiates: Naturally occurring, derived from the poppy plant • Opioids: “Opiate-like” drugs in effects, not chemical structure Includes opiates • Narcotic analgesics • CNS depressants • DEA Schedule I or II controlled substances • Additive effect with other CNS depressant drugs Analysis. Answers. Action. www.aphl.org Efficacy of Opioids • How do opioids work? • Bind with opioid receptors • Brain, spinal cord, GI tract, and throughout the body • Pain, emotion, breathing, movement, and digestion Opioid Receptor Analysis. Answers. Action. www.aphl.org Effects of Opioids Physiological Psychological • Pain relief • Drowsiness/ sedation • Cough suppression • Mental confusion • GI motility • Loss of memory • Respiratory depression • Lethargy/ apathy • Pupillary constriction • Euphoria/ tranquility • Itching • Mood swings • Constipation • Depression • Dependence • Withdrawal • Dependence Analysis. Answers. Action. www.aphl.org Opiates 1 Opiates • Naturally occurring alkaloids Opium • Latex from the opium poppy plant Codeine: • Mild to moderate pain • Antitussive Morphine: • Severe pain • Metabolite of codeine and heroin Analysis. Answers. Action. www.aphl.org Opiates 2 Semi-synthetic Opiates: • Synthesized from a natural opiate Heroin: • Schedule I narcotic Hydrocodone (Vicodin): • Mild to moderate pain • Metabolizes to hydromorphone (Dilaudid) Oxycodone (Oxycontin/Percocet): • Moderate to severe pain • Metabolizes to oxymorphone (Opana) Analysis. Answers. Action. -

What Are the Treatments for Heroin Addiction?
How is heroin linked to prescription drug abuse? See page 3. from the director: Research Report Series Heroin is a highly addictive opioid drug, and its use has repercussions that extend far beyond the individual user. The medical and social consequences of drug use—such as hepatitis, HIV/AIDS, fetal effects, crime, violence, and disruptions in family, workplace, and educational environments—have a devastating impact on society and cost billions of dollars each year. Although heroin use in the general population is rather low, the numbers of people starting to use heroin have been steadily rising since 2007.1 This may be due in part to a shift from abuse of prescription pain relievers to heroin as a readily available, cheaper alternative2-5 and the misperception that highly pure heroin is safer than less pure forms because it does not need to be injected. Like many other chronic diseases, addiction can be treated. Medications HEROIN are available to treat heroin addiction while reducing drug cravings and withdrawal symptoms, improving the odds of achieving abstinence. There are now a variety of medications that can be tailored to a person’s recovery needs while taking into account co-occurring What is heroin and health conditions. Medication combined with behavioral therapy is particularly how is it used? effective, offering hope to individuals who suffer from addiction and for those around them. eroin is an illegal, highly addictive drug processed from morphine, a naturally occurring substance extracted from the seed pod of certain varieties The National Institute on Drug Abuse (NIDA) has developed this publication to Hof poppy plants. -
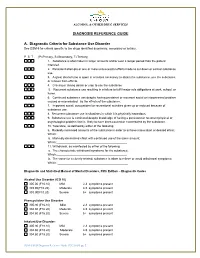
DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance
ALCOHOL & OTHER DRUG SERVICES DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance Use Disorder See DSM-5 for criteria specific to the drugs identified as primary, secondary or tertiary. P S T (P=Primary, S=Secondary, T=Tertiary) 1. Substance is often taken in larger amounts and/or over a longer period than the patient intended. 2. Persistent attempts or one or more unsuccessful efforts made to cut down or control substance use. 3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from effects. 4. Craving or strong desire or urge to use the substance 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. 6. Continued substance use despite having persistent or recurrent social or interpersonal problem caused or exacerbated by the effects of the substance. 7. Important social, occupational or recreational activities given up or reduced because of substance use. 8. Recurrent substance use in situations in which it is physically hazardous. 9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. 10. Tolerance, as defined by either of the following: a. Markedly increased amounts of the substance in order to achieve intoxication or desired effect; Which:__________________________________________ b. Markedly diminished effect with continued use of the same amount; Which:___________________________________________ 11. Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for the substance; Which:___________________________________________ b. -

The Opioid Crisis and the Black/African American Population: an Urgent Issue
THE OPIOID CRISIS AND THE BLACK/AFRICAN AMERICAN POPULATION: AN URGENT ISSUE THE OPIOID CRISIS AND THE BLACK/AFRICAN AMERICAN POPULATION: AN URGENT ISSUE U.S. Department of Health and Human Services Substance Abuse and Mental Health Services Administration Office of Behavioral Health Equity Table of Contents Introduction ...................................................................................................................................................... 3 i. Purpose of the Issue Brief ........................................................................................................................ 3 ii. Sources of Information ............................................................................................................................ 4 Opioids in Black/African American Communities: Context .................................................................. 4 i. What Do the National Data Show? ........................................................................................................ 4 ii. Routes to Opioid Misuse and Overdose Deaths: Pain Management, Illicit Drug Use, and Opioid Comorbidities in Black/African American Communities .................................................... 6 iii. Challenges to Prevention, Treatment, and Recovery .......................................................................... 7 Strategies to Address Opioid Misuse and OUD in Black/African American Communities ............ 9 i. Standard Treatment ................................................................................................................................ -

Phencyclidine: an Update
Phencyclidine: An Update U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse and Mental Health Administration Phencyclidine: An Update Editor: Doris H. Clouet, Ph.D. Division of Preclinical Research National Institute on Drug Abuse and New York State Division of Substance Abuse Services NIDA Research Monograph 64 1986 DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administratlon National Institute on Drug Abuse 5600 Fishers Lane Rockville, Maryland 20657 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 NIDA Research Monographs are prepared by the research divisions of the National lnstitute on Drug Abuse and published by its Office of Science The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integrative research reviews. its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisors MARTIN W. ADLER, Ph.D. SIDNEY COHEN, M.D. Temple University School of Medicine Los Angeles, California Philadelphia, Pennsylvania SYDNEY ARCHER, Ph.D. MARY L. JACOBSON Rensselaer Polytechnic lnstitute National Federation of Parents for Troy, New York Drug Free Youth RICHARD E. BELLEVILLE, Ph.D. Omaha, Nebraska NB Associates, Health Sciences Rockville, Maryland REESE T. JONES, M.D. KARST J. BESTEMAN Langley Porter Neuropsychiatric lnstitute Alcohol and Drug Problems Association San Francisco, California of North America Washington, D.C. DENISE KANDEL, Ph.D GILBERT J. BOTV N, Ph.D. College of Physicians and Surgeons of Cornell University Medical College Columbia University New York, New York New York, New York JOSEPH V. -

The Impact of Cannabis Access Laws on Opioid Prescribing
Journal of Health Economics 69 (2020) 102273 Contents lists available at ScienceDirect Journal of Health Economics j ournal homepage: www.elsevier.com/locate/econbase The impact of cannabis access laws on opioid prescribing a,∗ b c Benjamin J. McMichael , R. Lawrence Van Horn , W. Kip Viscusi a Assistant Professor of Law, University of Alabama School of Law, Box 870382, 101 Paul W. Bryant Drive East, Tuscaloosa, AL, 35487, United States b Associate Professor of Management and Law, Executive Director of Health Affairs, Owen Graduate School of Management, Vanderbilt University, 401 21st Avenue South, Nashville, TN, 37203, United States c University Distinguished Professor of Law, Economics, and Management, Vanderbilt University Law School. 131 21st Avenue South, Nashville, TN, 37203, United States a r a t i c l e i n f o b s t r a c t Article history: While recent research has shown that cannabis access laws can reduce the use of prescrip- Received 5 October 2018 tion opioids, the effect of these laws on opioid use is not well understood for all dimensions Received in revised form 17 July 2019 of use and for the general United States population. Analyzing a dataset of over 1.5 bil- Accepted 7 December 2019 lion individual opioid prescriptions between 2011 and 2018, which were aggregated to the Available online 14 December 2019 individual provider-year level, we find that recreational and medical cannabis access laws reduce the number of morphine milligram equivalents prescribed each year by 11.8 and 4.2 JEL classification: percent, respectively. These laws also reduce the total days’ supply of opioids prescribed, I180 the total number of patients receiving opioids, and the probability a provider prescribes K19 any opioids net of any offsetting effects. -

Dextrorphan Binds to Opioid Receptors in Guinea-Pig Brain Membranes And
Proc. Natl. Acad. Sci. USA Vol. 87, pp. 1629-1632, March 1990 Pharmacology Dextrorphan binds to opioid receptors in guinea-pig brain membranes and is an antagonist at opioid receptors in myenteric plexus (binding/guinea-pig ileum/levorphanol/stereoselectivity) AVRAM GOLDSTEIN AND ASHA NAIDU Department of Pharmacology, Stanford University, Stanford, CA 94305 Contributed by Avram Goldstein, December 11, 1989 ABSTRACT Dextrorphan (+)-tartrate, purified by re- LaRoche); [D-Ala,MePhe4,Gly-ol5]enkephalin (DAGO; Pe- peated crystallization to remove all traces of the enantiomer ninsula Laboratories) (2); trans-3,4-dichloro-N-methyl- levorphanol, binds to IL, 6, and K sites on guinea-pig brain N-[2-(1-pyrrolidinyl)cyclohexyl]benzeneacetamide methane- membranes with lower affinities (by a factor of400-3200) than sulfonate (U50,488; Upjohn) (3); (-)-naloxone hydrochloride levorphanol. In the guinea-pig ileum myenteric plexus longi- (NAL; Endo Laboratories, New York); normorphine hydro- tudinal muscle preparation (GPI), dextrorphan, at 100-200 chloride (NOR) and (+)-naloxone hydrochloride (National ,uM, inhibits the electrically stimulated twitch, but this action Institute on Drug Abuse); N-methyl-D-aspartic acid (NMDA), is not blocked or reversed by naloxone; both (+)- and (-)- aminophosphonovalerate, norepinephrine (levarterenol), at- naloxone produce similar non-opioid twitch inhibition at com- ropine, and eserine (physostigmine) (Sigma). parable concentrations. At 10-20 jaM, dextrorphan' blocks and Preparation ofDEXp. [3H]LEV (Ro 1-5431/701, Hoffmann- reverses the twitch inhibition due to ,u and KWagonists, but the LaRoche; 17.4 Ci/mmol; 1 Ci = 37 GBq) was purified' by blockade can be overcome only partially by increasing the preparative reversed-phase HPLC (Waters, C18 AgBondaPak, agonist concentration. -

Opioid Use Disorders
AD APTING YOUR PRACTIC E Recommendations for the Care of Homeless Patients with Opioid Use Disorders Opioid Use Disorders March 2014 ADAPTING YOUR PRACTICE Recommendations for the Care of Homeless Patients with Opioid Use Disorders Health Care for the Homeless Clinicians’ Network March 2014 Health Care for the Homeless Clinicians’ Network Adapting Your Practice: Recommendations for the Care of Homeless Patients with Opioid Use Disorders was developed with support from the Bureau of Primary Health Care, Health Resources and Services Administration, U.S. Department of Health and Human Services. All material in this document is in the public domain and may be used and reprinted without special permission. Citation as to source, however, is appreciated. Suggested citation: Meges D, Zevin B, Cookson E, Bascelli L, Denning P, Little J, Doe-Simkins M, Wheeler E, Watlov Phillips S, Bhalla P, Nance M, Cobb G, Tankanow J, Williamson J, Post P (Ed.). Adapting Your Practice: Recommendations for the Care of Homeless Patients with Opioid Use Disorders. 102 pages. Nashville: Health Care for the Homeless Clinicians' Network, National Health Care for the Homeless Council, Inc., 2014. DISCLAIMER This publication was made possible by grant number U30CS09746 from the Health Resources & Services Administration, Bureau of Primary Health Care. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Health Resources & Services Administration. i ADAPTING YOUR PRACTICE Recommendations for the Care of Homeless Patients with Opioid Use Disorders Health Care for the Homeless Clinicians’ Network PREFACE Clinicians experienced in homeless health care routinely adapt their practice to foster better outcomes for their patients. -
HHS Guide for Clinicians on the Appropriate Dosage Reduction Or
This HHS Guide for Clinicians on the Appropriate Dosage HHS Guide for Clinicians on the Reduction or Discontinuation of Long-Term Opioid Analgesics provides advice to clinicians who are contemplating or initiating a reduction in opioid dosage or discontinuation Appropriate Dosage Reduction of long-term opioid therapy for chronic pain. In each case the clinician should review the risks and benefits of the or Discontinuation of current therapy with the patient, and decide if tapering is appropriate based on individual circumstances. Long-Term Opioid Analgesics After increasing every year for more than a decade, annual needs.2,3,4 Coordination across the health care team is critical. opioid prescriptions in the United States peaked at 255 million in Clinicians have a responsibility to provide or arrange for 2012 and then decreased to 191 million in 2017.i More judicious coordinated management of patients’ pain and opioid-related opioid analgesic prescribing can benefit individual patients as problems, and they should never abandon patients.2 More well as public health when opioid analgesic use is limited to specific guidance follows, compiled from published guidelines situations where benefits of opioids are likely to outweigh risks. (the CDC Guideline for Prescribing Opioids for Chronic Pain2 At the same time opioid analgesic prescribing changes, such and the VA/DoD Clinical Practice Guideline for Opioid Therapy as dose escalation, dose reduction or discontinuation of long- for Chronic Pain3) and from practices endorsed in the peer- term opioid analgesics, have potential to harm or put patients at reviewed literature. risk if not made in a thoughtful, deliberative, collaborative, and measured manner. -

(Oxycodone) RATIONALE for INCLUSION in PA PROGRAM
OXYCODONE IR (oxycodone) RATIONALE FOR INCLUSION IN PA PROGRAM Background Oxycodone hydrochloride, a pure opioid agonist, is used in the treatment of moderate to severe pain (1-2). The precise mechanism of action is unknown; however, specific opioid receptors in the CNS have been identified and are considered to play a role in the therapeutic effects of the drug (3). Oxycodone is a Schedule II controlled substance and can be abused in a manner similar to other opioid agonists, legal or illicit. This should be considered when prescribing or dispensing oxycodone in a situation where misuse, abuse, or diversion are a concern (1). Regulatory Status FDA-approved indications: Oxycodone IR tablets and capsules are immediate-release (IR) oral formulations of oxycodone hydrochloride indicated for the management of moderate to severe pain where the use of an opioid analgesic is appropriate. Oxycodone hydrochloride oral solution 100 mg/5 mL (20 mg/mL) is an opioid analgesic indicated for the management of moderate to severe acute and chronic pain in opioid-tolerant patients (1-3). Limitations of use: (1) Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, reserve Oxycodone IR for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or non-opioid combination products): • Have not been tolerated, or are not expected to be tolerated • Have not provided adequate analgesia or are not expected to provide adequate analgesia The Oxycodone IR has boxed warnings for the following (1-6): • Respiratory depression is the chief hazard of opioid agonists, including morphine sulfate, which if not immediately recognized and treated, may lead to respiratory arrest and death. -

Benefit/Risk Assessment of Prescription Opioid Antitussive Products for Treatment of Cough in Pediatric Patients
Background Document Pediatric Advisory Committee Meeting September 11, 2017 Benefit/Risk Assessment of Prescription Opioid Antitussive Products for Treatment of Cough in Pediatric Patients Table of Contents 1. Introduction ..........................................................................................................................................2 2. Regulatory History of Prescription Opioid Antitussive Products .......................................................... 3 Codeine ..................................................................................................................................................... 3 Hydrocodone............................................................................................................................................. 5 Pediatric Study Requirements for Prescription Opioid Antitussives ........................................................ 8 3. Safety of Opioid Antitussive Products among Children and Adolescents ............................................ 9 Codeine and Risk of Respiratory Depression and Death Due to Ultra‐rapid Metabolism........................9 Hydrocodone and Risk of Respiratory Depression and Death................................................................ 12 Risks of misuse, abuse, addiction, overdose and death with opioid antitussives .................................. 13 4. Utilization of Products to Treat Cough in Pediatric Patients .............................................................. 14 5. Treatment Alternatives for Cough