Nuclear Receptors & Endocrine / Metabolic Disruption
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cryptorchidism and Endocrine Disrupting Chemicals ⇑ Helena E
Molecular and Cellular Endocrinology 355 (2012) 208–220 Contents lists available at SciVerse ScienceDirect Molecular and Cellular Endocrinology journal homepage: www.elsevier.com/locate/mce Review Cryptorchidism and endocrine disrupting chemicals ⇑ Helena E. Virtanen , Annika Adamsson Department of Physiology, University of Turku, Finland article info abstract Article history: Prospective clinical studies have suggested that the rate of congenital cryptorchidism has increased since Available online 25 November 2011 the 1950s. It has been hypothesized that this may be related to environmental factors. Testicular descent occurs in two phases controlled by Leydig cell-derived hormones insulin-like peptide 3 (INSL3) and tes- Keywords: tosterone. Disorders in fetal androgen production/action or suppression of Insl3 are mechanisms causing Cryptorchidism cryptorchidism in rodents. In humans, prenatal exposure to potent estrogen diethylstilbestrol (DES) has Testis been associated with increased risk of cryptorchidism. In addition, epidemiological studies have sug- Endocrine disrupting chemical gested that exposure to pesticides may also be associated with cryptorchidism. Some case–control stud- ies analyzing environmental chemical levels in maternal breast milk samples have reported associations between cryptorchidism and chemical levels. Furthermore, it has been suggested that exposure levels of some chemicals may be associated with infant reproductive hormone levels. Ó 2011 Elsevier Ireland Ltd. All rights reserved. Contents 1. Background. -

TOXIC EQUIVALENCY FACTORS for DIOXIN-LIKE Pcbs
Chemosphere, Vol. 28, No. 6, pp. 1049-1067, 1994 Perl~amon ELsevier Science Ltd Printed in Great Britain 0045-6535/94 $6.00+0.00 0045-6535(94)E0070-A TOXIC EQUIVALENCY FACTORS FOR DIOXIN-LIKE PCBs Report on a WHO-ECEH and IPCS consultation, December 1993 Ahlborg UG 1., Becking GC 2, Birnbaum LS 3, Brouwer A 4, Derks HJGM s, Feeley M6, Color G 7, Hanberg A 1, Larsen JC s, Liem AKD s, Safe SH9, Schlatter C 10, Wvern F 1, Younes M 11, Yrj~inheikki E 12 1 Karolinska Institutet, Box 210, S-171 77 Stockholm, Sweden 2IPCS/IRRU, Research Triangle Park, NC, USA; 3USEPA, Research Triangle Park, NC, USA; 4Agricultural University, Wageningen, The Netherlands; 5Nan Inst Publ Health and Environmental Protection, Bilthoven, The Netherlands; C~Iealth and Welfare Canada, Ottawa, Canada; 7Freie Universit~t Berlin, Bedin-Dahlem, Germany; 8National Food Agency, S~aorg, Denmark; 9Texas A & M University, College Station TX, USA; l°Swiss Federal Institute of Toxicology, Schwerzenbach, Ziirich, Switzerland; 11WHOEuropean Centre for Environment and Health, Bilthoven, The Netherlands; 12Occupational Safety and Health Division, Tampere, Finland (Received in Germany 10 February 1994; accepted 16 February 1994) ABSTRACT The WHO-European Centre for Environment and Health (WHO-ECEH) and the International Programme on Chemical Safety (IPCS), have initiated a project to create a data base containing information relevant to the setting of Toxic Equivalency Factors (TEFs), and, based on the available information, to assess the relative potencies and to derive consensus TEFs for PCDDs, PCDFs and dioxin-like PCBs. Available data on the relative toxicities of dioxin-like PCBs with respect to a number of endpoints were collected and analyzed. -
Examining Reproductive Health Outcomes in Females Exposed to Polychlorinated Biphenyl and Polybrominated Biphenyl Michael F
www.nature.com/scientificreports OPEN Examining Reproductive Health Outcomes in Females Exposed to Polychlorinated Biphenyl and Polybrominated Biphenyl Michael F. Neblett II1*, Sarah W. Curtis2, Sabrina A. Gerkowicz1, Jessica B. Spencer1, Metrecia L. Terrell3, Victoria S. Jiang1, M. Elizabeth Marder4, Dana Boyd Barr4, Michele Marcus5 & Alicia K. Smith 6 In 1973, accidental contamination of Michigan livestock with polybrominated biphenyls (PBBs) led to the establishment of a registry of exposed individuals that have been followed for > 40 years. Besides being exposed to PBBs, this cohort has also been exposed to polychlorinated biphenyls (PCBs), a structurally similar class of environmental pollutants, at levels similar to average US exposure. In this study, we examined the association between current serum PCB and PBB levels and various female reproductive health outcomes to build upon previous work and inconsistencies. Participation in this cross-sectional study required a blood draw and completion of a detailed health questionnaire. Analysis included only female participants who had participated between 2012 and 2015 (N = 254). Multivariate linear and logistic regression models were used to identify associations between serum PCB and PBB levels with each gynecological and infertility outcome. Additionally, a generalized estimating equation (GEE) model was used to evaluate each pregnancy and birth outcome in order to account for multiple pregnancies per woman. We controlled for age, body mass index, and total lipid levels in all analyses. A p-value of <0.05 was used for statistical signifcance. Among the women who reported ever being pregnant, there was a signifcant negative association with higher total PCB levels associating with fewer lifetime pregnancies ( β = −0.11, 95% CI = −0.21 to −0.005, p = 0.04). -

Polybrominated Biphenyls Bers of Bromine Atoms
Report on Carcinogens, Fourteenth Edition For Table of Contents, see home page: http://ntp.niehs.nih.gov/go/roc Polybrominated Biphenyls bers of bromine atoms. PBBs are usually white, off‑white, or beige powders at room temperature (IPCS 1994). All of the congeners are Separate CAS Nos. are assigned to individual polybrominated insoluble in water but readily soluble in fat. PBBs are extremely sta‑ biphenyls ble and therefore persistent in the environment. Hexabromobiphe‑ Reasonably anticipated to be human carcinogens nyl (C12H4Br6, CAS No. 36355‑01‑8), one of 101 PBBs compounds in the CAS Registry system, is the main component of the com‑ First listed in the Third Annual Report on Carcinogens (1983) mercial PBB mixtures tested in animal carcinogenicity studies as Also known as PBBs FireMaster FF‑1 (FireMaster was registered as a trademark by the Michigan Chemical Corporation, St. Louis, MI). FireMaster FF‑1 was (Br) (Br)y x produced by grinding FireMaster BP‑6, the other main commercial hexabromo biphenyl PBB mixture (of which the major components were 4.0% pentabromobiphenyls, 62.6% hexabromobiphenyls, and Polybrominated biphenyls (number of bromine atoms [x + y] = 1–10) 33.4% heptabromo biphenyls) and blending it with 2% calcium poly‑ silicate as an anticaking agent (NTP 1993). Physical and chemical Carcinogenicity properties of hexabromobiphenyl, as a representative PBB, are listed in the following table. Polybrominated biphenyls (PBBs) are reasonably anticipated to be hu- man carcinogens based on sufficient evidence of carcinogenicity from Property Information studies in experimental animals. The animal studies used Fire Master Molecular weight 627.6 FF‑1, which is a commercial mixture of polybrominated biphenyl iso‑ Melting point 72°C mers, containing a mixture of pentabromobiphenyls, hexabromo‑ Log Kow 6.39 biphenyls, and heptabromobiphenyls. -

Investigation Into Levels of Chlorinated and Brominated Organic Pollutants in Carcass Fat, Offal, Eggs and Milk Produced in Ireland
cHeMICAL Monitoring & Surveillance SerieS Investigation into levels of chlorinated and brominated organic pollutants in carcass fat, offal, eggs and milk produced in Ireland JANUARY 2010 Investigation into levels of chlorinated and brominated organic pollutants in carcass fat, offal, eggs and milk produced in Ireland JANUARY 2010 TABLE OF CONTENTS SUMMARY ................................................................................................................................................................ 2 ABBREVIATIONS ..................................................................................................................................................... 3 BACKGROUND ......................................................................................................................................................... 4 Polychlorinated dibenzodioxins and polychlorinated dibenzofurans .............................................. 4 Polychlorinated Biphenyls ............................................................................................................. 5 Toxic equivalence factors and Tolerable Intakes for PCDD/Fs and dioxin-like PCBs .................... 5 Risk assessment of PCDD/Fs and PCBs in food ........................................................................... 7 Legislation on PCDD/Fs and PCBs in food.................................................................................... 8 Brominated Flame Retardants.................................................................................................... -

Toxicological Profile for Polybrominated Biphenyls
PBBs and PBDEs 487 11. REFERENCES *Adinolfi M. 1985. The development of the human blood-CSF-brain barrier. Dev Med Child Neurol 27:532-537. *Adlercreutz H. 1995. Phytoestrogens: Epidemiology and a possible role in cancer protection. Environ Health Perspect Suppl 103(7):103-112. *Agency for Toxic Substances and Disease Registry. 1989. Decision guide for identifying substance- specific data needs related to toxicological profiles. Notice. Federal Register 54(174):37618-37634. *Agency for Toxic Substances and Disease Registry. 1990. Biomarkers of organ damage or dysfunction for the renal, hepatobiliary, and immune systems. Atlanta, GA: Subcommittee on Biomarkers of Organ Damage and Dysfunction. *Agency for Toxic Substances and Disease Registry. 1994. Toxicological profile for chlorodibenzofurans. Atlanta, GA: U.S. Department of Health and Human Services. *Agency for Toxic Substances and Disease Registry. 1998. Toxicological profile for chlorinated dibenzo-p-dioxins. Atlanta, GA: U.S. Department of Health and Human Services. *Agency for Toxic Substances and Disease Registry. 2000. Toxicological profile for polychlorinated biphenyls. Atlanta, GA: U.S. Department of Health and Human Services. *Ahmadizadeh M, Kuo C-H, Echt R, et al. 1984. Effect of polybrominated biphenyls, B-naphthoflavone and phenobarbital on arylhydrocarbon hydrolase activities and chloroform-induced nephrotoxicity and hepatotoxicity in male C57BL/6J and DBA/2J mice. Toxicology 31:343-352. *Akoso BT, Sleight SD, Aust SD, et al. 1982a. Pathologic effects of purified polybrominated biphenyl congeners in rats. J Am Coll Toxicol 1:1-21. *Akoso BT, Sleight SD, Nachreiner RF, et al. 1982b. Effects of purified polybrominated biphenyl congeners on the thyroid and pituitary glands in rats. -

Environmental Pollutants and Marine Mammal Health: the Potential Impact of Hydrocarbons and Halogenated Hydrocarbons on Immune System Dysfunction
/. CETACEAN RES. MANAGE. (SPECIAL ISSUE I), 223-248, 1999 Environmental pollutants and marine mammal health: The potential impact of hydrocarbons and halogenated hydrocarbons on immune system dysfunction DAVID BUSBEE*, IAN TIZARD+, JEFFREY SroiT1, DAVID FERRICR*, ELLEN Orr-REEVEst Contact e-mail: [email protected] ABSTRACT This paper provides a detailed review of the immunotoxicological effects of environmental pollutants on the health of marine mammals, particularly in relation to their impact on the immune system and mechanisms of toxicity. Environmental pollutants are increasingly implicated (both directly and indirectly) with the onset of infectious disease and related mortality incidents in marine mammals,. The release of chemicals into the marine environment and the subsequent bioaccumulation up the food chain may pose a serious threat to marine mammals inhabiting contaminated areas; this has been documented in various studies of pollutant concentrations in tissue samples and large scale mass mortalities. Data correlating pollutant residues with altered reproductive/developmental states, and immune system dysfunction in particular, are reported for terrestrial mammals and suggest a similar association in marine mammals. Immunology is emphasised as a tool for assessing marine mammal health using quantitative and qualitative techniques to establish the effects of chemical pollutants. This has become increasingly important in relation to the subsequent dangers that may be posed to humans through any indirect exposure via the food chain. KEYWORDS: POLLUTANTS: ORGANOCHLORINES; DISEASE; REVIEW; IMMUNOSUPPRESSION INTRODUCTORY CONCEPTS OF IMMUNOTOXICITY IN MARINE MAMMALS During the last twenty years there has been increasing attention directed toward the role of chemical pollutants as causative factors in the onset of disease. -
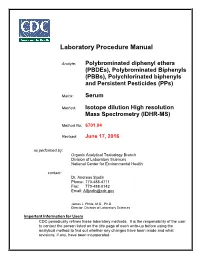
Pbdes), Polybrominated Biphenyls (Pbbs), Polychlorinated Biphenyls and Persistent Pesticides (Pps
Laboratory Procedure Manual Analyte: Polybrominated diphenyl ethers (PBDEs), Polybrominated Biphenyls (PBBs), Polychlorinated biphenyls and Persistent Pesticides (PPs) Matrix: Serum Method: Isotope dilution High resolution Mass Spectrometry (IDHR-MS) Method No: 6701.04 Revised: June 17, 2016 as performed by: Organic Analytical Toxicology Branch Division of Laboratory Sciences National Center for Environmental Health contact: Dr. Andreas Sjodin Phone: 770-488-4711 Fax: 770-488-0142 Email: [email protected] James L. Pirkle, M.D., Ph.D. Director, Division of Laboratory Sciences Important Information for Users CDC periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. Isotope dilution High resolution Mass Spectrometry (IDHR-MS) NHANES 2015-2016 Public Release Data Set Information This document details the Lab Protocol for testing the items listed in the following table: Data File Name Variable SAS Label LBC028 PCB 28 (ng/g) LBC066 PCB 66 (ng/g) LBC074 PCB 74 (ng/g) LBC099 PCB 99 (ng/g) LBC105 PCB 105 (ng/g) LBC114 PCB 114 (ng/g) LBC118 PCB 118 (ng/g) LBC138 PCB 138 (ng/g) LBC146 PCB 146 (ng/g) LBC153 PCB 153 (ng/g) LBC156 PCB 156 (ng/g) LBC157 PCB 157 (ng/g) PCBPOL_I LBC167 PCB 167 (ng/g) LBC170 PCB 170 (ng/g) LBC178 PCB 178 (ng/g) LBC180 PCB 180 (ng/g) LBC183 PCB 183 (ng/g) LBC187 PCB 187 (ng/g) LBC189 PCB 189 (ng/g) LBC194 PCB 194 (ng/g) LBC196 PCB 196 (ng/g) LBC199 PCB 199 (ng/g) LBC206 PCB 206 (ng/g) LBC209 PCB 209 (ng/g) 1 of 62 Isotope dilution High resolution Mass Spectrometry (IDHR-MS) NHANES 2015-2016 1. -

Polybrominated Diphenyl Ethers (Pbdes)
DRAFT FOR ÉBAUCHE POUR PUBLIC COMMENTS COMMENTAIRES DU PUBLIC Canadian Environmental Protection Act, 1999 Environmental Screening Assessment Report on Polybrominated Diphenyl Ethers (PBDEs) February 2004 Environment Canada where x + y = 1 to 10 Figure 1. PBDE structure Introduction The Canadian Environmental Protection Act, 1999 (CEPA 1999) requires the Minister of the Environment and the Minister of Health to conduct screening assessments of substances that meet the categorization criteria set out in the Act and Regulations to determine, in an expeditious manner, whether substances present or may present a risk to the environment or to human health. Based on the results of a screening assessment, the Ministers can propose taking no further action with respect to the substance, adding the substance to the Priority Substances List (PSL) for further assessment, or recommending that the substance be added to the List of Toxic Substances in Schedule 1 and, where applicable, the implementation of virtual elimination. A screening assessment involves an analysis of a substance using conservative assumptions to determine whether the substance is “toxic” or capable of becoming “toxic” as defined in CEPA 1999. This environmental screening assessment examines various supporting information and develops conclusions based on a weight of evidence approach as required under Section 76.1 of CEPA 1999. The screening assessment does not present an exhaustive review of all available data; rather, it presents the most critical studies and lines of evidence supporting the conclusions. One line of evidence includes consideration of risk quotients to identify potential for ecological effects. However, other concerns that affect current or potential risk, such as persistence, bioaccumulation, chemical transformation and trends in ambient concentrations, are also examined in this report. -

Updated Technical Guidelines for the Environmentally Sound Management of Wastes Consisting Of, Containing Or Contaminated with P
Updated technical guidelines for the environmentally sound management of wastes consisting of, containing or contaminated with polychlorinated biphenyls (PCBs), polychlorinated terphenyls (PCTs) or polybrominated biphenyls (PBBs) K0760119 230307 Contents I. Introduction .............................................................................................................5 A. Scope .............................................................................................................5 B. Description, production, use and wastes ......................................................................5 1. Description.......................................................................................................5 (a) PCBs....................................................................................................5 (b) PCTs....................................................................................................5 (c) PBBs....................................................................................................6 2. Production........................................................................................................6 (a) PCBs....................................................................................................6 (b) PCTs....................................................................................................7 (c) PBBs....................................................................................................7 3. Use .............................................................................................................7 -

1.0, 2.5, 5.0, 7.5 and 10.0 Mg HBN/Kg Body Weight/Day (Po)
Abstract Brominated naphthalenes have been identified as toxic contam¬ inants of the polybrominated biphenyl mixture Firemaster, which was found to be responsible for the 1973 Michigan livestock feed contamination incident. Extensive adult and embryo/fetal toxicity was associated with consumption of the contaminated feed. In order to characterize the embryotoxic and teratogenic properties of hexabrominated naphthalenes (HBNs), the most prevalent of the brominated naphthalenes in Firemaster, pregnant C57B1/6N mice were treated on gestation days 6-15 with 0, 0.5, 1.0, 2.5, 5.0, 7.5 and 10.0 mg HBN/kg body weight/day (p.o.) and sacrificed on gestation day 18. Maternal and fetal toxicity were characterized and a complete teratological evaluation was performed. Dose-related effects on maternal body and thymus weight, and liver to body weight ratios were seen. Dose-related increases were observed for fetal subcutaneous edema, involution of lymphatic organs, delayed cranial ossification and fetal mortality. A steep dose response curve was shown for cleft palate, with 4.8% and 98.6% of the fetuses per litter affected at 1.0 and 2.5 mg/kg, respectively. Kidney lesions, best described as apparent hydronephrosis, were an even more sensitive indicator of fetal toxicity with 100% of the fetuses having bilateral dilated renal pelves at 1.0 mg/kg and 90% having at least a unilateral dilated renal pelvis at 0.5 mg/kg. A pilot teratology study conducted by dosing animals between gestation days 10-13 with 0, 10, 100 or 1000 mg HBN/kg body weight/day revealed that 100% of the fetuses had cleft palate at each of the HBN treatment levels. -

4. Mechanistic and Other Relevant Data
4. MECHANISTIC AND OTHER RELEVANT DATA 4.1 Absorption, distribution, and ensuing analytical difficulties in detection. metabolism, and excretion [Another possible explanation could be metabo- lism of the trichlorinated congener.] In this Section, the most recent Ballschmiter The gastrointestinal absorption of 10 conge- & Zell (BZ) nomenclature was used throughout ners from food was investigated using a mass (see Mills et al., 2007). For the full corresponding balance approach in seven individuals aged IUPAC nomenclature, the reader is referred to 24–81 years with different contaminant body Section 1.1, Tables 1.1–1.3. For the methyl sulfonyl burdens (Schlummer et al., 1998). The differ- metabolites, and wherever the nomenclature ence between ingested and excreted amounts of reported is unclear, the name of the metabolite the chlorinated compounds was defined as net is given as reported in the article, followed by, absorption. Nearly complete net absorption was where appropriate, the abbreviation as well as the observed for PCB-28, PCB-52, PCB-77, PCB-101, structural name (Maervoet et al., 2004; Grimm and PCB-126. Absorption of PCB-105, PCB-138, et al., 2015). PCB-153, and PCB-180 was > 60% in most volun- teers, but limited absorption was observed in the 4.1.1 Absorption three older subjects. In all cases, absorption of PCB-202 was < 52%. (a) Oral exposure (ii) Experimental systems (i) Humans Several reports have been published on the The absorption of polychlorinated biphenyls dietary absorption of PCBs, mostly individual (PCBs) was studied in four breastfed infants in congeners. Gastrointestinal absorption of conge- Sweden by Dahl et al.