The Effects of Chronic Chemogenetic Stimulation of Nucleus Accumbens on Binge Drinking, the Transcriptome, and Neuronal Morphology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lineage-Specific Evolution of the Vertebrate Otopetrin Gene Family Revealed by Comparative Genomic Analyses
Hurle et al. BMC Evolutionary Biology 2011, 11:23 http://www.biomedcentral.com/1471-2148/11/23 RESEARCHARTICLE Open Access Lineage-specific evolution of the vertebrate Otopetrin gene family revealed by comparative genomic analyses Belen Hurle1, Tomas Marques-Bonet2,3, Francesca Antonacci3, Inna Hughes4, Joseph F Ryan1, NISC Comparative Sequencing Program1,5, Evan E Eichler3, David M Ornitz6, Eric D Green1,5* Abstract Background: Mutations in the Otopetrin 1 gene (Otop1) in mice and fish produce an unusual bilateral vestibular pathology that involves the absence of otoconia without hearing impairment. The encoded protein, Otop1, is the only functionally characterized member of the Otopetrin Domain Protein (ODP) family; the extended sequence and structural preservation of ODP proteins in metazoans suggest a conserved functional role. Here, we use the tools of sequence- and cytogenetic-based comparative genomics to study the Otop1 and the Otop2-Otop3 genes and to establish their genomic context in 25 vertebrates. We extend our evolutionary study to include the gene mutated in Usher syndrome (USH) subtype 1G (Ush1g), both because of the head-to-tail clustering of Ush1g with Otop2 and because Otop1 and Ush1g mutations result in inner ear phenotypes. Results: We established that OTOP1 is the boundary gene of an inversion polymorphism on human chromosome 4p16 that originated in the common human-chimpanzee lineage more than 6 million years ago. Other lineage- specific evolutionary events included a three-fold expansion of the Otop genes in Xenopus tropicalis and of Ush1g in teleostei fish. The tight physical linkage between Otop2 and Ush1g is conserved in all vertebrates. -
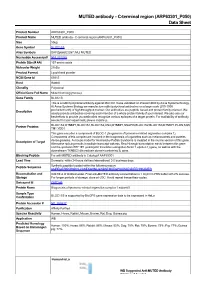
MUTED Antibody - C-Terminal Region (ARP63301 P050) Data Sheet
MUTED antibody - C-terminal region (ARP63301_P050) Data Sheet Product Number ARP63301_P050 Product Name MUTED antibody - C-terminal region (ARP63301_P050) Size 50ug Gene Symbol BLOC1S5 Alias Symbols DKFZp686E2287; MU; MUTED Nucleotide Accession# NM_201280 Protein Size (# AA) 187 amino acids Molecular Weight 21kDa Product Format Lyophilized powder NCBI Gene Id 63915 Host Rabbit Clonality Polyclonal Official Gene Full Name Muted homolog (mouse) Gene Family BLOC1S This is a rabbit polyclonal antibody against MUTED. It was validated on Western Blot by Aviva Systems Biology. At Aviva Systems Biology we manufacture rabbit polyclonal antibodies on a large scale (200-1000 Description products/month) of high throughput manner. Our antibodies are peptide based and protein family oriented. We usually provide antibodies covering each member of a whole protein family of your interest. We also use our best efforts to provide you antibodies recognize various epitopes of a target protein. For availability of antibody needed for your experiment, please inquire (). Partner Proteins BLOC1S2,DTNBP1,BLOC1S1,BLOC1S2,CNO,DTNBP1,SNAPIN,BLOC1S2,BLOC1S3,DTNBP1,PLDN,SQS TM1,YOD1 This gene encodes a component of BLOC-1 (biogenesis of lysosome-related organelles complex 1). Components of this complex are involved in the biogenesis of organelles such as melanosomes and platelet- Description of Target dense granules. A mouse model for Hermansky-Pudlak Syndrome is mutated in the murine version of this gene. Alternative splicing results in multiple transcript variants. Read-through transcription exists between this gene and the upstream EEF1E1 (eukaryotic translation elongation factor 1 epsilon 1) gene, as well as with the downstream TXNDC5 (thioredoxin domain containing 5) gene. -

University of California, San Diego
UC San Diego UC San Diego Electronic Theses and Dissertations Title The post-terminal differentiation fate of RNAs revealed by next-generation sequencing Permalink https://escholarship.org/uc/item/7324r1rj Author Lefkowitz, Gloria Kuo Publication Date 2012 Peer reviewed|Thesis/dissertation eScholarship.org Powered by the California Digital Library University of California UNIVERSITY OF CALIFORNIA, SAN DIEGO The post-terminal differentiation fate of RNAs revealed by next-generation sequencing A dissertation submitted in partial satisfaction of the requirements for the degree Doctor of Philosophy in Biomedical Sciences by Gloria Kuo Lefkowitz Committee in Charge: Professor Benjamin D. Yu, Chair Professor Richard Gallo Professor Bruce A. Hamilton Professor Miles F. Wilkinson Professor Eugene Yeo 2012 Copyright Gloria Kuo Lefkowitz, 2012 All rights reserved. The Dissertation of Gloria Kuo Lefkowitz is approved, and it is acceptable in quality and form for publication on microfilm and electronically: __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ __________________________________________________________________ Chair University of California, San Diego 2012 iii DEDICATION Ma and Ba, for your early indulgence and support. Matt and James, for choosing more practical callings. Roy, my love, for patiently sharing the ups and downs -

The NIH Catalyst from the Deputy Director for Intramural Research
— Fostering Communication and Collaboration The nihCatalyst A Publication for NIH Intramural Scientists National Institutes of Health Office of the Director Volume 15 Issue 6 November-Dece.mber i , 2007 Research Festival Research Festival of Age: Getting to the Bottom Coming Tissue Engineering and Regenerative Medicine Of the Beta Cell by Fran Pollner by Julie Wallace or some, the quest is to increase the progenitor pool of pancre- anel chair Rocky F atic beta cells, to derive stem Tuan noted that cells that can be controlled in cul- P this was the NIH ture and serve as replacements for Research Festival’s damaged or lost beta cells; for oth- first dedicated sympo- ers, the quest is for new treatments. sium on tissue engi- neering and regenera- Stem Cell Studies tive medicine, a re- Typically, cul- flection that the field tured human beta is steadily approach- cells do not prolif- ing the threshold of erate well or retain clinical application. the mature pheno- Indeed, applying type, noted Marvin biological and engi- neering principles to Gershengorn, chief Fran Pollner The Re-Generation: (left to right): Pamela Robey, N1DCR; of the Clinical En- Marvin repairing and replac- Cynthia Dunbar, NHLB1; Catherine Kuo, NIAMS; and panel docrinology Branch Gershengorn ing damaged and de- chair Rocky Tuan, NIAMS and scientific director, NIDDK, who stroyed tissues has at- has been exploring the optimization tracted researchers across NIH; scientists adipocytes, and chondrocytes derived of hIPCs (human islet cell-derived from three institutes described their on- from MSCs could indeed be made to precursor cells) for about five years. -

Human BLOC1S2 / BLOS2 Protein (GST Tag)
Human BLOC1S2 / BLOS2 Protein (GST Tag) Catalog Number: 13916-H09E General Information SDS-PAGE: Gene Name Synonym: BLOS2; CEAP; CEAP11 Protein Construction: A DNA sequence encoding the human BLOC1S2 (Q6QNY1-2) (Met1- Arg99) was fused with the GST tag at the N-terminus. Source: Human Expression Host: E. coli QC Testing Purity: > 74 % as determined by SDS-PAGE Endotoxin: Protein Description Please contact us for more information. BLOC1S2, also known as BLOS2, belongs to the BLOC1S2 family. It is a Stability: component of BLOC-1 complex. The BLOC-1 complex is composed of BLOC1S1, BLOC1S2, BLOC1S3, DTNBP1, MUTED, PLDN, Samples are stable for up to twelve months from date of receipt at -70 ℃ CNO/cappuccino and SNAPIN. The BLOC-1 complex is required for normal biogenesis of lysosome-related organelles, such as platelet dense Predicted N terminal: Met granules and melanosomes. BLOC1S2 interacts directly with BLOC1S1, Molecular Mass: BLOC1S3, MUTED, CNO/cappuccino and SNAPIN. It may play a role in cell proliferation. It also plays a role in intracellular vesicle trafficking. The recombinant human BLOC1S2 /GST chimera consists of 333 amino Functionally, BLOC1S2 gene has been proposed to participate in acids and has a predicted molecular mass of 38.7 kDa. It migrates as an processes (melanosome organization, microtubule nucleation, platelet approximately 39 KDa band in SDS-PAGE under reducing conditions. dense granule organization, positive regulation of cell proliferation, positive regulation of transcription, regulation of apoptosis, positive regulation of Formulation: transcription from RNA polymerase II promoter). Lyophilized from sterile PBS, pH 7.4 References Normally 5 % - 8 % trehalose, mannitol and 0.01% Tween80 are added as 1.Sowa ME, et al. -

A BLOC-1 Mutation Screen Reveals That PLDN Is Mutated in Hermansky-Pudlak Syndrome Type 9
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector ARTICLE A BLOC-1 Mutation Screen Reveals that PLDN Is Mutated in Hermansky-Pudlak Syndrome Type 9 Andrew R. Cullinane,1,* James A. Curry,1 Carmelo Carmona-Rivera,1 C. Gail Summers,2 Carla Ciccone,1 Nicholas D. Cardillo,1 Heidi Dorward,1 Richard A. Hess,1 James G. White,3 David Adams,1,4 Marjan Huizing,1 and William A. Gahl1,4 Hermansky-Pudlak Syndrome (HPS) is an autosomal-recessive condition characterized by oculocutaneous albinism and a bleeding diath- esis due to absent platelet delta granules. HPS is a genetically heterogeneous disorder of intracellular vesicle biogenesis. We first screened all our patients with HPS-like symptoms for mutations in the genes responsible for HPS-1 through HPS-6 and found no functional muta- tions in 38 individuals. We then examined all eight genes encoding the biogenesis of lysosome-related organelles complex-1, or BLOC-1, proteins in these individuals. This identified a homozygous nonsense mutation in PLDN in a boy with characteristic features of HPS. PLDN is mutated in the HPS mouse model pallid and encodes the protein pallidin, which interacts with the early endosomal t-SNARE syntaxin-13. We could not detect any full-length pallidin in our patient’s cells despite normal mRNA expression of the mutant transcript. We could detect an alternative transcript that would skip the exon that harbored the mutation, but we demonstrate that if this transcript is translated into protein, although it correctly localizes to early endosomes, it does not interact with syntaxin-13. -

Primepcr™Assay Validation Report
PrimePCR™Assay Validation Report Gene Information Gene Name cappuccino homolog (mouse) Gene Symbol CNO Organism Human Gene Summary This intronless gene encodes a protein that may play a role in organelle biogenesis associated with melanosomes platelet dense granules and lysosomes. A similar protein in mouse is a component of a protein complex termed biogenesis of lysosome-related organelles complex 1 (BLOC-1) and is a model for Hermansky-Pudlak syndrome. The encoded protein may play a role in intracellular vesicular trafficking. Gene Aliases BCAS4L, FLJ11230 RefSeq Accession No. NC_000004.11, NT_006051.18 UniGene ID Hs.7570 Ensembl Gene ID ENSG00000186222 Entrez Gene ID 55330 Assay Information Unique Assay ID qHsaCED0034300 Assay Type SYBR® Green Detected Coding Transcript(s) ENST00000320776 Amplicon Context Sequence GGTCGCCACTGCACCCAGCCTGTGTCTTCCAGCTCTAATCAGAAAGCTGCTTGT CGAGGGCATGGGGAATCAAACTGAATGAACTTTTCTCTGCACTGTGGCAAAAC Amplicon Length (bp) 77 Chromosome Location 4:6718880-6718986 Assay Design Exonic Purification Desalted Validation Results Efficiency (%) 100 R2 0.9992 cDNA Cq 20.69 cDNA Tm (Celsius) 80 gDNA Cq 25.49 Page 1/5 PrimePCR™Assay Validation Report Specificity (%) 100 Information to assist with data interpretation is provided at the end of this report. Page 2/5 PrimePCR™Assay Validation Report CNO, Human Amplification Plot Amplification of cDNA generated from 25 ng of universal reference RNA Melt Peak Melt curve analysis of above amplification Standard Curve Standard curve generated using 20 million copies of template diluted 10-fold to 20 copies Page 3/5 PrimePCR™Assay Validation Report Products used to generate validation data Real-Time PCR Instrument CFX384 Real-Time PCR Detection System Reverse Transcription Reagent iScript™ Advanced cDNA Synthesis Kit for RT-qPCR Real-Time PCR Supermix SsoAdvanced™ SYBR® Green Supermix Experimental Sample qPCR Human Reference Total RNA Data Interpretation Unique Assay ID This is a unique identifier that can be used to identify the assay in the literature and online. -

ISBRA 2012 Short Abstracts
1 ISBRA 20 2 SHORT ABSTRACTS 8TH INTERNATIONAL SYMPOSIUM ON BIOINFORMATICS RESEARCH AND APPLICATIONS May 21-23, 2012 University of Texas at Dallas, Dallas, TX http://www.cs.gsu.edu/isbra12/ Symposium Organizers Steering Committee Dan Gusfield, University of California, Davis Ion Mandoiu, University of Connecticutt Yi Pan, Georgia State University Marie-France Sagot, INRIA Alex Zelikovsky, Georgia State University General Chairs Ovidiu Daesku, University of Texas at Dallas Raj Sunderraman, Georgia State University Program Chairs Leonidas Bleris, University of Texas at Dallas Ion Mandoiu, University of Connecticut Russell Schwartz, Carnegie Mellon University Jianxin Wang, Central South University Publicity Chair Sahar Al Seesi, University of Connecticut Finance Chairs Anu Bourgeois, Georgia State University Raj Sunderraman, Georgia State University Web Master, Web Design Piyaphol Phoungphol J. Steven Kirtzic Sponsors NATIONAL SCIENCE DEPARTMENT OF COMPUTER SCIENCE DEPARTMENT OF COMPUTER SCIENCE FOUNDATION GEORGIA STATE UNIVESITY UNIVERSITY OF TEXAS AT DALLAS i Program Committee Members Srinivas Aluru, Iowa State University Allen Holder, Rose-Hulman Istitute of S. Cenk Sahinalp, Simon Fraser Danny Barash, Ben-Gurion Technology University University Jinling Huang, Eastern Carolina David Sankoff, University of Ottawa Robert Beiko, Dalhousie University University Russell Schwartz, Carnegie Mellon Anne Bergeron, Universite du Lars Kaderali, University of University Quebec a Montreal Heidelberg Joao Setubal, Virginia Bioinformatics Iyad Kanj, -

UC Santa Cruz UC Santa Cruz Electronic Theses and Dissertations
UC Santa Cruz UC Santa Cruz Electronic Theses and Dissertations Title Sample-Specific Cancer Pathway Analysis Using PARADIGM Permalink https://escholarship.org/uc/item/9zr859ks Author Benz, Stephen Charles Publication Date 2012 Peer reviewed|Thesis/dissertation eScholarship.org Powered by the California Digital Library University of California UNIVERSITY OF CALIFORNIA SANTA CRUZ SAMPLE-SPECIFIC CANCER PATHWAY ANALYSIS USING PARADIGM A dissertation submitted in partial satisfaction of the requirements for the degree of DOCTOR OF PHILOSOPHY in BIOMOLECULAR ENGINEERING AND BIOINFORMATICS by Stephen C. Benz June 2012 The Dissertation of Stephen C. Benz is approved: Professor David Haussler, Chair Professor Joshua Stuart Professor Nader Pourmand Dean Tyrus Miller Vice Provost and Dean of Graduate Studies Copyright c by Stephen C. Benz 2012 Table of Contents List of Figures v List of Tables xi Abstract xii Dedication xiv Acknowledgments xv 1 Introduction 1 1.1 Identifying Genomic Alterations . 2 1.2 Pathway Analysis . 5 2 Methods to Integrate Cancer Genomics Data 10 2.1 UCSC Cancer Genomics Browser . 11 2.2 BioIntegrator . 16 3 Pathway Analysis Using PARADIGM 20 3.1 Method . 21 3.2 Comparisons . 26 3.2.1 Distinguishing True Networks From Decoys . 27 3.2.2 Tumor versus Normal - Pathways associated with Ovarian Cancer 29 3.2.3 Differentially Regulated Pathways in ER+ve vs ER-ve breast can- cers . 36 3.2.4 Therapy response prediction using pathways (Platinum Free In- terval in Ovarian Cancer) . 38 3.3 Unsupervised Stratification of Cancer Patients by Pathway Activities . 42 4 SuperPathway - A Global Pathway Model for Cancer 51 4.1 SuperPathway in Ovarian Cancer . -

Lecture6-For Web.Key
1 2 Holly Wichman Jim Bull 3 4 Phage Population Growth at 43° C A A* H B K ! X174 C G D E J F 5 6 7 8 9 10 Adaptation for cryptic coloration 11 12 Mouse coat color genetics Endothelin receptor B (piebald) mutation Genes Phenotypes Mouse Adamts20, Ectodysplasin-A (Eda), Endothelin 3 Human ligand (Edn3),Endothelin receptor B (Ednrb) Epidermal growth factor receptor (Egfr), Fibroblast growth factor receptor2 (Fgfr2), Inhibitor of kappaB kinase gamma (Ikbkg), C-kit receptor (kit), Ligand for c-kit receptor (kitl), Keratin complex 2, gene 17 (Krt2-17), LIM homeodomain protein 1 (Lmx1a), Mucolipin 3(Mcoln3), Pax-3 transcription factor (Pax3), Sideroflexin (Sfxn1), Neural crest transcription factor (Snai2), Sry-box containing gene 10 (Sox10), Sry-box containing gene 18 (Sox18), T- box 15 (tbx15), Growth factor (Wnt1), Growth factor (Wnt3a), Tyrosinase-related protein 2 (Tyrp2/Dct), Glycoprotein (Gpnmb), Membrane- assoc. transporter protein (Matp), Member of RAS oncogene family (Rab38), Silver protein (Pmel17), Tyrosinase (Tyr), Tyrosinas-related protein 1 (Tyrp1), Beta 3 subunit of adaptor protein 3 (Ap3b1), Delta subunit of adaptor protein 2 (Ap3d), Vacuoloar protein sorting 33a (Vps33a), Cno, Hermansky-Pudlak syndrome gene 1 (Hps1), Hermansky-Pudlak gene 3 (Hps3), Hermansky-Pudlak gene 4 (Hps4), Hermansky- Pudlak gene 5 (Hps5), Hermansky-Pudlak gene 6 (Hps6), Lysosomal trafficking regulator (Lyst), Ocular albinism type 1 (Oa1), Pallidin (Pldn), Rab geranylgeranyl transferase (Rabgtta), Melanophilin (Mlph), Myosin type Va (Myo5a), Myosin type -

Negative Feedback Control of Neuronal Activity by Microglia
Article Negative feedback control of neuronal activity by microglia https://doi.org/10.1038/s41586-020-2777-8 Ana Badimon1,2,3, Hayley J. Strasburger1,2,3, Pinar Ayata1,2,3,4, Xinhong Chen5, Aditya Nair5, Ako Ikegami6,7, Philip Hwang1,2,3, Andrew T. Chan1,2,3, Steven M. Graves8, Joseph O. Uweru9, Received: 26 November 2019 Carola Ledderose10, Munir Gunes Kutlu11, Michael A. Wheeler12, Anat Kahan5, Accepted: 28 August 2020 Masago Ishikawa1, Ying-Chih Wang13, Yong-Hwee E. Loh1, Jean X. Jiang14, D. James Surmeier15, Simon C. Robson16,17, Wolfgang G. Junger10, Robert Sebra13, Erin S. Calipari11,18,19,20,21, Published online: 30 September 2020 Paul J. Kenny1, Ukpong B. Eyo9, Marco Colonna22, Francisco J. Quintana12,23, Hiroaki Wake6,7, Check for updates Viviana Gradinaru5 & Anne Schaefer1,2,3,4 ✉ Microglia, the brain’s resident macrophages, help to regulate brain function by removing dying neurons, pruning non-functional synapses, and producing ligands that support neuronal survival1. Here we show that microglia are also critical modulators of neuronal activity and associated behavioural responses in mice. Microglia respond to neuronal activation by suppressing neuronal activity, and ablation of microglia amplifes and synchronizes the activity of neurons, leading to seizures. Suppression of neuronal activation by microglia occurs in a highly region-specifc fashion and depends on the ability of microglia to sense and catabolize extracellular ATP, which is released upon neuronal activation by neurons and astrocytes. ATP triggers the recruitment of microglial protrusions and is converted by the microglial ATP/ADP hydrolysing ectoenzyme CD39 into AMP; AMP is then converted into adenosine by CD73, which is expressed on microglia as well as other brain cells. -

Molecular Karyotyping Using an SNP Array for Genomewide Genotyping
916 J Med Genet: first published as 10.1136/jmg.2004.022855 on 9 December 2004. Downloaded from ORIGINAL ARTICLE Molecular karyotyping using an SNP array for genomewide genotyping A Rauch, F Ru¨schendorf, J Huang, U Trautmann, C Becker, C Thiel, K W Jones, A Reis, P Nu¨rnberg ............................................................................................................................... J Med Genet 2004;41:916–922. doi: 10.1136/jmg.2004.022855 Background: Chromosomal imbalances are a major cause of developmental defects as well as cancer and often constitute the key in identification of novel disease related genes. Classical cytogenetic methods are limited in resolution and dependent on highly skilled labour, while methods with higher resolution, based on molecular cytogenetics approaches such as matrix CGH, are not widely available. Methods: We have developed and evaluated a method we term ‘‘molecular karyotyping’’, using readily See end of article for available and easy to handle oligonucleotide arrays originally designed for parallel genomewide analysis authors’ affiliations of over 10 000 SNPs. We show that we can easily and reliably detect unbalanced chromosomal ....................... aberrations of various sizes from as little as 250 ng of DNA on a single microarray, based on fluorescence Correspondence to: intensity information from clusters of SNPs. Andre´Reis, Institute of Results: We determined the resolution of this method through analysis of 20 trios with 21 previously Human Genetics, confirmed subtle aberrations sizing between 0.2 and 13 Mb. Duplications and deletions of at least 5 Mb Schwabachanlage 10, 91054 Erlangen, in size were reliably detectable, but detection of smaller aberrations was dependent on the number of Germany; reis@humgenet.