Ph.D. Og Speciale
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Curriculum Vitae
CURRICULUM VITAE STEVEN GITELIS, M.D. PERSONAL DATA: Professional Address: Midwest Orthopaedics at Rush 1611 West Harrison St. Suite 300 Chicago, Illinois 60612 (312) 563-2600 E-Mail: [email protected] CURRENT APPOINTMENTS/ACTIVITIES: Trustee Rush University Associate Dean Surgery Rush Medical College Associate Chief Medical Officer Rush University Chief of Surgery Rush University President Elect Medical Staff Rush University Director Cancer Research Rush University Surgical Services Executive Committee Rush University Executive Committee Rush University Patient Safety Officer Orthopedic Surgery Rush University Rush Credentialing Committee Rush Medical Quality Committee Rush Surgical Quality Committee Rush Bylaws Committee Rush University Committee on Committees Ends 2012 Editor Emeritus Rush Orthopaedic Journal Vice Chairman Department of Orthopedic Surgery Rush Medical College Treasurer Medical Staff Rush University Medical Center Ends 2010 Rush University Committee on Committees Rush University Psychiatry Chairman Search Committee 2010 Past President Rush Surgical Society Treasurer 20th Century Orthopedic Association Biological Implants Committee AAOS Ends 2013 Chairman Task Force Technology Oversight Committee AAOS Ends 2010 Director Rush Center for Limb Preservation Rush Medical College Professor of Orthopaedic Oncology (Endowed Chair) Past President, Musculoskeletal Tumor Society Director, Section of Orthopedic Oncology Rush-Presbyterian-St. Luke's Medical Center, Chicago, Illinois Director, Bone and Tissue Bank of Gift of Hope -

Patient Guide for a Hip Replacement
Day of surgery: ____________________ Expected discharge home: ____________________ Surgeon: ____________________ Phone number: ____________________ Bring this guide with you to the hospital on the day of your surgery 4100492 (17-10) 2 Introduction This information guide will help you understand what is involved in hip arthroplasty (hip replacement). We hope the information in this booklet will help you prepare for your surgery •••••••••••••••••••••••••••••••••••••••••••••••••••••• About Hôpital Montfort Hôpital Montfort is a Francophone academic health care institution that provides quality care in both official languages and works with its partners to improve the health of communities. Montfort strives for excellence and wants to be a hospital of choice for its personalized patient care, its workplace, teaching and research. Our daily actions are guided by the values of compassion, commitment, excellence and respect. WARNING This guide does not replace the advice of your care provider. Please consult your care provider to assess if the information presented in this guide applies to your situation. The content of this guide was prepared by Vancouver Coastal Health and adapted by Hôpital Montfort. 3 Your Health Care: Be Involved! • Be involved in your health care. Speak up if you have questions or concerns about your care. • Tell a member of your health care team about your past illnesses and your current health condition. • Tell your health team if you have any food or medication allergies. • Make sure you know what to do when you leave the hospital. •••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••• Your Interprofessional Plan of Care • Your hospital admission for your total hip replacement will follow an “interprofessional plan of care” more commonly called a "Clinical Pathway". -

Sarcoma of the Lower Limb: Reconstructive Surgeon's Perspective
Published online: 2019-05-08 THIEME Review Article 55 Sarcoma of the Lower Limb: Reconstructive Surgeon’s Perspective Zhixue Lim1 Sophia A. Strike1 Mark E. Puhaindran1 1Department of Hand and Reconstructive Microsurgery, National Address for correspondence Zhixue Lim, MRCS (Edin), Department of University Hospital, Singapore, Singapore Hand and Reconstructive Microsurgery, National University Hospital, NUHS Tower Block, Level 11, 1E Kent Ridge Road, Singapore 119228, Singapore (e-mail: [email protected]). Indian J Plast Surg 2019;52:55–61 Abstract Management of sarcomas in the lower extremities have evolved from amputations to limb-preserving surgeries with evidence to support that they have equal overall Keywords survival, albeit with better functional outcome. The challenge of reconstruction lies ► sarcoma in providing a durable, functional, and aesthetically pleasing limb. However, limb- ► lower extremity preserving intention should not delay interventions that provide a survival benefit such ► reconstruction as chemotherapy and radiotherapy. The advent of radiotherapy and chemotherapy also ► vascularised bone has implications on wound healing and should be considered during the reconstruc- graft tive process. This article reviews the methodical approach, reconstructive strategies, ► soft tissue and considerations for the reconstructive surgeon with respect to the lower extremity reconstruction after sarcoma excision. who described a systematic approach to limb-preserving Introduction surgery in his article “Conservative surgery in the treatment Sarcomas are a diverse group of neoplasms that account of bone tumours,” where he shared his personal experience for approximately 1% of adult malignancies and 7 to 15% of in combining radiotherapy and surgical excision, with the 1 pediatric malignancies. The range of histological subtypes possibility of bone transplantation after resection of bone contributes to the varied prognoses. -

Rotationplasty Offers Greater Functionality for Patients with Cancer
Johns Hopkins Framework Orthopaedic Surgery NEWS FROM JOHNS HOPKINS MEDICINE Winter 2016 Rotationplasty Offers Greater Functionality for Patients with Cancer aya oberstein was diagnosed with osteosarcoma of Mthe distal femur in 2012, at age 9. After she completed chemotherapy, Maya’s treatment options Since Maya Oberstein’s initial 9.5-hour procedure, Carol Morris has been following were an above-knee up every six months to monitor her progress. amputation, limb salvage side. Cosmetically, if you’re sitting, it’s nice if the with an internal prosthesis or a knees are even.” Morris recalls her initial reluctance about the more unconventional approach: Post-op procedure. “I thought it was a physically challenging If you believe in yourself, rotationplasty. Carol Morris, thing to do to a child when prosthetics had made chief of Johns Hopkins’ tremendous advancements,” she says. “As I gained you can do anything.” more experience in the field, I began to appreciate —MAYA OBERSTEIN Orthopaedic Oncology Division, the limitations of internal prostheses and the is one of a select group of surgeons functionality rotationplasty could provide. For the in the United States who perform right parents and the right child, under the right set of circumstances, rotationplasty is a good operation. this alternative reconstructive It’s much more functional than an above-knee procedure. Morris counseled Maya amputation.” Traditional prostheses, especially growing and her family on the available protheses, are more restrictive than the modified options. “She was the first doctor transtibial prosthesis, limiting a patient’s ability to who asked me how I was feeling,” participate not only in sports, but in typical activities such as running, dancing and jumping. -

Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers Version 4.0 – October 2013
Children’s OncologyLong-Term Group Long-Term Follow-UpFollow-Up Guidelines for Survivors of Childhood,Guidelines Adolescent, and Young Adult Cancer Version 4.0 – October 2013 for Survivors of Childhood, Adolescent, and Young Adult Cancers www.survivorshipguidelines.org Version 4.0 October 2013 Copyright 2013 © Children’s Oncology Group All rights reserved worldwide Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers Version 4.0 – October 2013 www.survivorshipguidelines.org Copyright 2013 © Children’s Oncology Group All rights reserved worldwide Contents Content Outline vi Section # Page Gender Potential Late Effect Abstract vii 13 15 Female Gonadal dysfunction (ovarian) Disclaimer and Notice of Proprietary Rights viii 14 17 Acute myeloid leukemia; myelodysplasia Guidelines Panel of Experts x 15 18 Pulmonary fibrosis Guidelines Task Force Membership 2009–2012 xi 16 19 Cataracts Guidelines Health Link Authors xvi 17 20 Urinary tract toxicity Guidelines Health Link Reviewers xviii 18 21 Bladder malignancy Guidelines Development Task Force – Initial Versions xix 19 22 Renal toxicity Guidelines Reviewers – Initial Versions xx 20 23 Ototoxicity Introductory Material xxii 21 25 Peripheral sensory neuropathy; Introduction xxiii 22 26 Renal toxicity Explanation of Scoring xxviii (n/a) [Removed from v4: Dyslipidemia] Instructions for Use xxix 23 27 Neurocognitive deficits New to Version 4.0 xxxiv 24 29 Clinical leukoencephalopathy 25 31 No known late effects 26 32 Hepatic dysfunction; veno-occlusive disease -
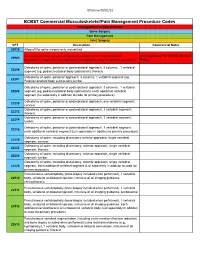
Commercial MSK Procedure Code List Effective 09.01.21.Xlsx
Effective 09/01/21 BCBST Commercial Musculoskeletal/Pain Management Procedure Codes Investigational or Non-Covered Spine Surgery Pain Management Joint Surgery CPT Description Commercial Notes 20930 Allograft for spine surgery only morselized Computer-assisted surgical navigational procedure for musculoskeletal Investigational Per BCBST Medical 20985 procedures, image-less (List separately in addition to code for primary procedure) Policy Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22206 segment (eg, pedicle/vertebral body subtraction); thoracic Osteotomy of spine, posterior approach, 3 columns, 1 vertebral segment (eg. 22207 Pedicle/vertebral body subtraction);lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22208 segment (eg, pedicle/vertebral body subtraction); each additional vertebral segment (list separately in addition to code for primary procedure) Osteotomy of spine, posterior or posterolateral approach, one vertebral segment; 22210 cervical Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22212 thoracic Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22214 lumbar Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22216 each additional vertebral segment (List separately in addition to primary procedure) Osteotomy of spine, including discectomy anterior approach, single vertebral 22220 segment; cervical Osteotomy of spine, including discectomy, anterior approach, single -

Hip Impingement and Osteoarthritis. Hip Arthroscopy, Resurfacing, Or Replacement: Is It Time for Surgery?
Hip Impingement and Osteoarthritis. Hip Arthroscopy, Resurfacing, or Replacement: Is it Time for Surgery? Bryan Whitfield, MD [email protected] Hip Operations • Background of hip diagnoses • Treatment of hip pathology • Surgery candidates • Time for surgery? • Cases Intra-articular hip pain - diagnoses • FAI (femoroacetabular impingement) / acetabular labrum tear • Neck of the femur and rim of the socket run into each other • Tear the labrum. • Articular cartilage damage possible • Labrum: fluid management, stability, and seal of the joint • Osteoarthritis • Socket and ball both coated in a layer of cartilage • Arthritis is the wearing away, loss of or damage to the cartilage coating (articular cartilage) Intra-articular hip pain - diagnoses • FAI (femoroacetabular impingement) / acetabular labrum tear • Neck of the femur and rim of the socket run into each other • Tear the labrum. • Articular cartilage damage possible • Labrum: fluid management, stability, and seal of the joint • Osteoarthritis • Socket and ball both coated in a layer of cartilage • Arthritis is the wearing away, loss of or damage to the cartilage coating (articular cartilage) Intra-articular hip pain - diagnoses • FAI (femoroacetabular impingement) / acetabular labrum tear • Neck of the femur and rim of the socket run into each other • Tear the labrum. • Articular cartilage damage possible • Labrum: fluid management, stability, and seal of the joint • Osteoarthritis • Socket and ball both coated in a layer of cartilage • Arthritis is the wearing away, loss -
Statistical Analysis Plan
~ GILEAU STATISTICAL ANALYSIS PLAN Study Title: A Phase 2, Randomized, Open Label Study to Evaluate the Efficacy and Safety ofTenofovir Alafenamide (fAF) versus Tenofovir Disoproxil Fumarate (fDF)-containing Regimens in Subjects with Chmnic HBV Infection and Stage 2 or Greater Chronic Kidney Disease Who Have Received a Liver Transplant Name of Test Drug: Tenofovir Alafenamide (fAF) Study Number: GS-US-320-3912 Protocol Version (Date): Amendment 2 (28 March 2017) Analysis Type: Week 24 Analysis Plan Version: Version 1.0 Analysis Plan Date: 19 March 2018 ..._ ...... Analysis Plan Author(s): PD______ CONFIDENTIAL AND PROPRIETARY INFORMATION TAF GS-US-320-3912 Statistical Analysis Plan – Week 24 Analysis Version 1.0 TABLE OF CONTENTS TABLE OF CONTENTS ..............................................................................................................................................2 LIST OF IN-TEXT TABLES........................................................................................................................................4 LIST OF ABBREVIATIONS........................................................................................................................................5 1. INTRODUCTION ................................................................................................................................................8 1.1. Study Objectives ......................................................................................................................................8 1.2. Study Design ............................................................................................................................................9 -

Van Nes Rotationplasty As a Treatment Method for Ewing's
CASE REPORT – OPEN ACCESS International Journal of Surgery Case Reports 4 (2013) 893–897 Contents lists available at ScienceDirect International Journal of Surgery Case Reports jou rnal homepage: www.casereports.com Van Nes rotationplasty as a treatment method for Ewing’s sarcoma in ଝ a 14-month-old ∗ Jagmeet S. Bhamra , Hani B. Abdul-Jabar, David McKenna, Stephen Ng Man Sun, Elizabeth Gillott, Robin Pollock Bone Tumour Unit, Royal National Orthopaedic Hospital, Brockley Hill, Stanmore, Middlesex HA7 4LP, UK a r t i c l e i n f o a b s t r a c t Article history: INTRODUCTION: In recent years, the rotationplasty procedure has become popular amongst tumour sur- Received 11 January 2013 geons as an alternative to endoprosthetic replacement or amputation. There are very few documented Received in revised form 26 June 2013 cases of this technique in young patients with malignancy. Accepted 19 July 2013 PRESENTATION OF CASE: We describe an extremely rare case of Ewing’s sarcoma in a 14-month-old Available online 6 August 2013 boy that involved the entire length of the left femur. At initial presentation, pulmonary metastatic spread had occurred and there was no neurovascular involvement. Complete response to neo-adjuvant Keywords: chemotherapy was achieved prior to performing the definitive surgical procedure. 14-Month-old DISCUSSION: This case highlights the many reconstructive options and difficulties encountered in man- Ewing’s sarcoma Femur aging such extremely young patients with aggressive malignant disease. In this case, a complete femoral Outcome excision was necessary and various treatment options were explored. These included irradiation and Treatment options re-implantation, endoprosthetic replacement and manufacturing a custom growing prosthesis. -

Dr. Mark Dolan Specializes in Hip and Knee Replacement Surgery, Hip Resurfacing, and Hip Arthroscopy/Hip Preservation Surgery
Dr. Mark Dolan specializes in hip and knee replacement surgery, hip resurfacing, and hip arthroscopy/hip preservation surgery. Dr. Dolan is originally from South Bend, Indiana and a graduate of the University of Notre Dame. He attended Indiana University School of Medicine before moving to Chicago to continue his education in orthopaedic surgery as a resident in Northwestern University Feinberg School of Medicine’s Department of Orthopaedic Surgery. After residency he completed a fellowship in Adult Reconstruction and Joint Replacement Surgery at the Hospital for Special Surgery in New York where he gained advanced training in hip and knee replacement surgery, hip resurfacing, and revision total joint surgery. Following this year long fellowship, he stayed at the Hospital for Special Surgery to obtain additional experience in providing care for young adults with hip pain. This included additional study in hip arthroscopy and hip preservation surgery. Dr. Dolan has a specific interest in hip disorders and strives to provide comprehensive care to patients suffering from hip pain. This includes non-operative treatment as well as total joint replacement, hip resurfacing, and arthroscopic hip surgery (athletic hip injuries, hip joint preservation surgery, femoracetabular impingement (FAI), and acetabular labral injuries). Dr. Dolan utilizes this wide array of treatment options to best serve his patients, working with each patient to develop a focused and individualized treatment plan. As a former varsity soccer player at Notre Dame and an active runner and skier, Dr. Dolan appreciates the importance of maintaining an active lifestyle. His goal is to relieve your pain and improve your mobility, thereby allowing you to return to an active life. -

The Endlock Tumor Prosthesis with Short-Length Fixation: a Clinical Study
An Original Study The Endlock Tumor Prosthesis With Short-Length Fixation: A Clinical Study Leonhard E. Ramseier, MD, Clement M. Werner, MD, Hilaire A. C. Jacob, PhD, and G. Ulrich Exner, MD early stability has been reported,10 and the advantages of ABSTRACT cementless fixation in revision cases have been maintained. Anchorage of segmental replacement prostheses in However, fixation over a long length of stem has the dis- diaphyseal bone remains a challenge in lower limb advantage of potential stress-shielding of the surrounding reconstructions. We developed and studied a new pros- bone.8,10-18 Interestingly, the prosthetic design is seldom thesis design that features an intramedullary anchorage implicated as a possible cause of aseptic loosening.10,19 system for which finite element analysis predicted favor- Encouraged by the good clinical and radiologic results able bone remodeling. We retrospectively analyzed the 20 cases of all patients who underwent implantation of the reported with the thrust plate hip prosthesis, a device new stem. Their data were prospectively collected. with a very short segmental fixation to bone, we proposed Twenty-four patients (25 prosthetic reconstructions a new design of diaphyseal anchorage and explored its using diaphyseal fixation of the prosthesis) had 18 pri- theoretical advantages by finite element analysis.21 The mary implantations and 7 revision cases. At a mean fol- short-length fixation in this design has shown a definitive low-up of 61 months, TESS (Toronto Extremity Salvage advantage over long-length fixation. The stress pattern Score) and MSTS (Musculoskeletal Tumor Society within the bone surrounding the prosthesis confirmed that Rating Scale score) were 80% and 65% that of a nor- shortening of the on-growth area in length increases the mal extremity, respectively. -

Dr. Cornett Named L. Thomas Hood, MD Professor of Orthopaedic Surgery
Breaking News for alumni and friends of the University of Nebraska Medical Center Department of Orthopaedic Surgery Nebraska Medicine—Bellevue locations. For his dedication to teaching, the orthopaedic residents selected Dr. Cornett to receive the department’s Outstanding Instructor Award. After completing a master’s degree in physical therapy, Dr. Cornett obtained his medical degree from UNMC. He completed residency at the University of Wisconsin in Madison and a spine surgery fellowship at the University of Pittsburgh Medical Center. Dr. Cornett’s clinical expertise is all aspects of adult spine surgery (cervical, thoracic and lumbar). In his spine-only practice, he treats a variety of conditions, including degenerative Dr. Cornett named L. Thomas Hood, MD conditions/arthritis, spinal stenosis, myelopathy, spondylolisthesis, disc Professor of Orthopaedic Surgery herniations, instability, scoliosis, tumors and trauma. Chris Cornett, MD, associate professor of Orthopaedic Surgery and Dr. Cornett serves on multiple UNMC Rehabilitation, has been named to the second L. Thomas Hood, MD, committees, including the Continuing Professor of Orthopaedic Surgery. Medical Education Committee and the This professorship is awarded to Dr. Cornett joined the Department of Faculty Senate. He also participates in faculty who have followed in Dr. Orthopaedic Surgery and Rehabilitation several Nebraska Medicine advisory Hood’s footsteps by establishing high in 2011 and is the department’s and operational committees. He is standards in patient care, education vice-chair of clinical services. He is an active member of many local and and research—inspiring orthopaedic also the medical director of both the national professional organizations surgeons of the future to maintain the Comprehensive Spine Program and and societies, including the American department’s mission and standard of Outpatient Physical & Occupational Academy of Orthopaedic Surgeons excellence.