Sarcoma of the Lower Limb: Reconstructive Surgeon's Perspective
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Curriculum Vitae
CURRICULUM VITAE STEVEN GITELIS, M.D. PERSONAL DATA: Professional Address: Midwest Orthopaedics at Rush 1611 West Harrison St. Suite 300 Chicago, Illinois 60612 (312) 563-2600 E-Mail: [email protected] CURRENT APPOINTMENTS/ACTIVITIES: Trustee Rush University Associate Dean Surgery Rush Medical College Associate Chief Medical Officer Rush University Chief of Surgery Rush University President Elect Medical Staff Rush University Director Cancer Research Rush University Surgical Services Executive Committee Rush University Executive Committee Rush University Patient Safety Officer Orthopedic Surgery Rush University Rush Credentialing Committee Rush Medical Quality Committee Rush Surgical Quality Committee Rush Bylaws Committee Rush University Committee on Committees Ends 2012 Editor Emeritus Rush Orthopaedic Journal Vice Chairman Department of Orthopedic Surgery Rush Medical College Treasurer Medical Staff Rush University Medical Center Ends 2010 Rush University Committee on Committees Rush University Psychiatry Chairman Search Committee 2010 Past President Rush Surgical Society Treasurer 20th Century Orthopedic Association Biological Implants Committee AAOS Ends 2013 Chairman Task Force Technology Oversight Committee AAOS Ends 2010 Director Rush Center for Limb Preservation Rush Medical College Professor of Orthopaedic Oncology (Endowed Chair) Past President, Musculoskeletal Tumor Society Director, Section of Orthopedic Oncology Rush-Presbyterian-St. Luke's Medical Center, Chicago, Illinois Director, Bone and Tissue Bank of Gift of Hope -

Rotationplasty Offers Greater Functionality for Patients with Cancer
Johns Hopkins Framework Orthopaedic Surgery NEWS FROM JOHNS HOPKINS MEDICINE Winter 2016 Rotationplasty Offers Greater Functionality for Patients with Cancer aya oberstein was diagnosed with osteosarcoma of Mthe distal femur in 2012, at age 9. After she completed chemotherapy, Maya’s treatment options Since Maya Oberstein’s initial 9.5-hour procedure, Carol Morris has been following were an above-knee up every six months to monitor her progress. amputation, limb salvage side. Cosmetically, if you’re sitting, it’s nice if the with an internal prosthesis or a knees are even.” Morris recalls her initial reluctance about the more unconventional approach: Post-op procedure. “I thought it was a physically challenging If you believe in yourself, rotationplasty. Carol Morris, thing to do to a child when prosthetics had made chief of Johns Hopkins’ tremendous advancements,” she says. “As I gained you can do anything.” more experience in the field, I began to appreciate —MAYA OBERSTEIN Orthopaedic Oncology Division, the limitations of internal prostheses and the is one of a select group of surgeons functionality rotationplasty could provide. For the in the United States who perform right parents and the right child, under the right set of circumstances, rotationplasty is a good operation. this alternative reconstructive It’s much more functional than an above-knee procedure. Morris counseled Maya amputation.” Traditional prostheses, especially growing and her family on the available protheses, are more restrictive than the modified options. “She was the first doctor transtibial prosthesis, limiting a patient’s ability to who asked me how I was feeling,” participate not only in sports, but in typical activities such as running, dancing and jumping. -

Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers Version 4.0 – October 2013
Children’s OncologyLong-Term Group Long-Term Follow-UpFollow-Up Guidelines for Survivors of Childhood,Guidelines Adolescent, and Young Adult Cancer Version 4.0 – October 2013 for Survivors of Childhood, Adolescent, and Young Adult Cancers www.survivorshipguidelines.org Version 4.0 October 2013 Copyright 2013 © Children’s Oncology Group All rights reserved worldwide Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers Version 4.0 – October 2013 www.survivorshipguidelines.org Copyright 2013 © Children’s Oncology Group All rights reserved worldwide Contents Content Outline vi Section # Page Gender Potential Late Effect Abstract vii 13 15 Female Gonadal dysfunction (ovarian) Disclaimer and Notice of Proprietary Rights viii 14 17 Acute myeloid leukemia; myelodysplasia Guidelines Panel of Experts x 15 18 Pulmonary fibrosis Guidelines Task Force Membership 2009–2012 xi 16 19 Cataracts Guidelines Health Link Authors xvi 17 20 Urinary tract toxicity Guidelines Health Link Reviewers xviii 18 21 Bladder malignancy Guidelines Development Task Force – Initial Versions xix 19 22 Renal toxicity Guidelines Reviewers – Initial Versions xx 20 23 Ototoxicity Introductory Material xxii 21 25 Peripheral sensory neuropathy; Introduction xxiii 22 26 Renal toxicity Explanation of Scoring xxviii (n/a) [Removed from v4: Dyslipidemia] Instructions for Use xxix 23 27 Neurocognitive deficits New to Version 4.0 xxxiv 24 29 Clinical leukoencephalopathy 25 31 No known late effects 26 32 Hepatic dysfunction; veno-occlusive disease -
Statistical Analysis Plan
~ GILEAU STATISTICAL ANALYSIS PLAN Study Title: A Phase 2, Randomized, Open Label Study to Evaluate the Efficacy and Safety ofTenofovir Alafenamide (fAF) versus Tenofovir Disoproxil Fumarate (fDF)-containing Regimens in Subjects with Chmnic HBV Infection and Stage 2 or Greater Chronic Kidney Disease Who Have Received a Liver Transplant Name of Test Drug: Tenofovir Alafenamide (fAF) Study Number: GS-US-320-3912 Protocol Version (Date): Amendment 2 (28 March 2017) Analysis Type: Week 24 Analysis Plan Version: Version 1.0 Analysis Plan Date: 19 March 2018 ..._ ...... Analysis Plan Author(s): PD______ CONFIDENTIAL AND PROPRIETARY INFORMATION TAF GS-US-320-3912 Statistical Analysis Plan – Week 24 Analysis Version 1.0 TABLE OF CONTENTS TABLE OF CONTENTS ..............................................................................................................................................2 LIST OF IN-TEXT TABLES........................................................................................................................................4 LIST OF ABBREVIATIONS........................................................................................................................................5 1. INTRODUCTION ................................................................................................................................................8 1.1. Study Objectives ......................................................................................................................................8 1.2. Study Design ............................................................................................................................................9 -

Van Nes Rotationplasty As a Treatment Method for Ewing's
CASE REPORT – OPEN ACCESS International Journal of Surgery Case Reports 4 (2013) 893–897 Contents lists available at ScienceDirect International Journal of Surgery Case Reports jou rnal homepage: www.casereports.com Van Nes rotationplasty as a treatment method for Ewing’s sarcoma in ଝ a 14-month-old ∗ Jagmeet S. Bhamra , Hani B. Abdul-Jabar, David McKenna, Stephen Ng Man Sun, Elizabeth Gillott, Robin Pollock Bone Tumour Unit, Royal National Orthopaedic Hospital, Brockley Hill, Stanmore, Middlesex HA7 4LP, UK a r t i c l e i n f o a b s t r a c t Article history: INTRODUCTION: In recent years, the rotationplasty procedure has become popular amongst tumour sur- Received 11 January 2013 geons as an alternative to endoprosthetic replacement or amputation. There are very few documented Received in revised form 26 June 2013 cases of this technique in young patients with malignancy. Accepted 19 July 2013 PRESENTATION OF CASE: We describe an extremely rare case of Ewing’s sarcoma in a 14-month-old Available online 6 August 2013 boy that involved the entire length of the left femur. At initial presentation, pulmonary metastatic spread had occurred and there was no neurovascular involvement. Complete response to neo-adjuvant Keywords: chemotherapy was achieved prior to performing the definitive surgical procedure. 14-Month-old DISCUSSION: This case highlights the many reconstructive options and difficulties encountered in man- Ewing’s sarcoma Femur aging such extremely young patients with aggressive malignant disease. In this case, a complete femoral Outcome excision was necessary and various treatment options were explored. These included irradiation and Treatment options re-implantation, endoprosthetic replacement and manufacturing a custom growing prosthesis. -

The Endlock Tumor Prosthesis with Short-Length Fixation: a Clinical Study
An Original Study The Endlock Tumor Prosthesis With Short-Length Fixation: A Clinical Study Leonhard E. Ramseier, MD, Clement M. Werner, MD, Hilaire A. C. Jacob, PhD, and G. Ulrich Exner, MD early stability has been reported,10 and the advantages of ABSTRACT cementless fixation in revision cases have been maintained. Anchorage of segmental replacement prostheses in However, fixation over a long length of stem has the dis- diaphyseal bone remains a challenge in lower limb advantage of potential stress-shielding of the surrounding reconstructions. We developed and studied a new pros- bone.8,10-18 Interestingly, the prosthetic design is seldom thesis design that features an intramedullary anchorage implicated as a possible cause of aseptic loosening.10,19 system for which finite element analysis predicted favor- Encouraged by the good clinical and radiologic results able bone remodeling. We retrospectively analyzed the 20 cases of all patients who underwent implantation of the reported with the thrust plate hip prosthesis, a device new stem. Their data were prospectively collected. with a very short segmental fixation to bone, we proposed Twenty-four patients (25 prosthetic reconstructions a new design of diaphyseal anchorage and explored its using diaphyseal fixation of the prosthesis) had 18 pri- theoretical advantages by finite element analysis.21 The mary implantations and 7 revision cases. At a mean fol- short-length fixation in this design has shown a definitive low-up of 61 months, TESS (Toronto Extremity Salvage advantage over long-length fixation. The stress pattern Score) and MSTS (Musculoskeletal Tumor Society within the bone surrounding the prosthesis confirmed that Rating Scale score) were 80% and 65% that of a nor- shortening of the on-growth area in length increases the mal extremity, respectively. -

Dr. Cornett Named L. Thomas Hood, MD Professor of Orthopaedic Surgery
Breaking News for alumni and friends of the University of Nebraska Medical Center Department of Orthopaedic Surgery Nebraska Medicine—Bellevue locations. For his dedication to teaching, the orthopaedic residents selected Dr. Cornett to receive the department’s Outstanding Instructor Award. After completing a master’s degree in physical therapy, Dr. Cornett obtained his medical degree from UNMC. He completed residency at the University of Wisconsin in Madison and a spine surgery fellowship at the University of Pittsburgh Medical Center. Dr. Cornett’s clinical expertise is all aspects of adult spine surgery (cervical, thoracic and lumbar). In his spine-only practice, he treats a variety of conditions, including degenerative Dr. Cornett named L. Thomas Hood, MD conditions/arthritis, spinal stenosis, myelopathy, spondylolisthesis, disc Professor of Orthopaedic Surgery herniations, instability, scoliosis, tumors and trauma. Chris Cornett, MD, associate professor of Orthopaedic Surgery and Dr. Cornett serves on multiple UNMC Rehabilitation, has been named to the second L. Thomas Hood, MD, committees, including the Continuing Professor of Orthopaedic Surgery. Medical Education Committee and the This professorship is awarded to Dr. Cornett joined the Department of Faculty Senate. He also participates in faculty who have followed in Dr. Orthopaedic Surgery and Rehabilitation several Nebraska Medicine advisory Hood’s footsteps by establishing high in 2011 and is the department’s and operational committees. He is standards in patient care, education vice-chair of clinical services. He is an active member of many local and and research—inspiring orthopaedic also the medical director of both the national professional organizations surgeons of the future to maintain the Comprehensive Spine Program and and societies, including the American department’s mission and standard of Outpatient Physical & Occupational Academy of Orthopaedic Surgeons excellence. -
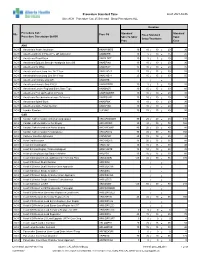
Standard Times Report
Procedure Standard Time as of: 2021-04-06 Site: ACH Procedure Cat: 25 Selected Show Procedures: ALL Duration Procedure Cat / Standard Standard Site Proc Cd Fixed Standard Procedure Description Std BK Skin To Skin/ Total Setup/Teardown Proc Case ANA ACH Anesthesia Awake Intubation ANAWKINTB 10 10 / 10 = 20 30 ACH Anesthesia Block in PACU Pre OR Admission ANABKRR 10 5 / 10 = 15 25 ACH Anesthesia Blood Patch ANABLDPT 10 5 / 5 = 10 20 ACH Anesthesia Epidural Steroid+/-Analgesia Inject SS ANAEPINJ 10 10 / 10 = 20 30 ACH Anesthesia for XRay ANAXRAY 15 10 / 10 = 20 35 ACH Anesthesia Insert Long Line IV<1 Year ANALINE<1 25 15 / 15 = 30 55 ACH Anesthesia Insert Long Line IV>1 Year ANALINE>1 25 15 / 15 = 30 55 ACH Anesthesia Intubate Only OR ANAINTB / = ACH Anesthesia Intubate Only PACU ANAINTBRR 10 5 / 5 = 10 20 ACH Anesthesia Local+/-Regional Block State Type ANABKOR 30 15 / 15 = 30 60 ACH Anesthesia Post Op Readmit to PACU ANARADMRR 10 10 / 10 = 20 30 ACH Anesthesia Pseudocholinesterase Deficiency ANAPSURR 10 10 / 10 = 20 30 ACH Anesthesia Spinal Block ANASPBK 10 10 / 10 = 20 30 ACH Anesthesia Spine Facet Injection ANASPINJ 10 10 / 10 = 20 30 ACH Lumbar Puncture LUPUNC 10 25 / 15 = 40 50 CAR ACH Cardiac Catheterization & Balloon Angioplasty HRCARCBANG 90 20 / 20 = 40 130 ACH Cardiac Catheterization w Full Biopsy HRCARCBX 90 40 / 30 = 70 160 ACH Cardiac Catheterization w Partial Biopsy HRCARCBXP 40 20 / 20 = 40 80 ACH Cardiac Catheterization+/-Valvoplasty HRCARCVL 90 40 / 30 = 70 160 ACH Catheter Insertion Aphoresis CAINAPHP 20 15 / 10 = 25 45 -

Reconstructive Techniques in Musculoskeletal Tumor Surgery
Management of Pelvic and Extremity Bone Tumors Management of Pelvic Surgery Tumor in Musculoskeletal Techniques Reconstructive Reconstructive Techniques in Musculoskeletal Tumor Surgery Management of Pelvic and Extremity Bone Tumors Michaël P.A. Bus Michaël P.A. Michaël P.A. Bus 49073 Michaël Bus cover en kaartje.indd 1 28-02-18 11:33 Reconstructive Techniques in Musculoskeletal Tumor Surgery - Management of Pelvic and Extremity Bone Tumors Michaël P.A. Bus 49073 Michaël Bus.indd 1 21-02-18 09:08 Reconstructive Techniques in Musculoskeletal Tumor Surgery – Management of Pelvic and Extremity Bone Tumors PhD thesis, Leiden University, Leiden, the Netherlands Copyright © 2018 M.P.A. Bus, Amsterdam, the Netherlands All rights reserved. No parts of this thesis may be reproduced, stored in a retrieval system of any nature or by any means, without prior written consent of the author. The copyright of the articles that have been published has been transferred to the respective journals. ISBN/EAN 978-94-6332-316-1 Cover design Jeroen Luijt Photography (jeroenluijt.nl), Amsterdam, the Netherlands Lay-out Ferdinand van Nispen tot Pannerden, Citroenvlinder DTP & Vormgeving, my-thesis.nl Printing GVO Drukkers & Vormgevers B.V., Ede, the Netherlands The research projects in this thesis were supported by an unconditional research grant from implantcast GmbH, Buxtehude, Germany. Publication of this thesis was kindly supported by: Nederlandse Orthopaedische Vereniging (NOV), Universiteit Leiden, implantcast Benelux, Bislife Foundation, ChipSoft and Anna Fonds|NOREF. 49073 Michaël Bus.indd 2 21-02-18 09:08 Reconstructive Techniques in Musculoskeletal Tumor Surgery Management of Pelvic and Extremity Bone Tumors Proefschrift ter verkrijging van de graad van Doctor aan de Universiteit Leiden op gezag van Rector Magnificus prof. -

Lengthening Reconstruction Surgery for Congenital Femoral Deficiency
Lengthening Reconstruction Surgery for Congenital 13 Femoral Defciency Dror Paley and Fran Guardo Contents 13.6 Rehabilitation After Superhip and Superknee Surgery ........................... 000 13.1 Introduction.............................................. 000 13.6.1 Preoperative ............................................... 000 13.1.1 Classifcation.............................................. 000 13.6.2 Acute.......................................................... 000 13.2 Evaluating the Child with 13.6.3 First 6 Weeks After Surgery ...................... 000 Unilateral CFD......................................... 000 13.6.4 After 6 Weeks ............................................ 000 13.2.1 History ....................................................... 000 13.7 Femoral Lengthening of Type 1 CFD .... 000 13.2.2 Physical Exam............................................ 000 13.7.1 Choice of Osteotomy Level for 13.2.3 Radiographic Examination ........................ 000 Lengthening of the Congenital 13.3 Surgical Reconstructive Strategy ........... 000 Short Femur ............................................... 000 13.3.1 Step 1: Preparatory Surgery of the 13.7.2 Soft Tissue Releases for Lengthening Hip and Knee ............................................. 000 in Cases of CFD......................................... 000 13.3.2 Step 2: Serial Lengthenings of 13.7.3 Knee Instability Consideration .................. 000 the Femur ................................................... 000 13.7.4 Distal Femoral Lengthening-Ilizarov -

Evaluation and Treatment of the Painful Shoulder After Rotator Cuff-Related Surgery
Volume 10 Spring 1997 Pages 12-17 Evaluation and Treatment of the Painful Shoulder after Rotator Cuff-Related Surgery R. John Naranja Jr., M.D. and Joseph P. Iannotti, M.D., Ph.D University of Pennsylvania, Department of Orthopaedics/Shoulder & Elbow Service, Presbyterian Medical Center, 1 Cupp Pavillion, 3900 Market St., Philadelphia, PA 19104. Abstract: The management of both rotator cuff tears and symptoms related to rotator cuff disease has historically demonstrated good results with surgical treatment when conservative measures fail. In cases of persistent pain and/or disability after rotator cuff surgery, reasons for failure include misdiagnosis, post-operative complications, errors in surgical execution, and problems related to post-operative rehabilitation. The purpose of this review is to outline these major categories for failure after rotator cuff-related surgery and to define methods for their evaluation and treatment. Introduction Our understanding of rotator cuff pathology has been fostered by identifying the intrinsic vulnerability of the rotator cuff to degenerative injury secondary to its blood supply [67], as well as the extrinsic anatomic considerations which have impinged on the cuff [52,53]. The spectrum of clinical manifestations range from an asymptomatic cuff tear to advancing stages of impingement. Current consensus regarding initial treatment of cuff impingement lesions revolves around a regimen of rest, anti-inflammatory medications, and physical therapy. If these conservative measures fail, surgical treatment may be indicated. The ultimate outcome is determined by several factors, but generally, favorable results can be expected. The etiology of a poor result requires careful evaluation, however. The purpose of this review is to outline the major categories for failure after rotator cuff-related surgery and to define the methods for their evaluation and treatment. -
Our Experience with Van Nes Rotationplasty for Locally Advanced
eCommons@AKU Department of Surgery Department of Surgery December 2014 Our experience with van nes rotationplasty for locally advanced lower extremity tumours Raza Askari Aga Khan University masood umer Aga Khan University, [email protected] Mohsin-e-Azam Aga Khan University Haroon Rashid Aga Khan University, [email protected] Follow this and additional works at: http://ecommons.aku.edu/pakistan_fhs_mc_surg_surg Part of the Orthopedics Commons, and the Surgery Commons Recommended Citation Askari, R., umer, m., Mohsin-e-Azam, ., Rashid, H. (2014). Our experience with van nes rotationplasty for locally advanced lower extremity tumours. JPMA : Journal of the Pakistan Medical Association, 64(12), S-139-S-143. Available at: http://ecommons.aku.edu/pakistan_fhs_mc_surg_surg/181 28th Pak Orthocon 2014 S-139 ORIGINAL ARTICLE Our experience with Van Nes Rotationplasty for locally advanced lower extremity tumours Raza Askari, Masood Umer, Mohsin-e-Azam, Haroon-ur-Rashid Abstract Objective: To present an early experience with the time-tested technique of Van Ness Rotationplasty to save distal lmbs. Methods: Van Nes Rotationplasty for locally advanced lower extremity tumours. A reterorespective audit was conducted at Aga Khan University Hospital, Karachi, and comprised cases of bone and soft tissue sarcoma who underwent Van Ness Rotationplasty over seven years from January 2005 to December 2011. Demographic data, family history, past history, co-morbids, date since diagnosis, duration of symptoms, type of tumour, metastasis, pre- op and post-op functional status, recurrence and survival were collected. Results: Of the 351 cases of bone and soft tissue sarcoma, 9 (2.6%) underwent Van Ness Rotationplasty and were included in the study.