Hip Impingement and Osteoarthritis. Hip Arthroscopy, Resurfacing, Or Replacement: Is It Time for Surgery?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BJH24901 Hip Replacement
ORTHOPEDICS Hip Replacement Surgery PRIMARY TOTAL HIP REPLACEMENT HEALTHY HIP A primary total hip replacement is a first time hip replacement surgery. Socket lined with cartilage Muscle (acetabulum) Why have a hip replaced? The goals of a hip replacement are to get rid of hip pain and help Tendon you be more active. A hip that is stiff and painful can be replaced with an artificial joint. This is called hip prosthesis. Hip replacements also help with damaged hips caused by Ball covered arthritis, rheumatoid arthritis and other hip-related issues. with cartilage (head of the thighbone) Pelvic bone How the hip works Thighbone The hip is a ball-and-socket-joint. In this case, the ball component (femur) is attached to the top of the femur (long bone of the thigh). The acetabulum (socket) is part of the pelvis. The ball rotating in the socket helps you move your leg. With a healthy hip, smooth cartilage covering the ends of the thigh Image courtesy of Krames StayWell bone and pelvis allows the ball to glide easily inside the socket. DAMAGED HIP DAMAGED HIP With a damaged hip, the worn cartilage no longer serves as a cushion. The surfaces of these bones become rough. This Cartilage Joint damage Tendon inflammation causes pain when they rub together. The cartilage may wear away, leaving nothing to help the bones move smoothly. Arthritis can cause inflammation and swelling around the joint. This causes pain and stiffness in the hip. (continued) Images courtesy of Krames StayWell ORTHOPEDICS PRIMARY TOTAL HIP REPLACEMENT (continued) PROBLEMS FROM SURGERY Although hip replacement can help with pain, there’s also the chance that surgery will cause problems. -
Modern Advances in Joint Replacement and Rapid Recovery
Modern Advances in Joint Replacement and Rapid Recovery UCSF Osher Mini-Med School Lecture Series Jeffrey Barry, M.D. Assistant Professor of Orthopaedic Surgery Division of Adult Reconstruction University of California, San Francisco Disclosures . No relevant disclosures to this talk About Me . Bay Area Native . UCSF - U Can Stay Forever Outline . Burden of Disease and Epidemiology . The Basics of Hip and Knee Replacement . What’s improving over the last decade - Longevity - Pain Management - Hospital Stay - Thromboembolism prophylaxis - Risk Reduction Question What is the most common inpatient surgery performed in the US? 1. Percutaneous coronary angioplasty 2. Total hip replacement 3. Lumbar Laminectomy 4. Appendectomy 5. Total knee replacement Burden of Disease . Arthritis = most common cause of disability in the US . 22.7% of adults have doctor-diagnosed arthritis - 43.2% of patients with arthritis report activity limitations due to disease . By 2030: - 3.5 million TKA (673%) - 570,000 THA (174%) . Curve updated 2014 – just as predicted! Causes of Increased Utilization . Aging Population . Patients receiving arthroplasty at a younger age - Improvements in technology - Obesity Why Replace a Joint? Arthritis arthro – joint itis – inflammation What is Arthritis – Disease of Cartilage . Cartilage Degeneration - Pain - Limp - Swelling - Loss of range of motion - Eventual deformity Arthritis Affects on Your Life • Quality of Life • Independence • Movement, Walking, Exercise • Self-image • Self-esteem • Family Life • Sleep • Everything and Everybody Causes of Arthritis . Osteoarthritis - “wear and tear” . Inflammatory arthritis . Trauma, old fractures . Infection . Osteonecrosis - “lack of oxygen to the bone” . Childhood/ developmental disease Diagnosis . Clinical Symptoms + Radiographic . Radiographs – Standing or Weight bearing! . MRI is RARELY needed!!! - Expensive - Brings in other issues - Unnecessary treatment - Unnecessary explanations Knee Arthritis . -

Patient Guide for a Hip Replacement
Day of surgery: ____________________ Expected discharge home: ____________________ Surgeon: ____________________ Phone number: ____________________ Bring this guide with you to the hospital on the day of your surgery 4100492 (17-10) 2 Introduction This information guide will help you understand what is involved in hip arthroplasty (hip replacement). We hope the information in this booklet will help you prepare for your surgery •••••••••••••••••••••••••••••••••••••••••••••••••••••• About Hôpital Montfort Hôpital Montfort is a Francophone academic health care institution that provides quality care in both official languages and works with its partners to improve the health of communities. Montfort strives for excellence and wants to be a hospital of choice for its personalized patient care, its workplace, teaching and research. Our daily actions are guided by the values of compassion, commitment, excellence and respect. WARNING This guide does not replace the advice of your care provider. Please consult your care provider to assess if the information presented in this guide applies to your situation. The content of this guide was prepared by Vancouver Coastal Health and adapted by Hôpital Montfort. 3 Your Health Care: Be Involved! • Be involved in your health care. Speak up if you have questions or concerns about your care. • Tell a member of your health care team about your past illnesses and your current health condition. • Tell your health team if you have any food or medication allergies. • Make sure you know what to do when you leave the hospital. •••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••• Your Interprofessional Plan of Care • Your hospital admission for your total hip replacement will follow an “interprofessional plan of care” more commonly called a "Clinical Pathway". -

Hip Arthroscopy Is Minimally Invasive Keyhole Surgery. Usually 2-3 Small Incisions (About 1-2 Cm Long) Are Made on the Side of Your Hip
AUT Millennium, 17 Antares Place Telephone: 09 281 6733 Mairangi Bay, Auckland 0632 Fax: 09 479 3805 www.matthewboyle.co.nz [email protected] FAQ’s: Hip Arthroscopy with Dr. Boyle What is hip arthroscopy? Hip arthroscopy is minimally invasive keyhole surgery. Usually 2-3 small incisions (about 1-2 cm long) are made on the side of your hip. Special instruments and a camera are used to look inside your hip and perform the operation. What can I do until surgery? Most people can do activities as tolerated by pain. We do not routinely prescribe pain medication pre-operatively. ANATOMY What is the hip joint? The hip joint is a ball and socket joint made up of 2 bones. The ball is the head of the femur (part of your thigh bone) and the socket is the acetabulum (part of your pelvis) The hip joint is lined by special glistening tissue called articular cartilage, which provides a smooth lubricated surface for your hip joint to move freely without pain or grating. Around the rim of your acetabulum (the socket), is a special type of cartilage called your labrum. It acts to effectively deepen your socket, providing more stability to your hip. What is femoroacetabular impingement? Femoroacetabular impingement is a term used when the bones of you hip joint are not shaped properly. There are 2 types of impingement. • CAM Impingement occurs when your ball (femoral head) is not perfectly round, often described as having a bone spur or bump. • Pincer Impingement occurs when your socket (acetabulum) is too deep, directed the wrong way, or has excess bone around the rim. -

Hip Arthroscopy Will Hip Arthroscopy Work for My Patient?
Hip Arthroscopy Will hip arthroscopy work for my patient? Indications or diagnoses treated with hip arthroscopy • femoroacetabular impingement • traumatic hip subluxations/dislocations • ligamentum teres ruptures • labral tears • loose bodies • synovial disorders • articular cartilage injuries Typical symptoms for hip arthroscopy candidates 1. Anterior groin pain, deep lateral hip pain, and posterior hip pain (rarely) 2. Groin pain with activity such as rising from a chair, getting out of a car, going up / down stairs, prolonged sitting, and during athletic activity. 3. Intermittent, mechanical pain “catching” or “snapping” can be an indication of labral pathology or a snapping tendon (psoas or iliotibial band). 4. Groin pain when bringing the knee to the chest and pulling it across your body. 5. Groin pain when bringing the knee to the chest and letting the knee fall to the side. Objective findings 1. Groin pain with flexion of hip to 90 degree or greater with maximal adduction and internal rotation (Anterior Impingement) 2. Possible limited internal rotation, has normal external rotation and extension of the hip 3. Positive FABER test (groin pain with flexion, abduction and external rotation of the (figure 1) hip also known as the figure 4 position). 4. Radiological Exam (see x-ray views below) a. Evaluate for Osteoarthritic (OA) changes, advanced arthritis is a contraindication (fig. 1) c. Pincer Impingement (acetabulum) 1. Crossover sign on pelvis (fig. 3) d. CAM impingement (femur) 1. CAM bump on Frog Lateral (osseous “bump” at head-neck junction) (fig. 3) Preferred imaging X-rays: Plain x-rays are an important part of the diagnostic process. -

Periacetabular Osteotomy (PAO) of the Hip
UW HEALTH SPORTS REHABILITATION Rehabilitation Guidelines For Periacetabular Osteotomy (PAO) Of The Hip The hip joint is composed of the femur (the thigh bone) and the Lunate surface of acetabulum acetabulum (the socket formed Articular cartilage by the three pelvic bones). The Anterior superior iliac spine hip joint is a ball and socket joint Head of femur Anterior inferior iliac spine that not only allows flexion and extension, but also rotation of the Iliopubic eminence Acetabular labrum thigh and leg (Fig 1). The head of Greater trochanter (fibrocartilainous) the femur is encased by the bony Fat in acetabular fossa socket in addition to a strong, (covered by synovial) Neck of femur non-compliant joint capsule, Obturator artery making the hip an extremely Anterior branch of stable joint. Because the hip is Intertrochanteric line obturator artery responsible for transmitting the Posterior branch of weight of the upper body to the obturator artery lower extremities and the forces of Obturator membrane Ischial tuberosity weight bearing from the foot back Round ligament Acetabular artery up through the pelvis, the joint (ligamentum capitis) Lesser trochanter Transverse is subjected to substantial forces acetabular ligament (Fig 2). Walking transmits 1.3 to Figure 1 Hip joint (opened) lateral view 5.8 times body weight through the joint and running and jumping can generate forces across the joint fully form, the result can be hip that is shared by the whole hip, equal to 6 to 8 times body weight. dysplasia. This causes the hip joint including joint surfaces and the to experience load that is poorly previously-mentioned acetabular The labrum is a circular, tolerated over time, resulting in labrum. -

What Is the Impact of a Previous Femoral Osteotomy on THA?
Clin Orthop Relat Res (2019) 477:1176-1187 DOI 10.1097/CORR.0000000000000659 2018 Bernese Hip Symposium What Is the Impact of a Previous Femoral Osteotomy on THA? A Systematic Review Enrico Gallazzi MD, Ilaria Morelli MD, Giuseppe Peretti MD, Luigi Zagra MD 02/11/2020 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD30p/TQ0kcqx8yGZO9yTf1dd5lN9ZPVa7AUCC2fdK0Vq4= by https://journals.lww.com/clinorthop from Downloaded Downloaded from Received: 10 August 2018 / Accepted: 8 January 2019 / Published online: 17 April 2019 https://journals.lww.com/clinorthop Copyright © 2019 by the Association of Bone and Joint Surgeons Abstract by Background Femoral osteotomies have been widely used Questions/purposes In this systematic review, we asked: BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD30p/TQ0kcqx8yGZO9yTf1dd5lN9ZPVa7AUCC2fdK0Vq4= to treat a wide range of developmental and degenerative hip (1) What are the most common complications after THA in diseases. For this purpose, different types of proximal fe- patients who have undergone femoral osteotomy, and how mur osteotomies were developed: at the neck as well as at frequently do those complications occur? (2) What is the the trochanteric, intertrochanteric, or subtrochanteric lev- survival of THA after previous femoral osteotomy? (3) Is els. Few studies have evaluated the impact of a previous the timing of hardware removal associated with THA femoral osteotomy on a THA; thus, whether and how a complications and survivorship? previous femoral osteotomy affects the -
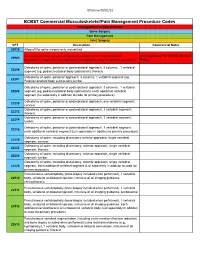
Commercial MSK Procedure Code List Effective 09.01.21.Xlsx
Effective 09/01/21 BCBST Commercial Musculoskeletal/Pain Management Procedure Codes Investigational or Non-Covered Spine Surgery Pain Management Joint Surgery CPT Description Commercial Notes 20930 Allograft for spine surgery only morselized Computer-assisted surgical navigational procedure for musculoskeletal Investigational Per BCBST Medical 20985 procedures, image-less (List separately in addition to code for primary procedure) Policy Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22206 segment (eg, pedicle/vertebral body subtraction); thoracic Osteotomy of spine, posterior approach, 3 columns, 1 vertebral segment (eg. 22207 Pedicle/vertebral body subtraction);lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22208 segment (eg, pedicle/vertebral body subtraction); each additional vertebral segment (list separately in addition to code for primary procedure) Osteotomy of spine, posterior or posterolateral approach, one vertebral segment; 22210 cervical Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22212 thoracic Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22214 lumbar Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22216 each additional vertebral segment (List separately in addition to primary procedure) Osteotomy of spine, including discectomy anterior approach, single vertebral 22220 segment; cervical Osteotomy of spine, including discectomy, anterior approach, single -

Diagnosis and Management of Snapping Hip Syndrome
Cur gy: ren lo t o R t e a s e m a u r c e h h Via et al., Rheumatology (Sunnyvale) 2017, 7:4 R Rheumatology: Current Research DOI: 10.4172/2161-1149.1000228 ISSN: 2161-1149 Review article Open Access Diagnosis and Management of Snapping Hip Syndrome: A Comprehensive Review of Literature Alessio Giai Via1*, Alberto Fioruzzi2, Filippo Randelli1 1Department of Orthopaedics and Traumatology, Hip Surgery Center, IRCCS Policlinico San Donato, Milano, Italy 2Department of Orthopaedics and Traumatology, IRCCS Policlinico San Matteo, Pavia, Italy *Corresponding author: Alessio Giai Via, Department of Orthopaedics and Traumatology, Hip Surgery Center, IRCCS Policlinico San Donato, Milano, Italy, Tel: +393396298768; E-mail: [email protected] Received date: September 11, 2017; Accepted date: November 21, 2017; Published date: November 30, 2017 Copyright: ©2017 Via AG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Background: Snapping hip is a common clinical condition, characterized by an audible or palpable snap of the hip joint. The snap can be perceived at the lateral side of the hip (external snapping hip), or at the medial (internal snapping hip). It is usually asymptomatic, but in few cases, in particular in athletes, the snap become painful (snapping hip syndrome-SHS). Materials and methods: This is a narrative review of current literature, which describes the pathogenesis, diagnosis and treatment of SHS. Conclusion: The pathogenesis of SHS is multifactorial. -

Total Joint Replacement (Hip and Knee) for Medicare, MPM 20.13
Medical Policy Subject: Total Joint Replacement (Hip and Knee) for Medicare Medical Policy #: 20.13 Original Effective Date: 07/22/2020 Status: New Policy Last Review Date: N/A Disclaimer Refer to the member’s specific benefit plan and Schedule of Benefits to determine coverage. This may not be a benefit on all plans or the plan may have broader or more limited benefits than those listed in this Medical Policy. Description Lower Extremity Major Joint Replacement or Arthroplasty refers to the replacement of the hip or knee joint. The goal of total hip or knee replacement surgery is to relieve pain and improve or increase functional activity of the member. The surgical treatment (arthroplasty) is the replacement of the damaged joint with a prosthesis. The chief reasons for joint arthroplasty (total joint replacement) are osteoarthritis, rheumatoid arthritis, traumatic arthritis (result of a fracture), osteonecrosis, malignancy, and revisions of previous surgery. Treatment options include physical therapy, analgesics or anti- inflammatory medications. The aim is to improve functional status and relieve pain. Arthroplasty failures are caused by trauma, chronic progressive joint disease, prosthetic loosening and infection of the prosthetic joint Coverage Determination Prior Authorization is required for 27130, 27132, 27134, 27447, 27486, and 27487. Logon to Pres Online to submit a request: https://ds.phs.org/preslogin/index.jsp PHP follows LCD (L36007) for Lower Extremity Major Joint Replacement for both Hip and Knee for Medicare members Note: In addition to the below items (for both knee or hip) further documentation requirements are listed in the documentation Requirement section below. Content: I. -

Hip Arthroscopy TABLE of CONTENTS
PATIENT’S GUIDE Hip Arthroscopy TABLE OF CONTENTS The Hip ....................................................................................................................................................... 2 How Do I Prepare for Surgery? ............................................................................................................ 5 24 Hours Before Surgery ......................................................................................................................... 6 The Day of Surgery ................................................................................................................................... 6 Post-Operative Rehabilitation Program ............................................................................................. 9 Crutch Training ...................................................................................................................................... 11 Follow-Up Appointments .................................................................................................................... 12 When to Call Us ..................................................................................................................................... 12 Helpful Information and Resources .................................................................................................. 12 Important Addresses and Phone Numbers ...................................................................................... 13 Welcome At UR Medicine, we understand that hip pain and dysfunction -

Hip Arthroscopy Is One of the Most Rapidly Developing Fields in Orthopedic Surgery
Hip arthroscopy is one of the most rapidly developing fields in orthopedic surgery. It is a minimally invasive surgery to correct problems in and around the hip joint. This surgery involves making 2 or 3 tiny “poke” holes in the front of the hip and placing an arthroscope, a special camera that allows one to look inside a joint, through one of those holes. The other one or two small holes are used to place special instruments inside the joint to perform the surgery. Unlike the shoulder and the knee, the hip is a very tight ball-in-socket joint. Getting into the joint can be challenging. However, there are two things that allow surgeons to get into the hip. The first and most important is the use of a special operating room table which allows the surgeon to gently pull on the patient’s foot to distract, or open up, the hip joint. An x-ray machine allows the surgeon to see the amount of distraction before any incision is made. A special well-padded post is placed against the patient’s perineum to pull against. Also, an arthroscopic pump is used to push sterile water into the joint and distend, or expand, the joint. This provides a space for surgeons to see and work. Indication for surgery The indications for hip arthroscopy, or the reasons this surgery is performed, have expanded over the last decade as equipment has improved, and new techniques have evolved. The most common reason is a condition called femoroacetabular impingement, or FAI. As stated, the hip joint is a very tight ball-in- socket joint.