PART G Lower Extremity Treatment Guidelines.Fm
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ERAS for Hip and Knee (THA and TKA) Arthroplasty – a Need to Look Beyond LOS
ASERalert November 2016 | Volume 1, Issue 1 ERAS for Hip and Knee (THA and TKA) Arthroplasty – A Need to Look Beyond LOS OFFICIAL also in this issue PUBLICATION OF ERAS for Total Enhanced ERAS for Spine Joint Arthroplasty: Recovery for Surgery: A New Past, Present and Orthopedic Frontier ASER ALERT • VOLUME 1, ISSUE 1 • aserhq.org Future Surgery 1 ANNUAL CONGRESS OF ENHANCED RECOVERY AND 2017 PERIOPERATIVE MEDICINE APRIL 27TH-29TH, 2017 HYATT REGENCY WASHINGTON ON CAPITOL HILL 400 NEW JERSEY AVE NW, WASHINGTON, D.C. 20001 For more information please visit www.aserhq.org 2 ASER ALERT • VOLUME 1, ISSUE 1 • aserhq.org Board of Directors President’s Message Officers By Tong J (TJ) Gan, MD, MHS, FRCA, President President Tong J (TJ) Gan, MD, MHS, FRCA President-Elect Julie Thacker, MD t is my great pleasure to announce Vice-President the inaugural issue of the ASER Timothy Miller MB, ChB, FRCA Newsletter. Founded in 2014, Treasurer ASER is a multi-specialty nonprofit Roy Soto, MD Iorganization with an international Secretary membership and is dedicated to the Stefan D. Holubar MD, MS, FACS, FASCRS practice of enhanced recovery in the perioperative patient through education Directors and research. We are experiencing a period of tremendous expansion and Keith A. (Tony) Jones, MD growth, as is evidenced by the great Anthony Senagore, MD interest to implement the enhanced Maxime Cannesson, MD, PhD recovery pathway in hospitals around Terrence Loftus, MD, MBA, FACS the country. Andrew Shaw MB, FRCA, FFICM, FCCM Desiree Chappel, CRNA The ASER Mission is to advance the practice of perioperative enhanced recovery and to contribute to its pathways. -

Total Joint Replacement Hip and Knee Pain Pinnacle Orthopedics Pinnacle Medical Network Total Joint Replacement
Total Joint Replacement Hip and Knee Pain Pinnacle Orthopedics Pinnacle Medical Network Total Joint Replacement About Pinnacle Orthopedics and Pinnacle Medical Network South Louisiana’s Premier System for the Delivery of Musculoskeletal Health Care. Our talented team and professional staff offer a fully- equipped facility for the comprehensive care of your bones, joints, ligaments and muscles. Our team is dedicated to your complete care, from assessment to full recovery. Our primary goal is your safe return to work, sports, play and the activities of daily living. Allow our medical professionals to advance your orthopedic care. Total Joint Replacement “It would be embarrassing to get out of a car because everybody had to help me. Somebody would have to pull me up. I felt like this old woman.” “My life got progressively less active, less fun, and less participative.” “Just a day on my feet was exhausting and the pain became greater and greater until Advil and ibuprofen and all of those kinds of drugs couldn't numb it out. It just got worse and worse.” Total Joint Replacement Does this sound familiar? Total Joint Replacement You’re Not Alone More than 43 million people have some form of arthritis. It is estimated that the number of people affected by arthritis will increase to 60 million by 2020. Source: CDC Total Joint Replacement This information will touch upon the following topics: Understanding the Causes of Joint Pain Treatment Options What Joint Replacement Surgery Involves Realistic Expectations After Joint Replacement Total Joint Replacement Total Joint Replacement Total Joint Replacement Did you know? Nearly 21 million Americans suffer from osteoarthritis, a degenerative joint disease that is a leading cause of joint replacement surgery. -

Patient Guide for a Hip Replacement
Day of surgery: ____________________ Expected discharge home: ____________________ Surgeon: ____________________ Phone number: ____________________ Bring this guide with you to the hospital on the day of your surgery 4100492 (17-10) 2 Introduction This information guide will help you understand what is involved in hip arthroplasty (hip replacement). We hope the information in this booklet will help you prepare for your surgery •••••••••••••••••••••••••••••••••••••••••••••••••••••• About Hôpital Montfort Hôpital Montfort is a Francophone academic health care institution that provides quality care in both official languages and works with its partners to improve the health of communities. Montfort strives for excellence and wants to be a hospital of choice for its personalized patient care, its workplace, teaching and research. Our daily actions are guided by the values of compassion, commitment, excellence and respect. WARNING This guide does not replace the advice of your care provider. Please consult your care provider to assess if the information presented in this guide applies to your situation. The content of this guide was prepared by Vancouver Coastal Health and adapted by Hôpital Montfort. 3 Your Health Care: Be Involved! • Be involved in your health care. Speak up if you have questions or concerns about your care. • Tell a member of your health care team about your past illnesses and your current health condition. • Tell your health team if you have any food or medication allergies. • Make sure you know what to do when you leave the hospital. •••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••• Your Interprofessional Plan of Care • Your hospital admission for your total hip replacement will follow an “interprofessional plan of care” more commonly called a "Clinical Pathway". -

Total Hip Replacement Part 1
DIAGNOSIS AND SURGICAL APPROACHES: TOTAL HIP REPLACEMENT PART 1 Jassin M. Jouria, MD Dr. Jassin M. Jouria is a medical doctor, professor of academic medicine, and medical author. He graduated from Ross University School of Medicine and has completed his clinical clerkship training in various teaching hospitals throughout New York, including King’s County Hospital Center and Brookdale Medical Center, among others. Dr. Jouria has passed all USMLE medical board exams, and has served as a test prep tutor and instructor for Kaplan. He has developed several medical courses and curricula for a variety of educational institutions. Dr. Jouria has also served on multiple levels in the academic field including faculty member and Department Chair. Dr. Jouria continues to serves as a Subject Matter Expert for several continuing education organizations covering multiple basic medical sciences. He has also developed several continuing medical education courses covering various topics in clinical medicine. Recently, Dr. Jouria has been contracted by the University of Miami/Jackson Memorial Hospital’s Department of Surgery to develop an e-module training series for trauma patient management. Dr. Jouria is currently authoring an academic textbook on Human Anatomy & Physiology. Abstract Arthritis, fractures, and repetitive strain can cause significant pain in the hip joint over time, but hip replacement surgery is an option for many patients each year in the United States. Plastic, ceramic, and metal components can be used to wholly replace the ball-and-socket hip joint and restore mobility in patients. Although most patients who undergo total hip replacement surgery are either retired or elderly, it can be useful for any patient who suffers pain that is not relieved by traditional methods. -
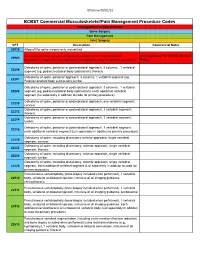
Commercial MSK Procedure Code List Effective 09.01.21.Xlsx
Effective 09/01/21 BCBST Commercial Musculoskeletal/Pain Management Procedure Codes Investigational or Non-Covered Spine Surgery Pain Management Joint Surgery CPT Description Commercial Notes 20930 Allograft for spine surgery only morselized Computer-assisted surgical navigational procedure for musculoskeletal Investigational Per BCBST Medical 20985 procedures, image-less (List separately in addition to code for primary procedure) Policy Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22206 segment (eg, pedicle/vertebral body subtraction); thoracic Osteotomy of spine, posterior approach, 3 columns, 1 vertebral segment (eg. 22207 Pedicle/vertebral body subtraction);lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral 22208 segment (eg, pedicle/vertebral body subtraction); each additional vertebral segment (list separately in addition to code for primary procedure) Osteotomy of spine, posterior or posterolateral approach, one vertebral segment; 22210 cervical Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22212 thoracic Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22214 lumbar Osteotomy of spine, posterior or posterolateral approach, 1 vertebral segment; 22216 each additional vertebral segment (List separately in addition to primary procedure) Osteotomy of spine, including discectomy anterior approach, single vertebral 22220 segment; cervical Osteotomy of spine, including discectomy, anterior approach, single -

Total Hip Arthroplasty in the Horse: Overview, Technical Considerations and Case Report N
EQUINE VETERINARY EDUCATION / AE / November 2010 547 Case Reporteve_118 547..553 Total hip arthroplasty in the horse: Overview, technical considerations and case report N. Huggons*, R. Andrea†, B. Grant‡ and C. Duncan§ WR Pritchard Veterinary Medical Teaching Hospital, University of California Davis; †Chaparral Veterinary Medical Center, Arizona; ‡31624 Wrightwood, California, USA; §Gordon & Leslie Diamond Health Care Centre, Vancouver, Canada. Keywords: horse; total hip arthroplasty; hip replacement; coxofemoral joint; acetabulum Summary Hance 1998; Loesch et al. 2003; Smith et al. 2004), disruption of intra-articular ligaments (Trotter et al. 1986; A total hip arthroplasty was performed in a small Nixon 1994), fractures (Turner et al. 1979; Embertson equine patient with a history of traumatic subluxation of et al. 1986; Hunt et al. 1990a) and dysplasia (Jogi and the coxofemoral joint during infancy resulting in severe Norberg 1962; Speirs and Wrigley 1979) have also been degenerative changes to the femoral head and described. acetabulum. The transtrochanteric surgical approach Few treatment options exist for hip disease, with used to expose the joint, as well as the technique and limitations primarily due to the large muscle mass technology to replace the joint, is described. The patient covering the joint, difficulty with surgical access to the was weightbearing within 24 h of surgery and walking joint and implant failure associated with post operative successfully without sling support 4 days post operatively. weightbearing. Surgical fixation of femoral capital On the fifth post operative day, the patient abruptly epiphyseal fractures in foals has included excision deteriorated and succumbed to multiple pulmonary arthroplasty, Steinmann or Knowles pin fixation, multiple thromboemboli and a jejunal infarction. -

Surgical Considerations of the TMJ
Surgical Considerations of the TMJ Peter B. Franco DMD, FACS Diplomate, American Board of Oral and Maxillofacial Surgery Fellow, American College of Surgeons Carolinas Center for Oral and Facial Surgery Surgical Options of the TMJ • Arthroscopy • Open Arthroplasty – Disk preservation – Diskectomy Surgical Options of TMJ • General Indications – Significant TMJ pain or dysfunction – Non-surgical therapy has failed – Radiographic evidence of disease Failure to manage associated myofascial pain and dysfunction lowers the rate of surgical success. Arthroscopic Arthroplasty • Biopsy of suspected lesions or disease • Confirmation of other diagnostic findings that may warrant surgical treatment • Unexplained persistent joint pain that is non-responsive to medical treatment Arthroscopic Arthroplasty Indications • Closed, locked articular disc • Painful popping joint • Adhesions • Perforated disc • Hypermobile joints • Inflammatory joint disease • Hypermobility • Degenerative Joint Disease • Traumatic Injuries • Suspected Infection Arthroscopic Arthroplasty Equipment • Video/monitoring equipment • Arthroscopic cannula, scissors, forceps, probes, shavers • Laser Arthroscopic Arthroplasty Equipment • Scope • Arthroscopic cannula, scissors, forceps, probes, shavers • Laser Arthroscopic Arthroplasty Equipment • Scope • Video/monitoring equipment • Laser Arthroscopic Arthroplasty Equipment • Scope • Video/monitoring equipment • Arthroscopic cannula, scissors, forceps, probes, shavers Arthroscopic Arthroplasty Equipment Arthroscopic Arthroplasty Arthroscopic -

Indications for Unicompartmental Knee Arthroplasty and Rationale for Robotic Arm–Assisted Technology
A Review Paper Indications for Unicompartmental Knee Arthroplasty and Rationale for Robotic Arm–Assisted Technology Jess H. Lonner, MD results not dissimilar from those of total knee arthroplasty Abstract (TKA), leading to a gradual change in attitude toward UKA. Unicompartmental knee arthroplasty (UKA) is an effec- As long-term data become available, UKA is being more tive surgical treatment for focal arthritis when appropri- universally embraced as a clear and definable treatment ate selection criteria are followed. Although results can option for unicompartmental arthritis. be optimized with careful patient selection and use of a Superb clinical data and desirable kinematic perfor- sound implant design, two of the most important deter- mance support the role of UKA. Berger and colleagues3 minants of UKA performance and durability are how well the bone is prepared and components aligned. Study found that the implant survival rate for 62 consecutive results have shown that component malalignment by as UKAs performed by a skilled surgeon with a design still in little as 2° may predispose to implant failure after UKA. use today was 98% after 10 years and 96% after 13 years, Conventional cutting guides have been relatively inac- using revision and radiographic loosening as the respective curate in determining alignment and preparing the bone endpoints. Emerson and Higgins,4 reporting their personal surfaces for unicompartmental implants. Computer navi- experience with 55 mobile-bearing UKAs, noted a 90% gation has improved component alignment to an extent, rate of 10-year implant survival with progression of lateral but outliers still exist. compartment arthritis as the endpoint and 96% with com- The introduction of robotics capitalizes on the virtues of ponent loosening as the endpoint. -

Hip Impingement and Osteoarthritis. Hip Arthroscopy, Resurfacing, Or Replacement: Is It Time for Surgery?
Hip Impingement and Osteoarthritis. Hip Arthroscopy, Resurfacing, or Replacement: Is it Time for Surgery? Bryan Whitfield, MD [email protected] Hip Operations • Background of hip diagnoses • Treatment of hip pathology • Surgery candidates • Time for surgery? • Cases Intra-articular hip pain - diagnoses • FAI (femoroacetabular impingement) / acetabular labrum tear • Neck of the femur and rim of the socket run into each other • Tear the labrum. • Articular cartilage damage possible • Labrum: fluid management, stability, and seal of the joint • Osteoarthritis • Socket and ball both coated in a layer of cartilage • Arthritis is the wearing away, loss of or damage to the cartilage coating (articular cartilage) Intra-articular hip pain - diagnoses • FAI (femoroacetabular impingement) / acetabular labrum tear • Neck of the femur and rim of the socket run into each other • Tear the labrum. • Articular cartilage damage possible • Labrum: fluid management, stability, and seal of the joint • Osteoarthritis • Socket and ball both coated in a layer of cartilage • Arthritis is the wearing away, loss of or damage to the cartilage coating (articular cartilage) Intra-articular hip pain - diagnoses • FAI (femoroacetabular impingement) / acetabular labrum tear • Neck of the femur and rim of the socket run into each other • Tear the labrum. • Articular cartilage damage possible • Labrum: fluid management, stability, and seal of the joint • Osteoarthritis • Socket and ball both coated in a layer of cartilage • Arthritis is the wearing away, loss -

A Regional Resource for Joint Replacement, Trauma, Orthopedics, Sports Medicine and Spine Problems
3688 Veterans Memorial Dr. Hattiesburg, MS 39401 appointments, referrals & 2nd opinions: 601-554-7400 Online encyclopedia about orthopedics and spine care at: SouthernBoneandJoint.com A regional resource for joint replacement, trauma, orthopedics, sports medicine and spine problems Decades ago an orthopedic provide patients the most hip and knee replacement. The advanced FDA-approved artificial surgeon would treat all types advanced technology and care technology enables the joint discs that preserve motion in the of joint problems. With ever- specific to their orthopedic injury replacement surgeon to map out spine. increasing new technology and or pain symptom. in advance of surgery the optimal Consquently, these clinical care treatment advances specific to One example is the use of new cuts in the bone for the best centers are referred patients from different joints and bones, that’s Robotic Surgery Technology. The surgical outcome and to spare as across the region. changed dramatically. Over hip and knee surgeons make use much bone as possible. Appointments, referrals and the past 15 years, orthopedics of Mako Robotic Surgery that Similarly, the spine surgeons in second opinions can be set up by has become super-specialized improves the outcomes from The Spine Center provide the most calling 601-554-7400. with surgeons now becoming fellowship-trained in a specific body part, such as foot/ankle or ORTHOPEDIC SPECIALTY CENTERS LOCATIONS hand/arm or spine. The best care comes from a specialized approach. Consequently, MAIN CLINIC LOCATION: Because of this super 3688 Veterans Memorial Drive Southern Bone and Joint Specialists is organized into CLINICAL CARE specialization in orthopedics, Hattiesburg, MS 39401 CENTERS that provides the most advanced treatment options. -

AIS-Pennhip-Manual.Pdf
Training Manual Table of Contents Chapter 1: Introduction and Overview ............................................................................................... 5 Brief History of PennHIP ........................................................................................................................................5 Current Status of CHD ...........................................................................................................................................5 Requirements for Improved Hip Screening ............................................................................................................6 PennHIP Strategies ................................................................................................................................................7 The AIS PennHIP Procedure .................................................................................................................................8 AIS PennHIP Certification ......................................................................................................................................8 Purchasing a Distractor ..........................................................................................................................................9 Antech Imaging Services........................................................................................................................................9 Summary ............................................................................................................................................................ -

Utilization Management Policy Title: Lumbar Spine Surgeries
Medica Policy No. III-SUR.34 UTILIZATION MANAGEMENT POLICY TITLE: LUMBAR SPINE SURGERIES EFFECTIVE DATE: January 18, 2021 This policy was developed with input from specialists in orthopedic spine surgery and endorsed by the Medical Policy Committee. IMPORTANT INFORMATION – PLEASE READ BEFORE USING THIS POLICY These services may or may not be covered by all Medica plans. Please refer to the member’s plan document for specific coverage information. If there is a difference between this general information and the member’s plan document, the member’s plan document will be used to determine coverage. With respect to Medicare and Minnesota Health Care Programs, this policy will apply unless these programs require different coverage. Members may contact Medica Customer Service at the phone number listed on their member identification card to discuss their benefits more specifically. Providers with questions about this Medica utilization management policy may call the Medica Provider Service Center toll-free at 1-800-458-5512. Medica utilization management policies are not medical advice. Members should consult with appropriate health care providers to obtain needed medical advice, care and treatment. PURPOSE To promote consistency between Utilization Management reviewers by providing the criteria that determine medical necessity. BACKGROUND I. Prevalence / Incidence A. It is reported that the lifetime incidence of low back pain (LBP) in the general population within the United States is between 60% and 90%, with an annual incidence of 5%. According to a National Center for Health Statistics study (Patel, 2007), 14.3% of new patient visits to primary care physicians per year are for LBP.