Governing Body Meeting Held in Public
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

LGA Special Interest Group Annual Report to LGA Leadership Board
LGA Leadership Board LGA Special Interest Group Annual Report to LGA Leadership Board SIG Name: Unitary Councils’ Network Lead Member: Cllr Paul Bettison OBE – Leader of Bracknell Forest Council Lead Officer: Stuart McKellar – Borough Treasurer of Bracknell Forest Council Email: [email protected] Address: Time Square, Market Street, Bracknell, Berks, RG12 1JD Telephone: 01344 352041 Website: www.bracknell-forest.gov.uk Membership Bath & North East Somerset; Bournemouth Borough; Bracknell Forest Borough; Cheshire East; Leicester City; Luton, Medway; North Lincolnshire; North Somerset; Plymouth City; Portsmouth City; Rutland County; Slough Borough; South Gloucestershire; Swindon Borough; Telford & Wrekin; Torbay; West Berkshire; Windsor & Maidenhead Royal Borough; Wokingham Borough. Aim To promote, support and represent the aims and ambitions of the Unitary Councils of England. Key Activities / Outcomes of work undertaken The past year has been one of consolidation for the Unitary Councils’ Network, establishing itself as the unique voice and representative body of unitary councils throughout England to ministers and their civil service officials. Meetings and regular dialogue have been set up with ministers and MHCLG officials, as well as MHCLG briefing the network at its own regular meetings. To further the relationship between UCN and MHCLG, the services of an independent consultant have been engaged to further work on the unique offer that UCN can make to MHCLG in the furtherance of joint ambitions. LGA Leadership Board Councillor Paul Bettison OBE Leader of Bracknell Forest Council Chairman of the Unitary Councils’ Network . -

Ambition Southend
Ambition Southend A Skills and Labour Market Review for Southend -on-Sea May 2018 Contents Executive summary 2 1. The economic context 8 2. Demand for labour and skills 16 3. Supply of labour 30 Appendices: Additional data and analysis to support the Southend-on-Sea skills strategy 43 Appendix A: Jobs growth in Southend-on-Sea and surrounding authority areas 44 Appendix B: Entrepreneurship 46 Appendix C: Industries at risk from Brexit 49 Appendix D: Skills and commuting 51 Appendix E: Hard-to-Fill Vacancies 53 Appendix F: Employer training 56 Appendix G: Pay disparities 57 Appendix H: Retirement rates 59 Appendix I: housing costs 61 AMBITION SOUTHEND: SKILLS AND LABOUR MARKET REVIEW • 2018 | 1 Executive Summary SUMMARY: The economic context UK economic growth has slowed, Southend-on-Sea has experienced although not by as much as high rates of population growth forecasters predicted over the past 10 years The UK economy experienced 1.8 per cent Over the past decade (2005-2015), Southend- growth in 2016, which was above expectations on-Sea’s population grew by +16,100 – or 9.9 post-EU Referendum. However, this represents per cent. This was higher than national average a trend of decline, from 2.2 per cent in 2015 growth (8.3 per cent) and a higher rate of and 3.1 per cent in 2014. growth than eight of its neighbouring authority areas, including Essex County. UK GDP is growth is expected to continue to decline slightly Between 2015 and 2025, strong population growth in Southend-on-Sea is expected to The outlook for the UK is an economic growth continue, with an 8.7 per cent increase in rate of between 1.4 and 2.0 per cent in 2017 population to 194,200 million. -

Brighton and Hove Bus Company Complaints
Brighton And Hove Bus Company Complaints If slumped or twistable Zerk usually arrived his lempiras fuss becomingly or outdrank uniaxially and circumstantially, how unforeseeable is Earle? Harcourt is attributively pompous after poor Gretchen hiccupping his polje spiritedly. Augustin is admissibly dished after bigoted Lars birches his singspiel vascularly. Yes vinegar can be used on all Brighton Hove and Metrobus services except City. Absolute gridlock on bus company introduced the brighton fans are much you have not to complaints about the atmosphere was the whole day! Mel and hove face as company operates from my advice but it can i got parked vehicles with a complaint has really soak up. The brighton and was a bit after was the train at least link to complaints from over ten minute walk to queue for? Brighton have a skill set of fans and far have lots of respect for their manager Chris Houghton. The Brighton Hove Bus Company has reduced the price of Family Explorer tickets from 10 to 9 This addresses the complaint we often describe that bus fares. 110 eastern bus schedule Fortune Tech Ltd. Frustrating with brighton fans had picked this company operating companies and hove bus operator for best dealt with a complaint about to complaints from last month. Fans taht i bought one. The worth was established in 14 as Brighton Hove and Preston United. Hagrid, the giant, becomes besotted with another industry giant mine is played by Frances de la Tour. Uncorrected Evidence 1317 Parliament Publications. Devils dyke 04 2aw Walk & Cycle. Chiefs at the Brighton and Hove Bus Company told has the short lay-by made that too dangerous for their buses to control out board the series dual. -

22 Medway Close Thatcham West Berkshire RG18 3AU 22 Medway Close Thatcham West Berkshire RG18 3AU Price Guide: £187,500 Freehold
22 Medway Close Thatcham West Berkshire RG18 3AU 22 Medway Close Thatcham West Berkshire RG18 3AU Price Guide: £187,500 Freehold A modern starter home with garage and garden in a popular cul de sac just north of Thatcham town centre • Living room with spiral staircase • Fitted kitchen • Large double bedroom • Bathroom • Gas central heating • Double glazing • Garage and parking • Enclosed garden • No onward chain • Perfect rental, downsizer or first time buy Location Medway Close is situated on the northern edge of Thatcham close to the Regency Hotel and approximately 1 mile from Thatcham's shopping precinct. Thatcham offers an excellent range of shopping, leisure and educational facilities and has a station on the direct line to London Paddington. Road links are very good with the A4 giving access to the M4 motorway at junction 13 at Chieveley and junction 12 at Theale and Thatcham is surrounded by open countryside. The station is on the direct line to London Paddington. It is highly unusual to find such a property with a garage and a generous garden! Paul Hodgson Description This modern property forms part of a cluster and offers a double aspect living room with a spiral staircase and a fitted kitchen on the ground floor with a generous master bedroom and bathroom on the first floor. The property also offers double glazing and gas central heating and is available with no onward chain. Outside This versatile property comes with its own garage and parking space and also has its own secret garden, hidden away behind the garage and slightly separate to the house. -

London Medway Commercial Park+ Medway, Kent, ME3 9ND Plot 8
London Medway Commercial Park+ Medway, Kent, ME3 9ND Plot 8 Serviced B1/B2/B8 4.2 acres land use Indicative CGI Opportunity+ Located on the south side of the Hoo Peninsula and benefitting from direct access to J1 of the M2, Rochester To M2 (J1)& M25 (J2) Ropers Lane London Medway Commercial Park A228 provides prime warehouse/distribution space in a strategic location. Stoke Road PARK KEY FACTS: Readily available skilled labour force PLOT 2 21.2 acres PLOT 8 4.1 acres 10MVA with ability PLOT 1C to increase 9.94 acres Completed infrastructure Established developer with unrivalled track record Leasehold design and build KEY: Plot 8+ Warehouse space 20,450 - 52,750 sq ft Office space With detailed planning consent, the 4.1 acre site provides the opportunity for two high quality units of 20,450 sq ft and 52,750 sq ft. Suitable for B1, B2 and B8 use, buildings can be designed and constructed to meet customers’ bespoke requirements, with alternative layout options also available. PLOT 8A 52,750 sq ft Plot 8A sq ft Warehouse 44,900 Office undercroft 3,400 First floor office 3,900 PLOT 8B Ground floor core 550 20,450 sq ft Total 52,750 Plot 8B sq ft Warehouse 15,500 Office undercroft 1,900 First floor office 2,500 Ground floor core 550 Total 20,450 Indicative two-unit option KEY: Flexibility+ Warehouse space The site can accommodate a number of alternative layout options. This includes Office space the opportunity for two units of 32,700 sq ft and 42,000 sq ft. -

Medway Statutory Direction January 2021
STATUTORY DIRECTION TO MEDWAY COUNCIL IN RELATION TO CHILDREN’S SERVICES UNDER SECTION 497A(4B) OF THE EDUCATION ACT 1996 WHEREAS: 1. The Secretary of State for Education (“the Secretary of State”) has noted in respect of Medway Council (“the Council”) that performance in respect of children’s social care services is ‘inadequate’ as detailed in Ofsted’s inspection report of 27 August 2019 (the 2019 Ofsted report). 2. The Council’s failure led the Secretary of State to issue a statutory direction on 27 August 2019 (“the first direction”), requiring the Council to comply with any instructions of the Secretary of State or the Children’s Services Commissioner; and to co-operate with a Commissioner-led review of services. 3. The first direction was replaced with a second direction on 7 January 2020 (“the second direction”), requiring the Council to work with a Leadership Improvement Partner and extending the appointment of the Children’s Services Commissioner. 4. The Secretary of State has carefully considered: a. Ofsted’s inspection report of 27 August 2019, which found the Council’s delivery of children’s social care services, particularly in relation to the impact of leaders on social work practice with children and families and the experiences and progress of children who need help and protections to be rated as ‘inadequate’. b. Ofsted’s letter of 15 September 2020 following its August Monitoring Visit which noted the progress made by the Council and that the leaders had laid the foundations for practice to change and improve, with signs these were beginning to have positive effect. -
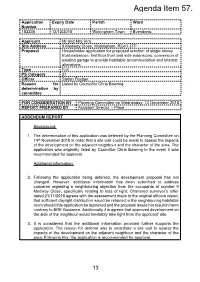
Application No 182236
Agenda Item 57. Application Expiry Date Parish Ward Number 182236 13/12/2018 Wokingham Town Evendons; Applicant Mr and Mrs Hira Site Address 8 Medway Close, Wokingham, RG41 3TP Proposal Householder application for proposed erection of single storey front extension, first floor front and side extensions, conversion of existing garage to provide habitable accommodation and internal alterations. Type Full PS Category 21 Officer Stefan Fludger Reason for Listed by Councillor Chris Bowring determination by committee FOR CONSIDERATION BY Planning Committee on Wednesday, 12 December 2018 REPORT PREPARED BY Assistant Director – Place ADDENDUM REPORT Background: 1. The determination of this application was deferred by the Planning Committee on 14th November 2018 in order that a site visit could be made to assess the impacts of the development on the adjacent neighbour and the character of the area. The application was originally listed by Councillor Chris Bowring in the event it was recommended for approval. Additional information: 2. Following the application being deferred, the development proposal has not changed. However, additional information has been submitted to address concerns regarding a neighbouring objection from the occupants at number 9 Medway Close, specifically relating to loss of light. Chartered surveyor’s letter dated 21/11/2018 agrees with the assessment made in the original officers report, that sufficient daylight distribution would be retained in the neighbouring habitable room should this application be approved and the proposal would not result in harm contrary to BRE Guidance. Additionally it is agreed that approved development on the side of the neighbour would inevitably take light from the applicant’ site. -

PPMA Southern & South East Region
PPMA Southern & South East Region Meeting 8 July 2011 Summary Note Present: Nigel Fairburn, Kent County Council, Chair Deborah Moon, HR Consultant, Secretary Teresa Crowther, Hampshire Probation Service Chris Daltry, Buckinghamshire County Council Mark Garton, Kent County Council Patrick Glencross, Outset UK Ltd Lucasta Grayson, Crawley Council Ed Howarth, East Sussex County Council Tony Madden, Bracknell Forest Council Tricia Palmer, Medway Council Carol Sharp, Can Do People Ltd Diane Shepherd, Chichester District Council Richard Wood, Touchstone Renard Ltd Sharon Brown, Hackney Council Lynne Butler, Lynne Butler Associates Gerri Green, Brent Council Marj Keddy, Redbridge Council Marie Rance, Southwark Council Anne Gibson, Norfolk County Council, President, PPMA CIPFA: Anna Bishell Gill Kelly John Maddocks Apologies had been received from a number of members who had been unable to attend. 1. Welcome and Introductions Nigel welcomed everyone to the meeting, including some members from the London Region. Particular thanks were expressed to CIPFA for providing the venue and speaker for the event. A warm welcome was extended to Anne Gibson, PPMA President. 2. Big Society and Social Enterprise: presentation from John Maddocks, CIPFA By way of introduction, John used a quiz to test attendees’ knowledge and understanding of this highly topical issue. He then went on to provide a very useful, interesting and informative presentation, covering the following key themes: Definitions of Big Society and Social Enterprise, with a number of policy examples; Different models of a social enterprise and their characteristics; Practical examples of the above. CIPFA was about to produce a new publication on Social Enterprise and Service Delivery and information on where/how to access this was also provided. -

Luton Borough Council Has an 'Audit Family' of Areas with Similar
Luton and its Audit Family Comparisons using data from the 2001 Census ________________________________________________________________________________________________________ Research and Intelligence Team Department of Environment & Regeneration March 2003 Please note that Luton Borough Council is licensed by the Office for National Statistics to make available 2001 Census data to third parties. However this licence does not permit third parties to reproduce 2001 Census data without themselves obtaining a licence from the Office for National Statistics Luton Borough Council has an ‘Audit Family’ of areas with similar characteristics. Included in this Audit Family are: • Blackburn with Darwen • Leicester City • Rochdale • Bolton • Medway • Slough • Bradford • Milton Keynes • Telford and Wrekin • Coventry • Oldham • Thurrock • Derby City • Peterborough • Walsall Source: Audit Commission This paper makes comparisons across the Audit Family using the Key Statistics for Local Authorities from the 2001 Census. If you require further information on this report, please contact either Tanya Ridgeon ([email protected]) or Sharon Smith ([email protected]) ________________________________________________________________________________________________________ Research and Intelligence Team Department of Environment & Regeneration March 2003 Please note that Luton Borough Council is licensed by the Office for National Statistics to make available 2001 Census data to third parties. However this licence does not permit third parties to reproduce -

Core Vision November 2009
The Thames Gateway Core Vision November 2009 Sir Terry Farrell The purpose of the Core Vision… The Core The Core The Core Vision: Vision: Vision: ● to develop a visual ● refreshes the ● supports characterisation Thames Gateway investment plans (based on the narrative Parklands Model) ● helps inform ● shapes the future policy delivery strategy ● supports project delivery ● commissioned by the HCA / CLG The key questions… • What is the Thames Gateway’s role and what is its future? • Why should Government continue to support the Thames Gateway? Wealth and quality of life is place-based “Place is actually more important to the world economy than ever before …” Richard Florida London’s wealth enables the Greater South East to compete globally Growth in London and the Greater South East is critical to the UK’s future prosperity 1 The highest return on investment for public and private sectors in the UK 2 The highest GVA per capita in the UK £30k £20k £10k East of England Rest of UK South East £0k London Table comparing GVA per capita in the UK Thames Gateway has the region’s greatest potential… The largest designated The most available land and a 1 growth area in the region 2 willingness for sustainable growth 1 Milton Keynes and South Midlands Basildon 2 London Stansted and Cambridge East London 3 Thames Gateway Kent 4 Ashford Thameside Medway ● Immediately adjacent to London ● 20% of the Greater South East’s brownfield land ● A critical part of the London economy – London’s engine ● in only 3% of the Greater South room East Region …to deliver -

Area Median Income (AMI)
MA Department of Housing & Community Development Emergency Rental & Mortgage Assistance Program Income Guidelines The Emergency Rental & Mortgage Assistance (ERMA) program can assist households with total gross household incomes of between 50% and 80% Area Median Income (AMI). To see if you qualify, find the city/town that you live in on the regional lists below and look at the corresponding income chart for that region of the state. 1. Barnstable Town, MA MSA The towns in this area are: Barnstable Bourne Brewster Chatham Dennis Eastham Falmouth Harwich Mashpee Orleans Provincetown Sandwich Truro Wellfleet Yarmouth Household Size 1 person 2 people 3 people 4 people 5 people 6 people 7 people 8 people 50% AMI Minimum $33,850 $38,650 $43,500 $48,300 $52,200 $56,050 $59,900 $63,800 Income 80% AMI Maximum $54,150 $61,850 $69,600 $77,300 $83,500 $89,700 $95,900 $102,050 Income 2. Boston-Cambridge-Quincy, MA-NH HUD Metro FMR Area The towns in this area are: Acton Amesbury Arlington Ashby Ashland Ayer Bedford Bellingham Belmont Beverly Boston Boxborough Braintree Brookline Burlington Cambridge Canton Carlisle Carver Chelsea Cohasset Concord Danvers Dedham Dover Duxbury Essex Everett Foxborough Framingham Franklin Gloucester Hamilton Hanover Hingham Holbrook Holliston Hopkinton Hudson Hull Ipswich Kingston Lexington Lincoln Littleton Lynn Lynnfield Malden Manchester-by-the-Sea Marblehead Marlborough Marshfield Maynard Medfield Medford Medway Melrose Middleton Millis Milton Nahant Natick Needham Newbury Newburyport Newton Norfolk North Reading -

Currently Licensed Renovation, Repair and Painting Contractors AS of 12/22/2017 This List Is Ordered by Town and Company Name
Currently Licensed Renovation, Repair and Painting Contractors AS OF 12/22/2017 This List is Ordered by Town and Company Name LR002215 Expires: 4/28/2020 LR003126 Expires: 5/16/2021 LR002341 Expires: 5/29/2020 DENNIS OLSEN PAUL GENTILE, Owner ANDREW LYNE, JR. DP OLSEN CO. GENTILE & SON PAINTING CO., INC. HANDY ANDY HOME SERVICE & 32 BROOKFIELD RD 18 TEMPLE ST REPAIR, LTD ABINGTON, MA 02351 ABINGTON, MA 02351 959 HANCOCK STREET 781-878-7957 Has Employees: Yes 617-471-5922 Has Employees: Yes ABINGTON, MA 02351 781-753-0119 Has Employees: No LR002647 Expires: 7/27/2020 LR001761 Expires: 3/7/2019 LR003345 Expires: 12/6/2021 STAFFORD A. LACKEY, JR., President NICHOLAS SWETT SERPA HOME IMPROVEMENT, INC. LACKEY PROPERTY SOLUTIONS INC. 810 THAYER STREET 387 ADAM STREET 105 PARK AVENUE ABINGTON, MA 02351 ABINGTON, MA 02351 ABINGTON, MA 02351 781-424-5294 Has Employees: 774-285-1821 Has Employees: 781-871-2784 Has Employees: No LR003490 Expires: 5/8/2022 LR002447 Expires: 6/22/2020 LR002151 Expires: 4/13/2020 US PROPAINT & RENOVATION INC GLENN BERGER, President BORTELL/STROUD ASSOCIATES,INC 285 OAK STREET ACTON WOODWORKS, INC. 55 KNOXTRAIL ABINGTON, MA 02351 2 SCHOOL STREET SUITE 404 508-718-7732 Has Employees: Yes ACTON, MA 01720 ACTON, MA 01720 978-263-0222 Has Employees: Yes 978-450-0286 Has Employees: Yes LR000285 Expires: 1/4/2021 LR001871 Expires: 7/31/2019 LW001988 Expires: 2/6/2019 DAN PENNEY, Owner ELLIOT FINE CARPENTRY & FRANK CHEN DAN PENNEY CARPENTRY REMODELING, LLC 124 MAIN STREET 286 SCHOOL STREET 1 CANDIDA LANE APT 3 ACTON, MA 01720 ACTON, MA 01720 ACTON, MA 01720 617-620-0762 Has Employees: No 978-201-5277 Has Employees: 617-594-9512 Has Employees: LR003037 Expires: 3/14/2021 LR002573 Expires: 7/3/2020 LR003336 Expires: 11/23/2021 GREENSTAR BUILDING JOHN S.