Cost–Utility Analysis of Glucagon-Like Peptide-1 Agonists
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Soliqua – Criteria
Criteria Based Consultation Prescribing Program CRITERIA FOR DRUG COVERAGE Insulin glargine; lixisenatide (Soliqua) subcutaneous injection Initiation (new start) criteria: Non-formulary lixisenatide/glargine (Soliqua) will be covered on the prescription drug benefit when the following criteria are met: Must meet criteria for both individual agents lixisenatide and insulin glargine. Criteria for lixisenatide: • Diagnosis of Type 2 Diabetes Mellitus • Intolerance to preferred GLP-1 agonists liraglutide (Victoza) AND injectable semaglutide (Ozempic) • No personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) • No personal history of gastroparesis • On maximally tolerated metformin dose (dose appropriate per renal function) or allergy or intolerance* to metformin (includes both metformin IR and XR) • And meets one of the following criteria: o Inadequate glycemic response on both basal and bolus insulin despite high dose requirements (total daily insulin dose of 1.5 units per kilogram of body weight or more OR greater than 200 units) OR o Has experienced recurrent nocturnal hypoglycemia with basal insulin defined as: 3 or more episodes of nocturnal hypoglycemia (BG less than 70 mg/dL) over the preceding 30 days that persists despite basal insulin dose reduction (including decrease in NPH dose and subsequent switch to and dose adjustment of insulin glargine) Criteria for insulin glargine • Use in patients with type 1 diabetes mellitus as basal insulin -OR- • Use in patients with -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal. -
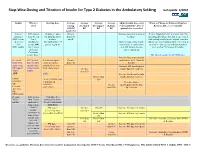
Step-Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting Last Update 5/2010
Step -Wise Dosing and Titration of Insulin for Type 2 Diabetes in the Ambulatory Setting last update 5/2010 Insulin When to Starting dose Average Average Average Average Adjust Insulin dose every When to Change to Different Regimen start fasting Pre-lunch Pre-supper Bedtime 3 days until BG < 130, or Recheck A1C every 3 months AM BG BG BG BG optimal dose is reached Goal<130 Lantus A1C greater 10 units or up to Greater Increase dose by 2-4 units at If after 3 months if A1c is greater than 7% (glargine) than 8% on 0.2 units/kg SQ at than 130 bedtime. and optimal bedtime dose has been reached OR Levemir 2 or 3 bedtime mg/dL with fasting blood glucose at goal, consider (detemir) antidiabetic (DC sulfonylurea if Optimal long acting (basal) adding a pre-meal bolus insulin at the largest OR agents OR part of regimen) insulin dose keeps bedtime meal of the day, pre-meal bolus insulin at NPH insulin 1 or 2 agents and AM fasting glucose each meal or 70/30 premix insulin. if Serum values consistent. Creatinine greater than 2 DC all oral agents except Metformin. Increase long acting (basal) Pre-meal A1C greater 2-4 units of rapid Greater insulin dose by 2-4 units at bolus with than 7% with acting or regular than 130 bedtime rapid acting optimal long insulin SQ at each Increase AM rapid/regular OR regular acting (basal) meal (base dose) Greater insulin dose by 2-4 units. insulin insulin. than 130 AND with Increase lunch rapid/regular Greater than insulin dose by 2-4 units. -

Combination Use of Insulin and Incretins in Type 2 Diabetes
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé CADTH Optimal Use Report Volume 3, Issue 1C Combination Use of Insulin and July 2013 Incretins in Type 2 Diabetes Supporting Informed Decisions This report is prepared by the Canadian Agency for Drugs and Technologies in Health (CADTH). The report contains a comprehensive review of the existing public literature, studies, materials, and other information and documentation (collectively the “source documentation”) available to CADTH at the time of report preparation. The information in this report is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. The information in this report should not be used as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process, nor is it intended to replace professional medical advice. While CADTH has taken care in the preparation of this document to ensure that its contents are accurate, complete, and up to date as of the date of publication, CADTH does not make any guarantee to that effect. CADTH is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in the source documentation. CADTH is not responsible for any errors or omissions or injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the information in this document or in any of the source documentation. -

Tresiba-Product-Monograph.Pdf
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION TRESIBA® insulin degludec injection TRESIBA® FlexTouch® 100 U/mL, Solution for injection in a pre-filled pen TRESIBA® FlexTouch® 200 U/mL, Solution for injection in a pre-filled pen Subcutaneous Antidiabetic Agent Long-Acting Basal Insulin Analogue ATC Code: A10AE06 Novo Nordisk Canada Inc. Date of Initial Authorization: AUG 25, 2017 101-2476 Argentia Road Date of Revision: Mississauga, Ontario JUL 23, 2021 Canada L5N 6M1 Submission Control Number: 250276 Product Monograph Master Template Template Date: September 2020 TRESIBA® (insulin degludec injection) Page 1 of 2 RECENT MAJOR LABEL CHANGES 7 Warnings and Precautions 03/2021 TABLE OF CONTENTS Sections or subsections that are not applicable at the time of authorization are not listed. TABLE OF CONTENTS ..............................................................................................................2 1 INDICATIONS ..................................................................................................................4 1.1 Pediatrics ................................................................................................................4 1.2 Geriatrics ................................................................................................................4 2 CONTRAINDICATIONS ..................................................................................................4 3 SERIOUS WARNINGS AND PRECAUTIONS BOX .......................................................4 4 DOSAGE AND ADMINISTRATION -

Study Protocol
CLINICAL TRIAL REPORT ZP4207-17086 (ZEA-DNK-02170) 16.1 TRIAL INFORMATION 16.1.1 PROTOCOL AND PROTOCOL AMENDMENTS This appendix includes Document Date, Version Clinical trial protocol Version 1.0, 08 June 2018 (valid in Slovenia and the USA) Version 3.0, 08 January 2019 (valid in Germany) Section 16.1.1: Protocol and Protocol Amendments Clinical Trial Protocol, final version 1.0 ZP4207-17086 (ZEA-DNK-02170) Clinical Trial Protocol A phase 3, randomized, double-blind, placebo- and active-controlled, parallel-arm trial to assess the efficacy, safety, and pharmacokinetics of dasiglucagon relative to placebo and GlucaGen® when administered as a rescue therapy for severe hypoglycemia in children with T1DM treated with insulin Sponsor code: ZP4207-17086 Synteract: ZEA-DNK-02170 EudraCT number: 2018-000892-33 Coordinating investigator: Prof. Dr. med. Thomas Danne Allgemeine Kinderheilkunde Diabetologie, Endokrinologie, Klinische Forschung Diabeteszentrum für Kinder und Jugendliche AUF DER BULT Kinder- und Jugendkrankenhaus Janusz-Korczak-Allee 12 30173 Hannover Germany Sponsor: Zealand Pharma A/S Smedeland 36 2600 Glostrup, Copenhagen Denmark Version: final version 1.0 Date: 08 June 2018 GCP statement This trial will be performed in compliance with Good Clinical Practice, the Declaration of Helsinki (with amendments) and local legal and regulatory requirements. 08 June 2018 CONFIDENTIAL Page 1/55 Zealand Pharma A/S ClinicalTrial Prolocol, final ve¡sion 1.0 zP 42A7 -1 7 A 86 (ZEA-DN K-02 1 L Slgnature¡ and agreoment wlth protocot Tltle: phase A 3, ¡andomized, double-blind, placebo- and aclivg-controlled, parallel-arm trial to assess the efficac¡ safety, and pharmacoítinetics of dasiglucagon rela¡ve to placebo and GlucaGeno when edministered as a rescue thêrapy for sevãre triposivcemia ¡n children w¡th TlDM treated with insulin we, the undersigned, agroe to conduct lhls trlal according to lhe Trlal protocol. -
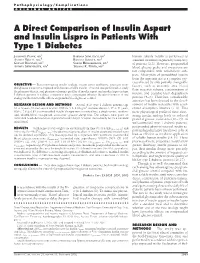
A Direct Comparison of Insulin Aspart and Insulin Lispro in Patients with Type 1 Diabetes
Pathophysiology/Complications ORIGINAL ARTICLE A Direct Comparison of Insulin Aspart and Insulin Lispro in Patients With Type 1 Diabetes 1 1 JOHANNES PLANK, MD BARBARA SEMLITSCH, RN human soluble insulin is performed as 1 1 ANDREA WUTTE, MSC ROMANA SOMMER, MD standard treatment regimen by a majority 1 2 GERNOT BRUNNER, MD SABINE HIRSCHBERGER, MD 1 1 of patients (2,3). However, postprandial ANDREA SIEBENHOFER, MD THOMAS R. PIEBER, MD blood glucose peaks and excursions are not comparable with nondiabetic sub- jects. Absorption of unmodified insulin from the injection site is a complex pro- cess affected by only partially changeable OBJECTIVE — Both rapid-acting insulin analogs, insulin aspart and lispro, attenuate pran- factors, such as anatomic area, blood dial glucose excursion compared with human soluble insulin. This trial was performed to study flow, injection volume, concentration of the pharmacokinetic and pharmacodynamic profiles of insulin aspart and insulin lispro in type 1 diabetic patients in a direct comparison and to investigate whether the administration of one insulin, and possible local degradation analog results in favorable effects on prandial blood glucose control. process (4–6). Therefore, considerable attention has been devoted to the devel- RESEARCH DESIGN AND METHODS — A total of 24 type 1 diabetic patients (age opment of insulin molecules with accel- 36 Ϯ 8 years, 16 men and 8 women, BMI 24.3 Ϯ 2.6 kg/m2, diabetes duration 17 Ϯ 11 years, erated absorption kinetics (7–9). This Ϯ HbA1c 7.9 0.8%) on intensified insulin therapy were recruited into a single-center, random- more physiological profile of these short- ized, double-blind, two-period, cross-over, glucose clamp trial. -

Safety and Effectiveness of Dipeptidyl Peptidase-4 Inhibitors Versus Intermediate-Acting Insulin Or Placebo for Patients with Ty
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2014-005752 on 23 December 2014. Downloaded from Safety and effectiveness of dipeptidyl peptidase-4 inhibitors versus intermediate-acting insulin or placebo for patients with type 2 diabetes failing two oral antihyperglycaemic agents: a systematic review and network meta-analysis Andrea C Tricco,1 Jesmin Antony,1 Paul A Khan,1 Marco Ghassemi,1 Jemila S Hamid,2 Huda Ashoor,1 Erik Blondal,1 Charlene Soobiah,1 Catherine H Yu,1 Brian Hutton,3 Brenda R Hemmelgarn,4 David Moher,3 Sumit R Majumdar,5 Sharon E Straus1,6 To cite: Tricco AC, Antony J, ABSTRACT et al Strengths and limitations of this study Khan PA, . Safety and Objective: To evaluate the effectiveness and safety of effectiveness of dipeptidyl dipeptidyl peptidase-4 (DPP-4) inhibitors versus ▪ peptidase-4 inhibitors versus Comprehensive systematic review including 10 intermediate-acting insulin for adults with type 2 intermediate-acting insulin or trials with a total of 2967 adult patients with placebo for patients with type diabetes mellitus (T2DM) and poor glycaemic control type 2 diabetes mellitus. 2 diabetes failing two oral despite treatment with two oral agents. ▪ Used rigorous methods for the conduct of our antihyperglycaemic agents: Setting: Studies were multicentre and multinational. systematic review (eg, we assessed risk of bias a systematic review and Participants: Ten studies including 2967 patients using the Cochrane risk-of-bias tool, conducted network meta-analysis. BMJ with T2DM. an assessment of the quality of reporting of Open 2014;4:e005752. Interventions: Studies that examined DPP-4 inhibitors harms using the McHarm tool, registered our http://bmjopen.bmj.com/ doi:10.1136/bmjopen-2014- compared with each other, intermediate-acting insulin, systematic review with the PROSPERO registry 005752 no treatment or placebo in patients with T2DM. -

Drug Formulary This Drug Formulary Was Updated: July 1, 2021
Kaiser Permanente Insurance Company (KPIC) PPO and Out-of-Area Indemnity (OOA) Drug Formulary This Drug Formulary was updated: July 1, 2021 NOTE: This drug formulary is updated often and is subject to change. Upon revision, all previous versions of the drug formulary are no longer in effect. This document contains information regarding the drugs that are covered when you participate in the California Grandfathered PPO and Out-of- Area Indemnity (OOA) Health Insurance Plans for Large Groups offered by Kaiser Permanente Insurance Company(KPIC) and fill your prescription at a MedImpact network pharmacy. Please note that this Formulary does not have a specialty drug tier. If you are covered by a KPIC PPO plan with a specialty drug tier, please see the KPIC PPO and Out-of- Area Indemnity (OOA) Formulary with Specialty Drug Tier. Access to the most current version of the Formulary can be obtained by visiting: kp.org/kpic-ca-rx-ppo-gf. For help understanding your KPIC insurance plan benefits, including cost sharing for drugs under the prescription drug benefit and under the medical benefit, please call 1-800-788-0710 or 711 (TTY) Monday through Friday, 7 a.m. to 7 p.m. For help with this Formulary, including the processes for submitting an exception request and requesting prior authorization and step therapy exceptions, please call MedImpact 24 hours a day, 7 days a week, at 1-800- 788-2949 or 711 (TTY). For information about your cost share for the outpatient prescription drug benefits in your specific plan, please visit: kp.org/kpic-ca-rx-ppo-gf. -

Insulin Aspart PI
Insulin Aspart Injection HIGHLIGHTS OF PRESCRIBING INFORMATION Insulin aspart is stable in infusion fluids such as 0.9% • Fluid retention and heart failure with concomitant use of thiazolidinediones (TZDs): Observe for signs and symptoms of These highlights do not include all the information sodium chloride. • Individualize and adjust the dosage of insulin aspart based heart failure; consider dosage reduction or discontinuation if needed to use insulin aspart safely and effectively. heart failure occurs (5.7). See full prescribing information for insulin aspart. on route of administration, the individual’s metabolic needs, blood glucose monitoring results and glycemic control goal • Hyperglycemia and Ketoacidosis Due to Insulin Pump Device Insulin Aspart Injection, for subcutaneous or (2.4). Malfunction: Monitor glucose and administer insulin aspart by intravenous use • Dosage adjustments may be needed with changes in physical subcutaneous injection if pump malfunction occurs (5.8). Initial U.S. Approval: 2000 activity, changes in meal patterns (i.e., macronutrient content ——— ADVERSE REACTIONS ——— ——— RECENT MAJOR CHANGES ——— or timing of food intake), changes in renal or hepatic function Adverse reactions observed with insulin aspart include: Dosage and Administration (2.1)-----------------------------------12/2018 or during acute illness (2.4). hypoglycemia, allergic reactions, local injection site reactions, Dosage and Administration (2.2) ----------------------------------11/2019 ——— DOSAGE FORMS AND STRENGTHS ——— lipodystrophy, rash, and pruritus (6). Warnings and Precautions (5.2) -----------------------------------11/2019 Each presentation contains 100 Units of insulin aspart per mL To report SUSPECTED ADVERSE REACTIONS, contact (U-100) Novo Nordisk Pharma, Inc. at 1-800-727-6500 or FDA ——— INDICATIONS AND USAGE ——— • 10 mL multiple-dose vial (3) at 1-800-FDA-1088 or www.fda.gov/medwatch. -

Liraglutide (Victoza) for the Indication 'Type 2 Diabetes Mellitus'
29090847 liraglutide (Victoza®) Pharmacotherapeutic report liraglutide (Victoza®) for the indication type 2 diabetes mellitus Date 9th November 2009. 1. Summary The Medicines Evaluation Committee (CFH) has approved a pharmacotherapeutic report for the medicine liraglutide (Victoza®) injection solution. In order to determine its therapeutic value, it was compared with NPH insulin and exenatide. They reached the following conclusions: Efficacy In a single direct comparative study with liraglutide in combination with metformin and/or a sulphonyllurea (SU)-derivative, a reduction was achieved in the HbA1c and fasting blood sugar levels. Significantly more patients achieved the <7% target value for HbA1c in comparison with exenatide in combination with metformin and/or an SU-derivative. However, the clinical relevance of the difference in the HbA1c reduction is limited, the liraglutide dose in the study is higher than the recommended 1,2 mg daily dose, the doses of metformin and the SU-derivatives are unknown. It was also an open-label study. In a single, direct, open-label study, liraglutide in combination with metformin and glimepiride significantly reduced the HbA1c-value in comparison with insulin glargine. In this study the liraglutide dose was also higher than the recommended dose, which may have a limited but extra effect on the reduction in the HbA1c. Furthermore, there is some doubt as to whether the regulation on insulin was optimal in the comparative study with insulin. Unlike insulin, the use of liraglutide and exenatide induces weight loss. Efficacy For liraglutide data demonstrating its efficacy with respect to micro- and macrovascular complications and life expectancy are not available. Neither has the efficacy of exenatide on clinically relevant final outcomes been demonstrated.The efficacy of insulin has been demonstrated, particularly on the occurrence of microvascular complications. -

WO 2018/144867 Al 09 August 2018 (09.08.2018) W!P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2018/144867 Al 09 August 2018 (09.08.2018) W!P O PCT (51) International Patent Classification: Diego, CA 92130 (US). LIN, Jui-chen; 8875 Costa Verde A61K 31/702 (2006.01) C12N 15/17 {2006.01) Blvd., Apt 1603, San Diego, CA 92122 (US). A61K 45/06 (2006.01) G01N 33/50 (2006.01) (74) Agent: LANGER, Michael, R. et al; Michael Best & CI2N 15/16 (2006.01) Friedrich LLP, 100 East Wisconsin Avenue, Suite 3300, (21) International Application Number: Milwaukee, W I 53218-4108 (US). PCT/US20 18/0 16647 (81) Designated States (unless otherwise indicated, for every (22) International Filing Date: kind of national protection available): AE, AG, AL, AM, 02 February 2018 (02.02.2018) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, (25) Filing Language: English DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, (26) Publication Language: English HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (30) Priority Data: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, 62/454,613 03 February 2017 (03.02.2017) U S OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (71) Applicant: VANDERBILT UNIVERSITY [US/US]; 305 SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, Kirkland Hall, 2201 West End Avenue, Nashville, TN TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW.