Topical Corticosteroids: Back to Basics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Policy: Topical Agents: Corticosteroids
Clinical Policy: Topical Agents: Corticosteroids Reference Number: OH.PHAR.PPA.92 Effective Date: 01/01/2020 Revision Log Last Review Date: Line of Business: Medicaid See Important Reminder at the end of this policy for important regulatory and legal information. Description TOPICAL AGENTS: CORTICOSTEROIDS – LOW POTENCY NO PA REQUIRED “PREFERRED” PA REQUIRED “NON- PREFERRED” DESONIDE cream, ointment (generic of Desowen®) ALCLOMETASONE cream, ointment (generic of FLUOCINOLONE ACETONIDE 0.01% cream, solution Aclovate®) (generic of Synalar®) CAPEX® shampoo (fluocinolone acetonide) FLUOCINOLONE body oil, scalp oil (generic of Derma- DESONATE®gel (desonide) Smoothe/ FS®) DESONIDE lotion (generic of Desowen®) HYDROCORTISONE cream, lotion, ointment HYDROCORTISONE ACETATE WITH ALOE gel HYDROCORTISONE WITH UREA cream (generic of Carmol HC®) PANDEL® cream (hydrocortisone probutate) PEDIADERM HC® kit TOPICAL AGENTS: CORTICOSTEROIDS – MEDIUM POTENCY NO PA REQUIRED “PREFERRED” PA REQUIRED “NON--PREFERRED” BETAMETHASONE DIPROPIONATE-CALCIPOTRIENE BETAMETHASONE DIPROPIONATE lotion (generic of Ointment Diprolene®) BETAMETHASONE VALERATE cream, lotion (generic of CLOCORTOLONE PIVALATE (generic of Cloderm®) Valisone®) CORDRAN® tape (flurandrenolide) FLUTICASONE PROPIONATE cream, ointment (generic of DESOXIMETASONE cream, gel, ointment (generic of Cutivate®) Topicort®) MOMETASONE FUROATE cream, ointment, solution FLUOCINOLONE ACETONIDE 0.025% cream, ointment (generic of Elocon®) (generic of Synalar®) PREDNICARBATE cream (generic of Dermatop®) FLUTICASONE -

Steroids Topical
Steroids, Topical Therapeutic Class Review (TCR) September 18, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. September -

April 1, 2019
BUREAU FOR MEDICAL SERVICES EFFECTIVE WEST VIRGINIA MEDICAID PREFERRED DRUG LIST WITH PRIOR AUTHORIZATION CRITERIA 04/01/2019 This is not an all-inclusive list of available covered drugs and includes only Version 2019.2e managed categories. Refer to cover page for complete list of rules governing this PDL. Prior authorization for a non-preferred agent in any class will be given only if there has been a trial of the preferred brand/generic equivalent or preferred formulation of the active ingredient, at a therapeutic dose, that resulted in a partial response with a documented intolerance. Prior authorization of a non-preferred isomer, pro-drug, or metabolite will be considered with a trial of a preferred parent drug of the same chemical entity, at a therapeutic dose, that resulted in a partial response with documented intolerance or a previous trial and therapy failure, at a therapeutic dose, with a preferred drug of a different chemical entity indicated to treat the submitted diagnosis. (The required trial may be overridden when documented evidence is provided that the use of these preferred agent(s) would be medically contraindicated.) Unless otherwise specified, the listing of a particular brand or generic name includes all legend forms of that drug. OTC drugs are not covered unless specified. PA criteria for non-preferred agents apply in addition to general Drug Utilization Review policy that is in effect for the entire pharmacy program, including, but not limited to, appropriate dosing, duplication of therapy, etc. The use of pharmaceutical samples will not be considered when evaluating the members’ medical condition or prior prescription history for drugs that require prior authorization. -

LGC Standards Pharmacopoeial Reference Standards 2014
LL CTS INKSP RODUTO A L P ITH W WEBSHO LGC Standards Pharmacopoeial reference standards 2014 FOR STANDARDS WITH CofA SEE OUR CATALOGUE: PHARMACEUTICAL IMPURITIES AND PRIMARY REFERENCE STANDARDS LGC Quality – ISO Guide 34 • GMP/GLP • ISO 9001 • ISO/IEC 17025 • ISO/IEC 17043 Pharmaceutical impurities Code Product CAS No. CS Price Unit Adiphenine Hydrochloride O LGC Standards N O MM1172.00 Adiphenine Hydrochloride 50-42-0 A 250mg HCl Pharmaceutical impurities and Adrenaline Tartrate OH H OH O OH primary reference standardsMM0614.00 2014 N OH Adrenaline Tartrate 51-42-3 A 500mg OH OH O OH OH H MM0614.02 L-Adrenaline 51-43-4 A 500mg OH N OH Imp. C (EP) as Hydrochloride: 1-(3,4-Di- O H OH MM0614.13 hydroxyphenyl)-2-(methylamino)ethanone 62-13-5 A 100mg N HCl Hydrochloride (Adrenalone Hydrochloride) OH (1R)-1-(3,4-Dihydroxyphenyl)-2- OH O S O MM0614.01 methylaminoethanesulphonic Acid H 78995-75-2 A 100mg OH N (Adrenaline -Sulphonate) OH Alanine NH2 MM0566.00 Alanine 56-41-7 A 500mg OH O Imp. A (Pharmeuropa): (2 S)-2-Aminobutanedioic Acid O NH 2 MM0567.00 OH (Aspartic Acid) 56-84-8 A 500mg OH O Albendazole O H MM0382.00 Albendazole N O 54965-21-8 A 500mg N H S N Imp. A (EP): 5-(Propylsulphanyl)-1H- H MM0382.01 N 80983-36-4 A 100mg NH2 benzimidazol-2-amine S N O H Imp. B (EP): Methyl [5-Propylsulphinyl)- N O MM0382.02 N 54029-12-8 A 100mg H 1H-benzimidazol-2-yl]carbamate S N O O H Imp. -

And Their Covered Alternatives for the Premier and Premier Plus Pharmacy Plans 2020 Formulary Exclusions Drug List
Covered and non-covered drugs Drugs not covered — and their covered alternatives for the Premier and Premier Plus pharmacy plans 2020 Formulary Exclusions Drug List 05.03.925.1O (7/20) Formulary Exclusions Drug List effective July 1, 2020 Key Premier and Premier Plus pharmacy plans UPPERCASE Brand-name medicine lowercase italics Generic medicine Category Not covered Covered alternatives Analgesics acetaminophen/caffeine/dihydrocodeine acetaminophen/caffeine/dihydrocodeine cap tab 325-30-16 mg 320.5-30-16mg (generic TREZIX) ALLZITAL (butalbital/acetaminophen) butalbital/acetaminophen 50-325mg bupap butalbital/acetaminophen 50-300mg ANAPROX DS** (naproxen) Generic oral nonsteroidal anti-inflammatory drug FENORTHO* (fenoprofen calcium) FLECTOR PATCH (diclofenac epolamine) INDOCIN SUPP* (indomethacin) INDOCIN SUSP* (indomethacin) ketoprofen 25mg capsules ketoprofen er MOBIC** (meloxicam) NAPRELAN* (naproxen sodium) SPRIX (ketorolac trometh nasal spray) TIVORBEX (indomethacin) VIVLODEX (meloxicam) VOLTAREN** (diclofenac) ZIPSOR (diclofenac potassium) ZORVOLEX (diclofenac) CONZIP* (tramadol ER capsules) tramadol immediate-release or extended-release tablets (generic ULTRAM, ULTRAM ER) DEXPAK 6 DAY** (dexamethasone) dexamethasone tab therapy pack DEXPAK 10 DAY** (dexamethasone) DEXPAK 13** (dexamethasone) TAPERDEX 6 DAY (dexamethasone) LAZANDA (fentanyl citrate nasal spray) fentanyl citrate lozenge (generic ACTIQ) SUBSYS (fentanyl sublingual spray) LIDODERM** (lidocaine) lidocaine patch 5% NALOCET oxycodone-acetaminophen (generic PERCOCET) PERCOCET** -
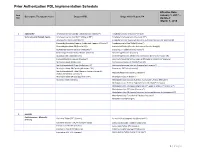
Prior Authorization PDL Implementation Schedule
Prior Authorization PDL Implementation Schedule Effective Date: Item January 1, 2017 – Descriptive Therapeutic Class Drugs on PDL Drugs which Require PA Nbr Updated: March 1, 2018 1 ADD/ADHD Amphetamine Salt Combo Tablet ( Generic Adderall®) Amphetamine ODT (Adzenys® XR ODT) Stimulants and Related Agents Amphetamine Salt Combo ER (Adderall XR®) Amphetamine Suspension (Dyanavel XR®) Atomoxetine Capsule (Strattera®) Amphetamine Salt Combo ER (Generic; Authorized Generic for Adderall XR) Dexmethylphenidate (Generic; Authorized Generic of Focalin®) Amphetamine Sulfate Tablet (Evekeo®) Dexmethylphenidate ER (Focalin XR®) Armodafinil Tablet (Generic; Authorized Generic; Nuvigil®) Dextroamphetamine Solution (Procentra®) Clonidine ER Tablet (Generic; Kapvay®) Dextroamphetamine Sulfate Tablet (Generic) Dexmethylphenidate (Focalin®) Guanfacine ER Tablet (Generic) Dexmethylphenidate XR (Generic; Authorized Generic for Focalin XR) Lisdexamfetamine Capsule (Vyvanse®) Dextroamphetamine Sulfate Capsule ER (Generic; Dexedrine®Spansule) Methylphenidate IR (Generic) Dextroamphetamine IR Tablet (Zenzedi®) Methylphenidate ER Chew (Quillichew ER®) Dextroamphetamine Solution (Generic for Procentra®) Methylphenidate ER Capsule (Metadate CD®) Guanfacine ER Tablet (Intuniv®) Methylphenidate ER Tablet (Generic; Generic Concerta®; Methamphetamine (Generic; Desoxyn®) Authorized Generic Concerta®) Methylphenidate ER Susp (Quillivant XR®) Methylphenidate IR (Ritalin®) Modafinil Tablet (Generic) Methylphenidate Solution (Generic; Authorized Generic; Methylin®) Methylphenidate -

Wo 2008/127291 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (43) International Publication Date PCT (10) International Publication Number 23 October 2008 (23.10.2008) WO 2008/127291 A2 (51) International Patent Classification: Jeffrey, J. [US/US]; 106 Glenview Drive, Los Alamos, GOlN 33/53 (2006.01) GOlN 33/68 (2006.01) NM 87544 (US). HARRIS, Michael, N. [US/US]; 295 GOlN 21/76 (2006.01) GOlN 23/223 (2006.01) Kilby Avenue, Los Alamos, NM 87544 (US). BURRELL, Anthony, K. [NZ/US]; 2431 Canyon Glen, Los Alamos, (21) International Application Number: NM 87544 (US). PCT/US2007/021888 (74) Agents: COTTRELL, Bruce, H. et al.; Los Alamos (22) International Filing Date: 10 October 2007 (10.10.2007) National Laboratory, LGTP, MS A187, Los Alamos, NM 87545 (US). (25) Filing Language: English (81) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of national protection available): AE, AG, AL, AM, AT,AU, AZ, BA, BB, BG, BH, BR, BW, BY,BZ, CA, CH, (30) Priority Data: CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, 60/850,594 10 October 2006 (10.10.2006) US ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, (71) Applicants (for all designated States except US): LOS LR, LS, LT, LU, LY,MA, MD, ME, MG, MK, MN, MW, ALAMOS NATIONAL SECURITY,LLC [US/US]; Los MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PG, PH, PL, Alamos National Laboratory, Lc/ip, Ms A187, Los Alamos, PT, RO, RS, RU, SC, SD, SE, SG, SK, SL, SM, SV, SY, NM 87545 (US). -

Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Seborrheic Dermatitis
Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Seborrheic Dermatitis Diagnosis: SEBORRHEIC DERMATITIS GENERAL INFORMATION: • Seborrheic dermatitis is a common, benign skin condition that is thought to be caused by overgrowth of a yeast that resides on the skin, Malassezia. • In infants, this typically resolves within the first year of life, so treatment is not required. • In children and teenagers, this may be chronic, requiring maintenance therapy. TREATMENT RECOMMENDATIONS: For children/teenagers: Scalp: • Maintenance shampoo 2-3 times weekly (or less frequently for drier hair types), shampoo should be allowed to sit for ~5 minutes before rinsing) o Ketoconazole 2% shampoo o OTC Selenium sulfide shampoos (Selsun Blue, Head and Shoulders Clinical Strength) o OTC Pyrithione zinc shampoos (Head and Shoulders Classic Clean) • For symptomatic relief: Fluocinolone 0.01% (Derma smoothe oil) or clobetasol 0.05% solution twice daily as needed. Face: • Miconazole 1 % cream (or other anti-yeast medication) mixed in equal amounts with hydrocortisone 2.5% cream (or other class 5, 6, 7 topical steroid) For infants with generalized skin involvement • Mild: Miconazole 1 % cream (or other anti-yeast medication) mixed in equal amounts with hydrocortisone 2.5% ointment (or other class 5, 6, 7 topical steroid) • Severe: Miconazole 1 % cream (or other anti-yeast medication) mixed in equal amounts with triamcinolone 0.1% ointment (or other class 3 or 4 topical steroid) REFERRAL GUIDELINES: Please refer patients who fail treatment guidelines above. Please avoid referring patients who are frustrated by need for maintenance therapy, as this is expected. Educational recommendations are made from the best evidence, expert opinions and consideration for the patients and families cared for by the service. -
Diflorasone Diacetate Cream USP, 0.05% Should Not Be Used in the Treatment of Rosacea Or Perioral for External Use Only - Not for Ophthalmic Use
4.5" 4.5" FRONT BACK Diflorasone Diacetate 0.75" 0.75" Cream USP, 0.05% PK-2768-2 0815-2 358 Rx only USP should be discontinued until the infection has been adequately controlled. Diflorasone diacetate cream USP, 0.05% should not be used in the treatment of rosacea or perioral For External Use Only - Not for Ophthalmic Use. dermatitis, and it should not be used on the face, groin, or axillae. DESCRIPTION Information for Patients: Patients using topical corticosteroids should receive the following Diflorasone diacetate cream USP, 0.05% contains the active compound diflorasone diacetate, a information and instructions: synthetic corticosteroid for topical dermatological use. 1. The medication is to be used as directed by the physician. It is for external use only. Chemically, diflorasone diacetate is 6α, 9α-difluoro-11β,17,21-trihydroxy-16-methylpregna-1,4- Avoid contact with the eyes. diene-3,20-dione 17,21 diacetate, with the empirical formula C26H32F2O7, a molecular weight of 494.5, 2. The medication should not be used for any disorder other than that for which it was prescribed. and the following structural formula: 3. The treated skin area should not be bandaged or otherwise covered or wrapped so as to be 135 10 O occlusive unless directed by the physician. 4. Patients should report to their physician any signs of local adverse reactions. O H3C O H H3C O CH3 2 6 HO Laboratory Tests: The following tests may be helpful in evaluating patients for HPA axis suppression: H O ACTH-stimulation test H C 3 CH3 A.M. -

Corticosteroids Topical Quantity Limit
QUANTITY LIMIT PRIOR AUTHORIZATION CRITERIA DRUG CLASS DERMATOLOGICAL TOPICAL CORTICOSTEROIDS BRAND AND GENERIC ALL DOSAGE FORMS BRAND NAME* BRAND AND GENERIC (generic) ALCLOMETASONE: (alclometasone dipropionate) AMCINONIDE: (amcinonide) BETAMETHASONE: (betamethasone dipropionate) (betamethasone valerate) CLOBETASOL: (clobetasol propionate) CLOCORTOLONE: (clocortolone pivalate) DESONIDE: (desonide) DESOXIMETASONE: (desoximetasone) DIFLORASONE: (diflorasone diacetate) FLUOCINOLONE: (fluocinolone acetonide) FLUOCINONIDE: (fluocinonide) FLURANDRENOLIDE: (flurandrenolide, include tape) FLUTICASONE: (fluticasone propionate) HALCINONIDE: Corticosteroids Topical (Brand and Generic) Limit-Post Limit 2324-HJ 03-2019 ©2019 CVS Caremark. All rights reserved. This document contains confidential and proprietary information of CVS Caremark and cannot be reproduced, distributed or printed without written permission from CVS Caremark. This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with CVS Caremark. 1 (halcinonide) HALOBETASOL: (halobetasol propionate) HYDROCORTISONE: (hydrocortisone) (hydrocortisone acetate) (hydrocortisone butyrate) (hydrocortisone probutate) (hydrocortisone valerate) MOMETASONE: (mometasone furoate) PREDNICARBATE: (prednicarbate) TRIAMCINOLONE: (triamcinolone acetonide) Status: CVS Caremark Criteria Type: Quantity Limit; Post Limit Prior Authorization Ref # 2324-HJ** * Drugs that are listed in the target drug box include -

Diflorasone Diacetate 0.05% ST
MEDICARE PART D STEP THERAPY CRITERIA diflorasone diacetate 0.05% Plan Limitations: Does not apply to the following Blue Shield of California Medicare Part D plans: o Blue Shield 65 Plus (HMO) in Fresno, Kern, San Luis Obispo, Santa Barbara, and Ventura counties o Blue Shield 65 Plus Choice Plan (HMO) o Blue Shield 65 Plus (HMO) in Los Angeles, Orange, and San Bernardino counties o Blue Shield 65 Plus (HMO) in Riverside, and San Diego counties o Blue Shield 65 Plus (HMO) in Sacramento County o Blue Shield Medicare Basic Plan (PDP) o Blue Shield Medicare Enhanced Plan (PDP) Step Therapy Criteria: 1) Step One: medium, high, or very high potency topical corticosteroid agents (amcinonide 0.1% (lotion, cream, ointment), betamethasone dipropionate 0.05% (lotion, cream, ointment), betamethasone valerate 0.1% (lotion, cream, ointment), augmented betamethasone 0.05% (lotion, cream, gel, ointment), clobetasol 0.05% (lotion, solution, shampoo, cream, foam, gel, ointment, spray, emollient cream, emollient foam), clocortolone pivalate 0.1% cream, desoximetasone 0.05% (cream, gel, ointment), desoximetasone 0.25% (cream, ointment), diflorasone 0.05% (cream, ointment), fluocinolone 0.01% (cream, solution), fluocinonide 0.05% (cream, gel, ointment, solution), fluocinonide 0.1% cream, fluticasone 0.05% lotion, halobetasol propionate 0.05% (cream, ointment), hydrocortisone butyrate 0.1% cream, hydrocortisone valerate 0.2% (cream, ointment), mometasone 0.1% (cream, ointment, solution), prednicarbate 0.1% (cream, ointment), triamcinolone acetonide 0.1% (lotion, cream, ointment), triamcinolone acetonide 0.147mg/gram topical aerosol), triamcinolone acetonide 0.5% (cream, ointment) 2) Step Two: If any claims history of two step one drugs within the past 180 days, then diflorasone diacetate 0.05% is approved for coverage. -

Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Psoriasis
Texas Children's Hospital Dermatology Service PCP Referral Guidelines- Psoriasis Diagnosis: PSORIASIS TREATMENT RECOMMENDATIONS: • Careful physical exam for possible strep infection (throat, perianal area, inguinal folds) and treatment if positive. • Careful history for persistent or frequent history of morning stiffness or joint pain Location Eyelids Elidel 1% cream (or other calcineurin inhibitor) Face, Axillae, Hydrocortisone 2.5% ointment (or other Class 6 or 7 topical steroid) Inguinal Folds Body Thin/mild: Triamcinolone 0.1% ointment (or other Class 3, 4 topical steroid) Thick/severe: Mometasone 0.1% ointment (or other Class 1 or 2 topical steroid) Scalp Mild (or patients with dry hair): Fluocinolone 0.01% (Derma-smoothe) oil Severe: Clobetasol 0.05 % solution Shampoo: (over-the-counter) • Salicylic acid containing shampoo (e.g. T sal shampoo) • Tar containing shampoo (e.g. T gel shampoo) • Baker’s P&S shampoo Nails Mometasone 0.1% ointment (or other Class 1 or 2 topical steroid) • Apply medication to nail folds/cuticle PATIENT RESOURCES: National Psoriasis Foundation www.psoriasis.org REFERRAL RECOMMENDATIONS: • Please refer patient if there is extensive involvement (>5-10% BSA), or localiZed involvement that has failed treatment recommendations above. • If patient has persistent morning stiffness or joint complaints, please also refer to rheumatology for evaluation for possible psoriatic arthritis Educational recommendations are made from the best evidence, expert opinions and consideration for the patients and families cared for by the service. This is NOT intended to impose standards of care preventing selective variation in practice that are necessary to meet the unique needs of individual patients. The physician must consider each patient’s circumstance to make the ultimate judgment regarding best care.