Medical Foundations of Workers' Compensation Conditions of The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Painful Heel Comparative Study in Rheumatoid Arthritis, Ankylosing Spondylitis, Reiter's Syndrome, and Generalized Osteoarthrosis
Ann Rheum Dis: first published as 10.1136/ard.36.4.343 on 1 August 1977. Downloaded from Annals of the Rheumatic Diseases, 1977, 36, 343-348 The painful heel Comparative study in rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthrosis J. C. GERSTER, T. L. VISCHER, A. BENNANI, AND G. H. FALLET From the Department of Medicine, Division of Rheumatology, University Hospital, Geneva, Switzerland SUMMARY This study presents the frequency of severe and mild talalgias in unselected, consecutive patients with rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthosis. Achilles tendinitis and plantar fasciitis caused a severe talalgia and they were observed mainly in males with Reiter's syndrome or ankylosing spondylitis. On the other hand, sub-Achilles bursitis more frequently affected women with rheumatoid arthritis and rarely gave rise to severe talalgias. The simple calcaneal spur was associated with generalized osteoarthrosis and its frequency increased with age. This condition was not related to talalgias. Finally, clinical and radiological involvement of the subtalar and midtarsal joints were observed mainly in rheumatoid arthritis and occasionally caused apes valgoplanus. copyright. A 'painful heel' syndrome occurs at times in patients psoriasis, urethritis, conjunctivitis, or enterocolitis. with inflammatory rheumatic disease or osteo- The antigen HLA B27 was present in 29 patients arthrosis, causing significant clinical problems. Very (80%O). few studies have investigated the frequency and characteristics of this syndrome. Therefore we have RS 16 PATIENTS studied unselected groups of patients with rheuma- All of our patients had the complete triad (non- toid arthritis (RA), ankylosing spondylitis (AS), gonococcal urethritis, arthritis, and conjunctivitis). -

Upper Extremity
Upper Extremity Shoulder Elbow Wrist/Hand Diagnosis Left Right Diagnosis Left Right Diagnosis Left Right Adhesive capsulitis M75.02 M75.01 Anterior dislocation of radial head S53.015 [7] S53.014 [7] Boutonniere deformity of fingers M20.022 M20.021 Anterior dislocation of humerus S43.015 [7] S43.014 [7] Anterior dislocation of ulnohumeral joint S53.115 [7] S53.114 [7] Carpal Tunnel Syndrome, upper limb G56.02 G56.01 Anterior dislocation of SC joint S43.215 [7] S43.214 [7] Anterior subluxation of radial head S53.012 [7] S53.011 [7] DeQuervain tenosynovitis M65.42 M65.41 Anterior subluxation of humerus S43.012 [7] S43.011 [7] Anterior subluxation of ulnohumeral joint S53.112 [7] S53.111 [7] Dislocation of MCP joint IF S63.261 [7] S63.260 [7] Anterior subluxation of SC joint S43.212 [7] S43.211 [7] Contracture of muscle in forearm M62.432 M62.431 Dislocation of MCP joint of LF S63.267 [7] S63.266 [7] Bicipital tendinitis M75.22 M75.21 Contusion of elbow S50.02X [7] S50.01X [7] Dislocation of MCP joint of MF S63.263 [7] S63.262 [7] Bursitis M75.52 M75.51 Elbow, (recurrent) dislocation M24.422 M24.421 Dislocation of MCP joint of RF S63.265 [7] S63.264 [7] Calcific Tendinitis M75.32 M75.31 Lateral epicondylitis M77.12 M77.11 Dupuytrens M72.0 Contracture of muscle in shoulder M62.412 M62.411 Lesion of ulnar nerve, upper limb G56.22 G56.21 Mallet finger M20.012 M20.011 Contracture of muscle in upper arm M62.422 M62.421 Long head of bicep tendon strain S46.112 [7] S46.111 [7] Osteochondritis dissecans of wrist M93.232 M93.231 Primary, unilateral -

Frequency and Criticality of Diagnoses in Family Medicine Practices: from the National Ambulatory Medical Care Survey (NAMCS)
J Am Board Fam Med: first published as 10.3122/jabfm.2018.01.170209 on 12 January 2018. Downloaded from ORIGINAL RESEARCH Frequency and Criticality of Diagnoses in Family Medicine Practices: From the National Ambulatory Medical Care Survey (NAMCS) Michael R. Peabody, PhD, Thomas R. O’Neill, PhD, Keith L. Stelter, MD, MMM, and James C. Puffer, MD Background: Family medicine is a specialty of breadth, providing comprehensive health care for the individual and the family that integrates the broad scope of clinical, social, and behavioral sciences. As such, the scope of practice (SOP) for family medicine is extensive; however, over time many family phy- sicians narrow their SOP. We sought to provide a nationally representative description of the most com- mon and the most critical diagnoses that family physicians see in their practice. Methods: Data were extracted from the 2012 National Ambulatory Medical Care Survey (NAMCS) to select all ICD-9 codes reported by family physicians. A panel of family physicians then reviewed 1893 ICD-9 codes to place each code into an American Board of Family Medicine Family Medicine Certifica- tion Examination test plan specifications (TPS) category and provide a rating for an Index of Harm (IoH). Results: An analysis of all 1893 ICD-9 codes seen by family physicians in the 2012 NAMCS found that 198 ICD-9 codes could not be assigned a TPS category, leaving 1695 ICD-9 codes in the dataset. Top 10 lists of ICD-9 codes by TPS category were created for both frequency and IoH. Conclusions: This study provides a nationally representative description of the most common diag- copyright. -

Pediatric MSK Protocols
UT Southwestern Department of Radiology Ankle and Foot Protocols - Last Update 5-18-2015 Protocol Indications Notes Axial Coronal Sagittal Ankle / Midfoot - Routine Ankle Pain Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD SPAIR T1 FSE Injury, Internal Derangement Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR STIR Talar OCD, Coalition Protocol Indications Notes Axial Coronal Sagittal Ankle / Midfoot - Arthritis Arthritis Axial = In Relation to Leg "Footprint" (Long Axis to Foot) PD SPAIR PD SPAIR T1 FSE Coronal = In Relation to Leg (Short Axis Foot) STIR T1 SPIR POST T1 SPIR POST Protocol Indications Notes Axial Coronal Sagittal Foot - Routine Pain, AVN Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD FSE T1 FSE Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR PD SPAIR STIR Protocol Indications Notes Axial Coronal Sagittal Foot - Arthritis Arthritis Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD SPAIR STIR Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR T1 SPIR POST 3D WATS T1 SPIR POST Protocol Indications Notes Axial Coronal Sagittal Great Toe / MTP Joints Turf Toe Smallest Coil Possible (Microcoil if Available) PD FSE T1 FSE PD FSE Sesamoiditis FoV = Mid Metatarsal Through Distal Phalanges PD SPAIR PD SPAIR PD SPAIR Slice thickness = 2-3 mm, 10% gap Axial = In relation to the great toe (short axis foot) Coronal = In relation to the great toe (long axis foot / footprint) Appropriate Coronal Plane for Both Ankle and Foot Imaging UT Southwestern Department -

Desarrollo De La Podología En España
Desarrollo de la podología en España Virginia Novel Martí ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tdx.cat) i a través del Dipòsit Digital de la UB (diposit.ub.edu) ha estat autoritzada pels titulars dels drets de propietat intelꞏlectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX ni al Dipòsit Digital de la UB. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX o al Dipòsit Digital de la UB (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tdx.cat) y a través del Repositorio Digital de la UB (diposit.ub.edu) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR o al Repositorio Digital de la UB. -

Haglund's Syndrome, Retrocalaneal Exostosis
Open Access Review Article DOI: 10.7759/cureus.820 Haglund’s Syndrome: A Commonly Seen Mysterious Condition Raju Vaishya 1 , Amit Kumar Agarwal 1 , Ahmad Tariq Azizi 2 , Vipul Vijay 1 1. Orthopaedics, Indraprastha Apollo Hospitals 2. Orthopaedics, Herat Regional Hospital, Herat, Afghanistan Corresponding author: Amit Kumar Agarwal, [email protected] Abstract Haglund’s deformity was first described by Patrick Haglund in 1927. It is also known as retrocalcaneal exostosis, Mulholland deformity, and ‘pump bump.' It is a very common clinical condition, but still poorly understood. Haglund’s deformity is an abnormality of the bone and soft tissues in the foot. An enlargement of the bony section of the heel (where the Achilles tendon is inserted) triggers this condition. The soft tissue near the back of the heel can become irritated when the large, bony lump rubs against rigid shoes. The aetiology is not well known, but some probable causes like a tight Achilles tendon, a high arch of the foot, and heredity have been suggested as causes. Middle age is the most common age of affection, females are more affected than males, and the occurence is often bilateral. A clinical feature of this condition is pain in the back of the heel, which is more after rest. Clinical evaluation and lateral radiographs of the ankle are mostly enough to make a diagnosis of Haglund’s syndrome. Haglund’s syndrome is often treated conservatively by altering the heel height in shoe wear, orthosis, physiotherapy, and anti-inflammatory drugs. Surgical excision of the bony exostoses of the calcaneum is only required in resistant cases. -

Overuse Injuries in Elite Athletes
ATHLETES: OVERUSE MRI of Overuse INJURIES VERY COMMON Injury in the Elite Athlete • Muscle William B. Morrison, M.D. Associate Professor of • Joints Radiology Thomas Jefferson • Tendon University Hospital Philadelphia, PA USA • Ligament • Bone [email protected] How is this Relevant to My Practice? • High performance athletes get similar injuries as ‘regular’ people… but: – More of them, & at a younger age MUSCLE / SOFT TISSUE – More commonly imaged – Secondary gain involved INJURY • All the cases here are high performance athletes – but most injuries are conventional • Exceptions – Some weird sport-specific patterns of stress and other injuries – Acute injuries as opposed to overuse •Overuse –DOMS Muscle Injury Delayed Onset Muscle • Acute injury Soreness (DOMS) – Tendon – Myotendinous junction • All athletes are susceptible if they – Muscle belly change training regimen • Athletes tend to work out intensely – leads to muscle injury • Rarely imaged (“no pain no gain”) – Weightlifting / aerobic exercise – 24hr later – soreness – Can be severe, even look like a tear 1 Acute Muscle Injury • Direct → muscle belly, esp quadriceps T2 – esp rugby, football • Indirect → myotendinous junction – eccentric contraction – sudden acceleration / DOMS: Lateral gastrocnemius deceleration Finding can be subtle, even with T2 and fat sat Professional football player Acute Injury – T1 Quadriceps hematoma Muscle belly injury Myotendinous Unit Hit with helmet • Myotendinous Junction – ‘weak link’ of normal myotendinous complex T2 – Common place for injury – Most common mechanism: eccentric contraction (muscle lengthens and contracts at the same High time) T1 = blood Gastrocnemius tear: Grade 1 Muscle Strain “V” sign • Ill-defined edema T2 T1 STIR Weishaupt D, JCAT 2001; 25:677 2 Gd Gd can help identify Grade 2 Muscle Strain subtle muscle injury AKA “Partial Tear” STIR Professional baseball player Grade 1 strain Sartorius m. -

Information to Users
INFORMATION TO USERS This manuscript has been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter free, i ^ e others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely afreet reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand comer and continuing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. Higher quality 6” x 9” black and white photographic prints are available for any photographs or illustrations appearing in this copy for an additional charge. Contact UMI directly to order. UMI A Bell & Howell Information Compaiy 300 North Zeeb Road, Ann Arbor MI 48106-1346 USA 313/761-4700 800/521-0600 PHYSIOLOGIC RESPONSES TO INFLAMMATION IN ISOLATED EQUINE JOINTS DISSERTATION Presented in Partial Fulfilment of the Requirements for the Degree of Doctor of Philosophy in the Graduate School of The Ohio State University B y Joanne Hardy, D.V.M., M.S. -

20-0420 ) Issued: April 21, 2021 U.S
United States Department of Labor Employees’ Compensation Appeals Board __________________________________________ ) D.H., Appellant ) ) and ) Docket No. 20-0420 ) Issued: April 21, 2021 U.S. POSTAL SERVICE, BEVERLY POST ) OFFICE, Beverly, MA, Employer ) __________________________________________ ) Appearances: Case Submitted on the Record Katherine A. Harrell, for the appellant1 Office of Solicitor, for the Director DECISION AND ORDER Before: ALEC J. KOROMILAS, Chief Judge PATRICIA H. FITZGERALD, Alternate Judge VALERIE D. EVANS-HARRELL, Alternate Judge JURISDICTION On December 13, 2019 appellant, through his representative, filed a timely appeal from an October 16, 2019 nonmerit decision of the Office of Workers’ Compensation Programs (OWCP). As more than 180 days has elapsed from the last merit decision dated December 18, 2018 to the filing of this appeal, pursuant to the Federal Employees’ Compensation Act2 (FECA) and 20 C.F.R. §§ 501.2(c) and 501.3, the Board lacks jurisdiction over the merits of this case. 1 In all cases in which a representative has been authorized in a matter before the Board, no claim for a fee for legal or other service performed on appeal before the Board is valid unless approved by the Board. 20 C.F.R. § 501.9(e). No contract for a stipulated fee or on a contingent fee basis will be approved by the Board. Id. An attorney or representative’s collection of a fee without the Board’s approval may constitute a misdemeanor, subject to fine or imprisonment for up to one year or both. Id.; see also 18 U.S.C. § 292. Demands for payment of fees to a representative, prior to approval by the Board, may be reported to appropriate authorities for investigation. -

Chronic Superficial Achilles Bursitis Treated with Percutaneous Bursectomy and Platelet-Rich Plasma Injection
Extended Abstract Journal of Medical science 2020 Vol.4 No.3 Chronic Superficial Achilles Bursitis Treated with which had already been diagnosed with Achilles Percutaneous Bursectomy and Platelet-Rich Plasma tendinitis. He had followed several months of physical Injection: A Case Report therapy, oral anti-inflammatory drugs, and used a shoe Colberg RE*, Umarvadia JS and Walsh KP shoe and heel lift shoes without much relief. On examination, the patient had a severe sensitivity to Andrews Sports Medicine & Orthopedic Center, palpation throughout the Achilles superficial bursa, from Birmingham, AL, USA the medial to the lateral and from the proximal to the Keywords: Chronic ankle pain; Bursitis; Achilles tendon; distal. On ultrasound, his superficial Achilles bursa was Haglund deformity; Platelet-rich plasma; Radiofrequency chronically inflamed and there was no pathology in the coblation; Ultrasonography real tendon. Patient had Haglund deformity. Introduction Given the chronicity of his symptoms and the failure of conservative measures, the patient was offered a The Achilles tendon is the largest tendon in the body, surgical consultation for an open bursectomy and a connecting the gastrocnemius and soleus muscles to the Haglund resection; however, the patient indicated that calcaneus. It contains both a retrocalcanean bursa he was not interested in surgery at this time due to anterior to the tendon when it is inserted and a larger scarring issues and wanted to exhaust the minimally and more superficial subcutaneous bursa posterior to the invasive options. The patient was informed of the tendon. Although Achilles superficial bursitis is not possibility of injecting platelet rich plasma (PRP) into the related to a specific injury, it is usually due to repetitive bursa to stimulate the healing of tissues compared to the stress on the insertion of the tendon on the calcaneus. -
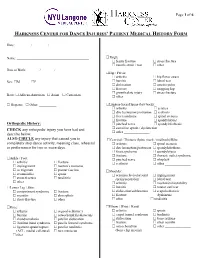
Harkness Center for Dance Injuries' Patient Medical History Form
Page 1 of 6 HARKNESS CENTER FOR DANCE INJURIES’ PATIENT MEDICAL HISTORY FORM Date: ________ / ________ / ________ Name: __________________________________________ Thigh: femur fracture stress fracture muscle strain / tear other_______________ Date of Birth: _______ / _______ / _______ Hip / Pelvis: arthritis hip flexor strain Sex: M F bursitis labral tear dislocation osteitis pubis fracture snapping hip growth plate injury stress fracture Race: African-American Asian Caucasian other _______________ Hispanic Other: __________ Lumbar-Sacral Spine (low back): arthritis sciatica disc herniation/protrusion scoliosis facet syndrome spinal stenosis fracture spondylolysis Orthopedic History: pinched nerve spondylolisthesis CHECK any orthopedic injury you have had and sacroiliac sprain / dysfunction other _______________ describe below. ALSO CIRCLE any injury that caused you to Cervical / Thoracic Spine (neck / mid back)/Ribs: completely stop dance activity, meaning class, rehearsal arthritis spinal stenosis or performance for two or more days. disc herniation/protrusion spondylolisthesis facet syndrome spondylolysis fracture thoracic outlet syndrome Ankle / Foot: pinched nerve whiplash arthritis fracture scoliosis other _______________ impingement morton’s neuroma os trigonum plantar fasciitis Shoulder: sesamoiditis sprain acromioclavicular joint impingement stress fracture tendinitis sprain/separation labral tear other________________ arthritis mechanical instability Lower Leg / Shin: -

Patient Medical History Form
Date of Visit: ________ / ________ / ________ ID # (R=Research) +MR# Patient Medical History Form Name: __________________________________________ Knee: arthritis osgood-schlatter’s Date of Birth: _______ / _______ / _______ Sex: M F bursitis osteochondritis dissecans Social Security ______-_____-________ chondromalacia patellar dislocation iliotibial band syndrome patella femoral syndrome Race: African-American Asian Caucasian ligament sprain/rupture patellar tendinitis Hispanic Other: __________ (ACL, medial collateral) torn meniscus other________________ Address:___________________________________________ ______________________________________________ Thigh: femur fracture stress fracture City: _________________ State: _______ ZIP: ________ muscle strain / tear other_______________ Primary Phone: _______ - ________ - __________ Hip / Pelvis: Email: ___________________________________________ arthritis hip flexor strain bursitis labral tear Emergency Contact Information: dislocation osteitis pubis Name: ___________________________________________ fracture snapping hip growth plate injury stress fracture Relation: ______________ Phone:_____________________ other _______________ Health Insurance Information: Lumbar-Sacral Spine (low back): Name of Insurance Co: _____________________________ arthritis sciatica Name of Policy Holder: _____________________________ disc herniation/protrusion scoliosis facet syndrome spinal stenosis Policy #: _________________ Group#: ________________ fracture spondylolsysis