Disorders of Mitochondrial Long-Chain Fatty Acid Oxidation and the Carnitine Shuttle
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Upregulation of Peroxisome Proliferator-Activated Receptor-Α And
Upregulation of peroxisome proliferator-activated receptor-α and the lipid metabolism pathway promotes carcinogenesis of ampullary cancer Chih-Yang Wang, Ying-Jui Chao, Yi-Ling Chen, Tzu-Wen Wang, Nam Nhut Phan, Hui-Ping Hsu, Yan-Shen Shan, Ming-Derg Lai 1 Supplementary Table 1. Demographics and clinical outcomes of five patients with ampullary cancer Time of Tumor Time to Age Differentia survival/ Sex Staging size Morphology Recurrence recurrence Condition (years) tion expired (cm) (months) (months) T2N0, 51 F 211 Polypoid Unknown No -- Survived 193 stage Ib T2N0, 2.41.5 58 F Mixed Good Yes 14 Expired 17 stage Ib 0.6 T3N0, 4.53.5 68 M Polypoid Good No -- Survived 162 stage IIA 1.2 T3N0, 66 M 110.8 Ulcerative Good Yes 64 Expired 227 stage IIA T3N0, 60 M 21.81 Mixed Moderate Yes 5.6 Expired 16.7 stage IIA 2 Supplementary Table 2. Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis of an ampullary cancer microarray using the Database for Annotation, Visualization and Integrated Discovery (DAVID). This table contains only pathways with p values that ranged 0.0001~0.05. KEGG Pathway p value Genes Pentose and 1.50E-04 UGT1A6, CRYL1, UGT1A8, AKR1B1, UGT2B11, UGT2A3, glucuronate UGT2B10, UGT2B7, XYLB interconversions Drug metabolism 1.63E-04 CYP3A4, XDH, UGT1A6, CYP3A5, CES2, CYP3A7, UGT1A8, NAT2, UGT2B11, DPYD, UGT2A3, UGT2B10, UGT2B7 Maturity-onset 2.43E-04 HNF1A, HNF4A, SLC2A2, PKLR, NEUROD1, HNF4G, diabetes of the PDX1, NR5A2, NKX2-2 young Starch and sucrose 6.03E-04 GBA3, UGT1A6, G6PC, UGT1A8, ENPP3, MGAM, SI, metabolism -

Downloaded from GEO
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Oxylipin metabolism is controlled by mitochondrial b-oxidation during bacterial inflammation. Mariya Misheva1, Konstantinos Kotzamanis1*, Luke C Davies1*, Victoria J Tyrrell1, Patricia R S Rodrigues1, Gloria A Benavides2, Christine Hinz1, Robert C Murphy3, Paul Kennedy4, Philip R Taylor1,5, Marcela Rosas1, Simon A Jones1, Sumukh Deshpande1, Robert Andrews1, Magdalena A Czubala1, Mark Gurney1, Maceler Aldrovandi1, Sven W Meckelmann1, Peter Ghazal1, Victor Darley-Usmar2, Daniel White1, and Valerie B O’Donnell1 1Systems Immunity Research Institute and Division of Infection and Immunity, and School of Medicine, Cardiff University, UK, 2Department of Pathology, University of Alabama at Birmingham, Birmingham, AL 35294, USA, 3Department of Pharmacology, University of Colorado Denver, Aurora, CO 80045, USA, 4Cayman Chemical 1180 E Ellsworth Rd, Ann Arbor, MI 48108, United States, 5UK Dementia Research Institute at Cardiff, Cardiff University, UK Address correspondence: Valerie O’Donnell, [email protected] or Daniel White, [email protected], Systems Immunity Research Institute, Cardiff University *Both authors contributed equally to the study 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -
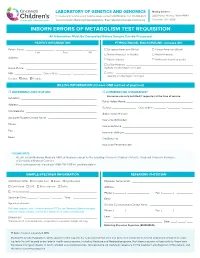
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

Health Effects Support Document for Perfluorooctanoic Acid (PFOA)
United States Office of Water EPA 822-R-16-003 Environmental Protection Mail Code 4304T May 2016 Agency Health Effects Support Document for Perfluorooctanoic Acid (PFOA) Perfluorooctanoic Acid – May 2016 i Health Effects Support Document for Perfluorooctanoic Acid (PFOA) U.S. Environmental Protection Agency Office of Water (4304T) Health and Ecological Criteria Division Washington, DC 20460 EPA Document Number: 822-R-16-003 May 2016 Perfluorooctanoic Acid – May 2016 ii BACKGROUND The Safe Drinking Water Act (SDWA), as amended in 1996, requires the Administrator of the U.S. Environmental Protection Agency (EPA) to periodically publish a list of unregulated chemical contaminants known or anticipated to occur in public water systems and that may require regulation under SDWA. The SDWA also requires the Agency to make regulatory determinations on at least five contaminants on the Contaminant Candidate List (CCL) every 5 years. For each contaminant on the CCL, before EPA makes a regulatory determination, the Agency needs to obtain sufficient data to conduct analyses on the extent to which the contaminant occurs and the risk it poses to populations via drinking water. Ultimately, this information will assist the Agency in determining the most appropriate course of action in relation to the contaminant (e.g., developing a regulation to control it in drinking water, developing guidance, or deciding not to regulate it). The PFOA health assessment was initiated by the Office of Water, Office of Science and Technology in 2009. The draft Health Effects Support Document for Perfluoroctanoic Acid (PFOA) was completed in 2013 and released for public comment in February 2014. -

(LCHAD) Deficiency / Mitochondrial Trifunctional Protein (MTF) Deficiency
Long chain acyl-CoA dehydrogenase (LCHAD) deficiency / Mitochondrial trifunctional protein (MTF) deficiency Contact details Introduction Regional Genetics Service Long chain acyl-CoA dehydrogenase (LCHAD) deficiency / mitochondrial trifunctional Levels 4-6, Barclay House protein (MTF) deficiency is an autosomal recessive disorder of mitochondrial beta- 37 Queen Square oxidation of fatty acids. The mitochondrial trifunctional protein is composed of 4 alpha London, WC1N 3BH and 4 beta subunits, which are encoded by the HADHA and HADHB genes, respectively. It is characterized by early-onset cardiomyopathy, hypoglycemia, T +44 (0) 20 7762 6888 neuropathy, and pigmentary retinopathy, and sudden death. There is also an infantile F +44 (0) 20 7813 8578 onset form with a hepatic Reye-like syndrome, and a late-adolescent onset form with primarily a skeletal myopathy. Tandem mass spectrometry of organic acids in urine, Samples required and carnitines in blood spots, allows the diagnosis to be unequivocally determined. An 5ml venous blood in plastic EDTA additional clinical complication can occur in the pregnant mothers of affected fetuses; bottles (>1ml from neonates) they may experience maternal acute fatty liver of pregnancy (AFLP) syndrome or Prenatal testing must be arranged hypertension/haemolysis, elevated liver enzymes and low platelets (HELLP) in advance, through a Clinical syndrome. Genetics department if possible. The genes encoding the HADHA and HADHB subunits are located on chromosome Amniotic fluid or CV samples 2p23.3. The pathogenic -

Lipid Metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives
cancers Review Lipid metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives 1, 1, 1 2 1 Laurence Pellerin y, Lorry Carrié y , Carine Dufau , Laurence Nieto , Bruno Ségui , 1,3 1, , 1, , Thierry Levade , Joëlle Riond * z and Nathalie Andrieu-Abadie * z 1 Centre de Recherches en Cancérologie de Toulouse, Equipe Labellisée Fondation ARC, Université Fédérale de Toulouse Midi-Pyrénées, Université Toulouse III Paul-Sabatier, Inserm 1037, 2 avenue Hubert Curien, tgrCS 53717, 31037 Toulouse CEDEX 1, France; [email protected] (L.P.); [email protected] (L.C.); [email protected] (C.D.); [email protected] (B.S.); [email protected] (T.L.) 2 Institut de Pharmacologie et de Biologie Structurale, CNRS, Université Toulouse III Paul-Sabatier, UMR 5089, 205 Route de Narbonne, 31400 Toulouse, France; [email protected] 3 Laboratoire de Biochimie Métabolique, CHU Toulouse, 31059 Toulouse, France * Correspondence: [email protected] (J.R.); [email protected] (N.A.-A.); Tel.: +33-582-7416-20 (J.R.) These authors contributed equally to this work. y These authors jointly supervised this work. z Received: 15 September 2020; Accepted: 23 October 2020; Published: 27 October 2020 Simple Summary: Melanoma is a devastating skin cancer characterized by an impressive metabolic plasticity. Melanoma cells are able to adapt to the tumor microenvironment by using a variety of fuels that contribute to tumor growth and progression. In this review, the authors summarize the contribution of the lipid metabolic network in melanoma plasticity and aggressiveness, with a particular attention to specific lipid classes such as glycerophospholipids, sphingolipids, sterols and eicosanoids. -

A Systems Chemoproteomic Analysis of Acyl-Coa/Protein Interaction Networks
bioRxiv preprint doi: https://doi.org/10.1101/665281; this version posted July 18, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. A systems chemoproteomic analysis of acyl-CoA/protein interaction networks Michaella J. Levy,1# David C. Montgomery,2# Mihaela E. Sardiu,1 Sarah E. Bergholtz,2 Kellie D. Nance, 2 Jose Montano,2 Abigail L. Thorpe,2 Stephen D. Fox,3 Qishan Lin,4 Thorkell Andresson,3 Laurence Florens,1 Michael P. Washburn,1,5 and Jordan L. Meier2* 1. Stowers Institute for Medical Research, Kansas City, MO, 64110, USA 2. Chemical Biology Laboratory, Center for Cancer Research, National Cancer Institute, National Institutes of Health, Frederick, MD, 21702, USA. 3. Laboratory of Proteomics and Analytical Technologies, Leidos, Inc, Frederick National Laboratory for Cancer Research, Frederick, Maryland 21702, USA 4. RNA Epitranscriptomics & Proteomics Resource, University of Albany, 1400 Washington Ave, Albany, NY 12222 5. Department of Pathology and Laboratory Medicine, University of Kansas Medical Center, Kansas City, KS, 66160, USA # M.J.L. and D.C.M. contributed equally to this work. * Lead contact to whom correspondence should be addressed. Email: [email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/665281; this version posted July 18, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Summary 2 Acyl-CoA/protein interactions are required for many functions essential to life including membrane synthesis, 3 oxidative metabolism, and macromolecular acetylation. -

Supplemental Table 1. List of Candidate Gene Filters Used in the Analysis of Exome Sequencing. MYOPATHY NEUROPATHY MND ABHD5
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) J Neurol Neurosurg Psychiatry Supplemental table 1. List of candidate gene filters used in the analysis of exome sequencing. MYOPATHY NEUROPATHY MND ABHD5 AAAS AAAS ACADL AARS1 AARS1 ACADM ABCA1 AGT ACADS ABCD1 ALAD ACADVL ABHD12 ALS2 ACTA1 ADCY6 ANG ADSSL1 AFG3L2 APEX1 AGL AIFM1 APOE AGPAT2 AMACR AR AGRN ANG ASAH1 AIRE AP1S1 ATM ALDOA APOA1 ATP7A ALG14 APTX ATXN2 ALG2 ARHGEF10 ATXN3 ALG3 ARL6IP1 B4GALT6 ANKRD2 ARSA BCL11B ANO5 ASAH1 BCL6 ASCC1 ATL1 BICD2 ATGL ATL3 BSCL2 ATP2A1 ATM C19orf12 ATRN ATXN1 C9orf72 B3GALNT2 ATXN10 CCS B3GNT2 ATXN2 CDH13 BAG3 ATXN3 CDH22 BIN1 ATXN7 CHCHD10 BSCL2 B2M CHMP2B BVES B4GALNT1 CNTF CACNA1S BAG3 CNTN4 CAPN3 BCKDHB CNTN6 CASQ1 BSCL2 CRIM1 CAV1 C12orf65 CRYM CAV3 C9orf72 CSNK1G3 CAVIN1 CLP1 CST3 CCDC78 CNTNAP1 CUL4B CDKN1C COX10 CYP2D6 CFL2 COX6A1 DAO Grunseich C, et al. J Neurol Neurosurg Psychiatry 2021;0:1–11. doi: 10.1136/jnnp-2020-325437 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) J Neurol Neurosurg Psychiatry CHAT CPOX DCAF15 CHCHD10 CRYAB DCTN1 CHD7 CTDP1 DIAPH3 CHKB CTSA DISC1 CHN1 CYP27A1 DNAJB2 CHRM3 DARS2 DOC2B CHRNA1 DDHD1 DPP6 CHRNB1 DGUOK DYNC1H1 CHRND DHH EFEMP1 CHRNE DHTKD1 ELP3 CIDEC DMD EPHA4 CLCN1 DNAJB2 EWSR1 CLN3 DNAJC3 EXOSC3 CNBP DNM2 FBLN5 CNTN1 DYNC1H1 FBXO38 COA3 EGR2 FEZF2 COL12A1 EMD FGGY COL13A1 ERCC6 FIG4 COL6A ERCC8 FUS COL6A1 FAH GARS1 COL6A2 FAM126A GBE1 COL6A3 FBLN5 GMPPA COL9A3 FGD4 GRB14 COLQ FGF14 GRN COX10 FIG4 HEXA COX15 FLNC HFE CPT2 FLRT1 HINT1 CRAT FLVCR1 HSPB1 CRPPA FMR1 HSPB3 CRYAB FUS HSPB8 CTNS FXN IGHMBP2 DAG1 GALC ITPR2 DECR1 GAN KDR DES GARS1 KIFAP3 DGUOK GBA2 KLHL9 DIH1 GBE1 LAMA2 DMD GDAP1 LAS1L DMPK GJB1 LIF DNAJB6 GJB3 LIPC DNAJC19 GLA LOX Grunseich C, et al. -

Free PDF Download
European Review for Medical and Pharmacological Sciences 2019; 23: 1710-1721 Next-generation sequencing identifies a homozygous mutation in ACADVL associated with pediatric familial dilated cardiomyopathy S.J. CARLUS1, I.S. ALMUZAINI2, M. KARTHIKEYAN3, L. LOGANATHAN3, G.S. AL-HARBI1, A.M. ABDALLAH4, K.M. AL-HARBI1 1Pediatrics Department, Cardiogenetics Unit, College of Medicine, Taibah University, Al-Madinah, Kingdom of Saudi Arabia 2Department of Pediatric Cardiology, Al-Madinah Maternity and Children Hospital (MMCH), Al-Madinah, Kingdom of Saudi Arabia 3Department of Bioinformatics, Alagappa University, Karaikudi, Tamil Nadu, India 4West Midlands Regional Genetics Laboratory, Birmingham Women’s NHS Foundation Trust, Birmingham, United Kingdom Abstract. – OBJECTIVE: Pediatric familial di- Key Words lated cardiomyopathy (DCM) is a rare and se- Pediatric familial dilated cardiomyopathy, Targeted vere heart disease. The genetics of familial DCM gene sequencing, ACADVL, Saudi Arabia, Consanguinity, are complex and include over 100 known dis- Molecular docking, Molecular dynamics. ease-causing genes, but many causative genes are unknown. We aimed to identify the causative gene for DCM in a consanguineous Saudi Ara- bian family with affected family members and a history of sudden death. Introduction PATIENTS AND METHODS: Affected (two chil- dren) and unaffected (one sibling and the mother) Dilated cardiomyopathy (DCM) is a heart family members were screened by next-gener- ation sequencing (NGS) for 181 candidate DCM disease characterized by ventricular dilation and genes and underwent metabolic screening. Fif- impaired myocardial contractility. DCM affects ty-seven clinically annotated controls and 46 DCM 1 in 2500 of the general population and is one of cases were then tested for the identified mutation. -

EGL Test Description
2460 Mountain Industrial Boulevard | Tucker, Georgia 30084 Phone: 470-378-2200 or 855-831-7447 | Fax: 470-378-2250 eglgenetics.com Inherited Metabolic Disorders Panel: Sequencing and CNV Analysis Test Code: MM310 Turnaround time: 6 weeks CPT Codes: 81404 x1, 81406 x1, 81405 x1 Condition Description Inherited metabolic disorders refer to diseases caused by defects in genes that are involved in the body’s metabolism. These usually involve the production, conversion, or use of energy. Traditionally, inherited metabolic conditions were broadly classified as disorders of carbohydrate metabolism, amino acid metabolism, organic acid metabolism, or lysosomal storage diseases. This test analyses genes involved in complex metabolic processes in the body including but not limited to the above four categories. Reference: OMIM. Genes ACAD9, ACADL, ACADM, ACADS, ACADVL, ACSF3, AGA, AGL, ALDH5A1, ARSA, ASL, ASS1, ATPAF2, AUH, BCKDHA, BCKDHB, CD320, CLN3, CLN5, CLN6, CLN8, CPS1, CPT1A, CPT2, CYP27A1, DBT, DLD, ENO3, ETFA, ETFB, ETFDH, G6PC, GAA, GALC, GALNS, GBA, GBE1, GLA, GLB1, GM2A, GNPTAB, GYS1, GYS2, HADHA, HADHB, HGSNAT, HMGCL, HMGCS2, HYAL1, IDS, IDUA, IVD, LIPA, LMBRD1, LPIN1, MAN2B1, MANBA, MCCC1, MCCC2, MCEE, MCOLN1, MFSD8, MLYCD, MMAA, MMAB, MMACHC, MMADHC, MMUT, MTR, MTRR, NAGA, NAGLU, NAGS, NEU1, NPC1, NPC2, OPA3, OTC, PC, PCCA, PCCB, PFKM, POLG, PPT1, PYGL, PYGM, SERAC1, SGSH, SLC17A5, SLC22A5, SLC25A13, SLC25A15, SLC25A20, SLC37A4, SLC7A7, SMPD1, SUCLG1, SUMF1, TAZ, TMEM70, TPP1 Indications This test is indicated for: Confirmation of a clinical diagnosis of inherited metabolic disorders. Methodology Next Generation Sequencing: In-solution hybridization of all coding exons is performed on the patient's genomic DNA. Although some deep intronic regions may also be analyzed, this assay is not meant to interrogate most promoter regions, deep intronic regions, or other regulatory elements, and does not detect single or multi-exon deletions or duplications. -

Proteomic Survey Towards the Tissue-Specific Proteins of Mouse Mitochondria
SCIENCE CHINA Life Sciences SPECIAL TOPIC January 2011 Vol.54 No.1: 3–15 • RESEARCH PAPERS • doi: 10.1007/s11427-010-4107-0 Proteomic survey towards the tissue-specific proteins of mouse mitochondria WANG Yuan, SUN HaiDan, RU YaWei, YIN SongYue, YIN Liang & LIU SiQi* Beijing Institute of Genomics, Chinese Academy of Sciences, Beijing 101300, China Received June 29, 2010; accepted July 30, 2010 Mitochondrion plays the key functions in mammalian cells. It is believed that mitochondrion exerts the common biologic func- tions in many tissues, but also performs some specific functions correspondent with tissues where it is localized. To identify the tissue-specific mitochondrial proteins, we carried out a systematic survey towards mitochondrial proteins in the tissues of C57BL/6J mouse, such as liver, kidney and heart. The mitochondrial proteins were separated by 2DE and identified by MALDI-TOF/TOF MS. Total of 87 unique proteins were identified as the tissue-specific ones, and some representatives were further verified through ICPL quantification and Western blot. Because these issue-specific proteins are coded from nuclear genes, real-time PCR was employed to examine the mRNA status of six typical genes found in the tissues.With combining of the expression data and the co-localization images obtained from confocal microscope, we came to the conclusion that the tis- sue-specifically mitochondrial proteins were widely distributed among the mouse tissues. Our investigation, therefore, indeed provides a solid base to further explore the biological significance of the mitochondrial proteins with tissue-orientation. proteomics, tissue-specific, mitochondria Citation: Wang Y, Sun H D, Ru Y W, et al. -

HADHB Gene Hydroxyacyl-Coa Dehydrogenase Trifunctional Multienzyme Complex Subunit Beta
HADHB gene hydroxyacyl-CoA dehydrogenase trifunctional multienzyme complex subunit beta Normal Function The HADHB gene provides instructions for making part of an enzyme complex called mitochondrial trifunctional protein. This enzyme complex functions in mitochondria, the energy-producing centers within cells. Mitochondrial trifunctional protein is made of eight parts (subunits). Four alpha subunits are produced from the HADHA gene, and four beta subunits are produced from the HADHB gene. As the name suggests, mitochondrial trifunctional protein contains three enzymes that each perform a different function. The beta subunits contain one of the enzymes, known as long-chain 3-keto- acyl-CoA thiolase. The alpha subunits contain the other two enzymes. These enzymes are essential for fatty acid oxidation, which is the multistep process that breaks down ( metabolizes) fats and converts them to energy. Mitochondrial trifunctional protein is required to metabolize a group of fats called long- chain fatty acids. Long-chain fatty acids are found in foods such as milk and certain oils. These fatty acids are stored in the body's fat tissues. Fatty acids are a major source of energy for the heart and muscles. During periods of fasting, fatty acids are also an important energy source for the liver and other tissues. Health Conditions Related to Genetic Changes Mitochondrial trifunctional protein deficiency Researchers have identified at least 26 mutations in the HADHB gene that cause mitochondrial trifunctional protein deficiency. These mutations reduce all three enzyme activities of mitochondrial trifunctional protein. Most mutations change one of the protein building blocks (amino acids) used to make the beta subunit. A change in amino acids probably alters the subunit's structure, which disrupts all three activities of the enzyme complex.