RISPERDAL CONSTA® Risperidone NEW ZEALAND DATA SHEET
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Medication Conversion Chart
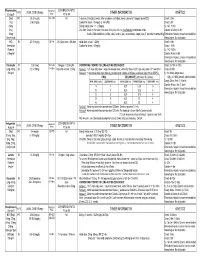
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Adjunctive Risperidone Treatment for Antidepressant-Resistant
Supplementary Online Content Krystal JH, Rosenheck RA, Cramer JA, et al. Adjunctive risperidone treatment for antidepressant- resistant symptoms of chronic military service–related PTSD. JAMA. 2011;306(5):493-502. eTable 1. Follow-up Drugs Started After Randomization eTable 2. Baseline Medications eTable 3. Number of Different Drugs From Each Major Class Each Patient Is Taking at Baseline eTable 4. Baseline Medication Combinations eTable 5. Adverse Events eFigure 1. Product-Limit Survival Estimates With Number of Subjects at Risk eFigure 2. Percentage of Veterans at Each CAPS Severity Level at 24 Weeks, by Treatment This supplementary material has been provided by the authors to give readers additional information about their work. © 2011 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/23/2021 eTable 1. Follow-up Drugs Started After Randomization Placebo Risperidone N= 134 N= 133 Total Patients % Patients % Patients % p-value Drugs started after randomization 46 34.3 59 44.4 105 39.3 0.10 Adrenergic Drugs 4 3.0 5 3.8 9 3.4 0.75 Atenolol 0 0.0 2 1.5 2 0.7 Metoprolol 3 2.2 2 1.5 5 1.9 Propranolol 1 0.7 1 0.8 2 0.7 Opiates 22 16.4 19 14.3 41 15.4 0.73 Codeine 1 0.7 1 0.8 2 0.7 Fentanyl 3 2.2 0 0.0 3 1.1 Hydrocodone (With Or Without 13 9.7 10 7.5 23 8.6 Acetaminophen) Methadone 1 0.7 0 0.0 1 0.4 Morphine 3 2.2 2 1.5 5 1.9 Oxycodone (With Or Without 4 3.0 7 5.3 11 4.1 Acetaminophen) Tramadol 3 2.2 2 1.5 5 1.9 Psycho-Stimulants 0 0.0 2 1.5 2 0.7 0.25 Methylphenidate 0 0.0 2 1.5 2 0.7 Muscle -
Recommended Methods for the Identification and Analysis Of
Vienna International Centre, P.O. Box 500, 1400 Vienna, Austria Tel: (+43-1) 26060-0, Fax: (+43-1) 26060-5866, www.unodc.org RECOMMENDED METHODS FOR THE IDENTIFICATION AND ANALYSIS OF AMPHETAMINE, METHAMPHETAMINE AND THEIR RING-SUBSTITUTED ANALOGUES IN SEIZED MATERIALS (revised and updated) MANUAL FOR USE BY NATIONAL DRUG TESTING LABORATORIES Laboratory and Scientific Section United Nations Office on Drugs and Crime Vienna RECOMMENDED METHODS FOR THE IDENTIFICATION AND ANALYSIS OF AMPHETAMINE, METHAMPHETAMINE AND THEIR RING-SUBSTITUTED ANALOGUES IN SEIZED MATERIALS (revised and updated) MANUAL FOR USE BY NATIONAL DRUG TESTING LABORATORIES UNITED NATIONS New York, 2006 Note Mention of company names and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. ST/NAR/34 UNITED NATIONS PUBLICATION Sales No. E.06.XI.1 ISBN 92-1-148208-9 Acknowledgements UNODC’s Laboratory and Scientific Section wishes to express its thanks to the experts who participated in the Consultative Meeting on “The Review of Methods for the Identification and Analysis of Amphetamine-type Stimulants (ATS) and Their Ring-substituted Analogues in Seized Material” for their contribution to the contents of this manual. Ms. Rosa Alis Rodríguez, Laboratorio de Drogas y Sanidad de Baleares, Palma de Mallorca, Spain Dr. Hans Bergkvist, SKL—National Laboratory of Forensic Science, Linköping, Sweden Ms. Warank Boonchuay, Division of Narcotics Analysis, Department of Medical Sciences, Ministry of Public Health, Nonthaburi, Thailand Dr. Rainer Dahlenburg, Bundeskriminalamt/KT34, Wiesbaden, Germany Mr. Adrian V. Kemmenoe, The Forensic Science Service, Birmingham Laboratory, Birmingham, United Kingdom Dr. Tohru Kishi, National Research Institute of Police Science, Chiba, Japan Dr. -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209 -

INVEGA SUSTENNA® (Paliperidone Palmitate)
INVEGA SUSTENNA® INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable suspension, for intramuscular use (paliperidone palmitate) extended-release injectable suspension, for intramuscular use --------------------------- DOSAGE FORMS AND STRENGTHS --------------------------- HIGHLIGHTS OF PRESCRIBING INFORMATION Extended-release injectable suspension: 39 mg/0.25 mL, 78 mg/0.5 mL, 117 mg/0.75 mL, These highlights do not include all the information needed to use 156 mg/mL, or 234 mg/1.5 mL (3) INVEGA SUSTENNA® safely and effectively. See full prescribing information for INVEGA SUSTENNA®. ----------------------------------- CONTRAINDICATIONS ----------------------------------- INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable Known hypersensitivity to paliperidone, risperidone, or to any excipients in suspension, for intramuscular use INVEGA SUSTENNA®. (4) Initial U.S. Approval: 2006 -----------------------------WARNINGS AND PRECAUTIONS ----------------------------- WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS • Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with WITH DEMENTIA-RELATED PSYCHOSIS Dementia-Related Psychosis: Increased incidence of cerebrovascular adverse See full prescribing information for complete boxed warning. reactions (e.g. stroke, transient ischemic attack). (5.2) • Neuroleptic Malignant Syndrome: Manage with immediate discontinuation of Elderly patients with dementia-related psychosis treated with antipsychotic drug and close monitoring. (5.3) drugs are -

Treatment of Adult Major Depressive Disorder (MDD) Tool
Section: A B C D E F G Resources References Treatment of Adult Major Depressive Disorder (MDD) Tool This tool is designed to support primary care providers in the treatment of adult patients (≥ 18 years) who have major depressive disorder (MDD). MDD is the most prevalent depressive disorder, and approximately 7% of Canadians meet the diagnostic criteria every year.1,2 The treatment of MDD involves psychotherapy and/or pharmacotherapy. Providers should work with patients to create a treatment plan together using providers’ clinical expertise and keeping in mind the patient’s preferences, as well as the practicality, feasibility, availability and affordability of treatment. TABLE OF CONTENTS pg. 1 Section A: Overview of MDD pathway pg. 6 Section E: Complementary and alternative medicine pg. 2 Section B: Assessing suicidality and managing pg. 7 Section F: Follow-up and monitoring suicide-related behaviour pg. 9 Section G: Special patient populations pg. 3 Section C: Psychotherapy options pg. 10 Resources pg.3 Section D: Pharmacotherapy management SECTION A: Overview of MDD pathway Patient has suspected depression Talking Points It is important to provide your patient with non-judgmental care (e.g. “Being Consider unexpected life events (e.g. death in the family, diagnosed with depression is nothing to be ashamed of, it is very common and change in family status, financial crisis). Consider special many adults are diagnosed with it every year”) patient populations. • Don’t use clinical/psychiatric language (e.g. “mental health,” “psychiatric,” and/or “maladaptive”) unless the patient uses these terms first • Use understandable language for cognitive distortions (e.g. -
Enhancing Transdermal Delivery of Opioid Antagonists and Agonists Using Codrugs Linked to Bupropion Or Hydroxybupropion Audra L
University of Kentucky UKnowledge Pharmaceutical Sciences Faculty Patents Pharmaceutical Sciences 2-18-2014 Enhancing Transdermal Delivery of Opioid Antagonists and Agonists Using Codrugs Linked To Bupropion or Hydroxybupropion Audra L. Stinchcomb University of Kentucky Peter A. Crooks University of Kentucky, [email protected] Mohamad O. Hamad University of Kentucky, [email protected] Paul K. Kiptoo University of Kentucky Click here to let us know how access to this document benefits oy u. Follow this and additional works at: https://uknowledge.uky.edu/ps_patents Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Stinchcomb, Audra L.; Crooks, Peter A.; Hamad, Mohamad O.; and Kiptoo, Paul K., "Enhancing Transdermal Delivery of Opioid Antagonists and Agonists Using Codrugs Linked To Bupropion or Hydroxybupropion" (2014). Pharmaceutical Sciences Faculty Patents. 27. https://uknowledge.uky.edu/ps_patents/27 This Patent is brought to you for free and open access by the Pharmaceutical Sciences at UKnowledge. It has been accepted for inclusion in Pharmaceutical Sciences Faculty Patents by an authorized administrator of UKnowledge. For more information, please contact [email protected]. US008653271B2 (12) United States Patent (10) Patent N0.: US 8,653,271 B2 Stinchcomb et a]. (45) Date of Patent: Feb. 18, 2014 (54) ENHANCING TRANSDERMAL DELIVERY (58) Field of Classi?cation Search OF OPIOID ANTAGONISTS AND AGONISTS USPC ............................... .. 546/45, 44, 46; 514/282 USING CODRUGS LINKED TO BUPROPION See application ?le for complete search history. OR HYDROXYBUPROPION (56) References Cited (75) Inventors: Audra L. Stinchcomb, Lexington, KY (US); Peter A. Crooks, Nicholasville, U.S. PATENT DOCUMENTS KY (US); Mohamed O. Hamad, Lexington, KY (US); Paul K. -

Detection and Characterization of Pyromarkers of Smoked Drugs of Abuse
Graduate Theses, Dissertations, and Problem Reports 2012 Detection and characterization of pyromarkers of smoked drugs of abuse Rona Kiyomi Nishikawa West Virginia University Follow this and additional works at: https://researchrepository.wvu.edu/etd Recommended Citation Nishikawa, Rona Kiyomi, "Detection and characterization of pyromarkers of smoked drugs of abuse" (2012). Graduate Theses, Dissertations, and Problem Reports. 4904. https://researchrepository.wvu.edu/etd/4904 This Dissertation is protected by copyright and/or related rights. It has been brought to you by the The Research Repository @ WVU with permission from the rights-holder(s). You are free to use this Dissertation in any way that is permitted by the copyright and related rights legislation that applies to your use. For other uses you must obtain permission from the rights-holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/ or on the work itself. This Dissertation has been accepted for inclusion in WVU Graduate Theses, Dissertations, and Problem Reports collection by an authorized administrator of The Research Repository @ WVU. For more information, please contact [email protected]. DETECTION AND CHARACTERIZATION OF PYROMARKERS OF SMOKED DRUGS OF ABUSE Rona Kiyomi Nishikawa Dissertation submitted to the Eberly College of Arts and Sciences at West Virginia University in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Chemistry Committee of Advisors: Suzanne C. Bell, Ph.D., Chair R. Lloyd Carroll, Ph.D. Patrick S. Callery, Ph.D. Harry O. Finklea, Ph.D. Keith B. Morris, Ph.D. C. Eugene Bennett Department of Chemistry Morgantown, West Virginia 2012 Keywords: Fentanyl, Heroin, Pyrolysis, Pyromarkers, GC/MS Copyright © 2012 Rona Kiyomi Nishikawa 1 Abstract DETECTION AND CHARACTERIZATION OF PYROMARKERS OF SMOKED DRUGS OF ABUSE Rona Kiyomi Nishikawa Smoking or inhalation has increased in popularity as the choice route of administration of drugs of abuse amongst drug abusers. -

Synthesis and Characterization of TPGS–Gemcitabine Prodrug
RSC Advances View Article Online PAPER View Journal | View Issue Synthesis and characterization of TPGS– gemcitabine prodrug micelles for pancreatic Cite this: RSC Adv.,2016,6,60126 cancer therapy† Vaibhav Khare,ab Wejdan Al. Sakarchi,a Prem N. Gupta,b Anthony D. M. Curtisa and Clare Hoskins*a The therapeutic potential of a nucleoside analog, gemcitabine, is severely compromised due to its rapid clearance from systemic circulation by enzymatic degradation into an inactive metabolite. In the present investigation, micelles based on polymer–drug conjugate were developed for gemcitabine and investigated for their potential to improve cancer chemotherapy. The tocopherol poly(ethylene glycol) succinate 1000 (TPGS)–gemcitabine prodrug was synthesized via an amide linkage and characterised by analytical methods, including FT-IR, 1H NMR, and MALDI-TOF. The micellar formulation of TPGS– gemcitabine prodrug was developed by a self-assembly technique and evaluated for various Creative Commons Attribution-NonCommercial 3.0 Unported Licence. physicochemical parameters including particle size, polydispersity, morphology, critical micelle concentration and release profile. It was observed that gemcitabine present in TPGS–gemcitabine micelles was resistant to deamination by crude cytidine deaminase. The improved cytotoxicity of the micellar formulation was observed using TPGS–gemcitabine micelles against pancreatic cancer cells. Received 11th April 2016 Further, it was found that, unlike native gemcitabine, nucleoside transporters were not required for Accepted 14th June 2016 TPGS–Gem micelles to demonstrate their anticancer potential. These findings revealed that TPGS– DOI: 10.1039/c6ra09347g gemcitabine micelles may serve as a promising platform for gemcitabine in order to improve its www.rsc.org/advances anticancer efficacy. -

Optimal Duration of Risperidone Or Olanzapine Adjunctive Therapy to Mood Stabilizer Following Remission of a Manic Episode: a CANMAT Randomized Double-Blind Trial
Molecular Psychiatry (2016) 21, 1050–1056 OPEN © 2016 Macmillan Publishers Limited All rights reserved 1359-4184/16 www.nature.com/mp ORIGINAL ARTICLE Optimal duration of risperidone or olanzapine adjunctive therapy to mood stabilizer following remission of a manic episode: A CANMAT randomized double-blind trial LN Yatham1, S Beaulieu2, A Schaffer3, M Kauer-Sant’Anna4, F Kapczinski4, B Lafer5, V Sharma6, SV Parikh7, A Daigneault8, H Qian9, DJ Bond1, PH Silverstone10, N Walji1, R Milev11, P Baruch12, A da Cunha13, J Quevedo14, R Dias5, M Kunz4, LT Young15, RW Lam1 and H Wong16 Atypical antipsychotic adjunctive therapy to lithium or valproate is effective in treating acute mania. Although continuation of atypical antipsychotic adjunctive therapy after mania remission reduces relapse of mood episodes, the optimal duration is unknown. As many atypical antipsychotics cause weight gain and metabolic syndrome, they should not be continued unless the benefits outweigh the risks. This 52-week double-blind placebo-controlled trial recruited patients with bipolar I disorder (n = 159) who recently remitted from a manic episode during treatment with risperidone or olanzapine adjunctive therapy to lithium or valproate. Patients were randomized to one of three conditions: discontinuation of risperidone or olanzapine and substitution with placebo at (i) entry (‘0-weeks’ group) or (ii) at 24 weeks after entry (‘24-weeks’ group) or (iii) continuation of risperidone or olanzapine for the full duration of the study (‘52-weeks’ group). The primary outcome measure was time to relapse of any mood episode. Compared with the 0-weeks group, the time to any mood episode was significantly longer in the 24-weeks group (hazard ratio (HR) 0.53; 95% confidence interval (CI): 0.33, 0.86) and nearly so in the 52-weeks group (HR: 0.63; 95% CI: 0.39, 1.02). -
When and How to Use Long-Acting Injectable Antipsychotics
Savvy Psychopharmacology When and how to use long-acting injectable antipsychotics William Klugh Kennedy, PharmD, BCPP, FASHP ong-acting injectable antipsychotics Understanding the similarities and dif- (LAIs) are a pharmacotherapeutic op- ferences among LAIs7 and potential inter- L tion to help clinicians individualize patient variability of each LAI allows pre- schizophrenia treatment. LAIs have been scribers to tailor the dosing regimen to the available since the 1960s, starting with flu- patient more safely and efficiently (Table, phenazine and later haloperidol; however, page 42).1,8-11 All LAI antipsychotic formu- second-generation antipsychotics were not lations rely on absorption pharmacokinet- Vicki L. Ellingrod, available in the United States until 20071,2 ics (PK) rather than elimination PK, which PharmD, BCPP, FCCP and more are in development (Box).3,4 generally is true for sustained-release oral Series Editor Up to one-half of patients with schizo- formulations as well. Absorption half-life phrenia do not adhere to their medica- duration and absorption half-life variabil- tions.5 LAI use may mitigate relapse in ity are key concepts in LAI dosing. acute schizophrenia that is caused by poor adherence to oral medications. LAIs may Clinical pearls have a lower risk of dose-related adverse Before prescribing an LAI, check that your effects because of lower peak antipsychotic patient has no known contraindications plasma levels and less variation between to the active drug or delivery method. peak and trough plasma levels. LAIs may Peak-related adverse effects typically are decrease the financial burden of schizo- not contraindications, although they may phrenia and increase individual quality prompt you to start at a lower dose. -

Claire Cole, Lisa Jones, Jim Mcveigh, Andrew Kicman, Qutub Syed & Mark A
Claire Cole, Lisa Jones, Jim McVeigh, Andrew Kicman, Qutub Syed & Mark A. Bellis Acknowledgements The authors would like to thank the following for their contribution to the literature searching, design, proofing, editing and distribution of this document: Carol Chadwick. Sian Connolly, Layla English, Michael Evans-Brown, Dave Seddon, Olivia Wooding, Lee Tisdall, Ellie McCoy and Gemma Parry of the Centre for Public Health. We would also like to thank the International Harm Reduction Association (IHRA) for their support with launching this report at their 2010 conference. About the Authors Claire Cole and Lisa Jones are Senior Researchers at the Centre for Public Health, Liverpool John Moores University. Jim McVeigh is the Deputy Director and Reader in Substance Use Epidemiology at the Centre for Public Health. Professor Andrew Kicman is Head of Research and Development in the Department of Forensic Science and Drug Monitoring, The Drug Control Centre, at Kings College London. Professor Qutub Syed is the Regional Director for Health Protection Agency in the North West Region. Professor Mark A. Bellis is the Director of the Centre for Public Health. 1 Contents Executive Summary 4 1. Introduction 10 2. Methodology 13 3. Heroin 17 4. Cocaine and Crack Cocaine 25 5. Amphetamine and Methamphetamine 30 6. Ecstasy 33 7. Cannabis 36 8. Other Illicit Drugs 38 9. Public Health Response and Harm Reduction Messages 40 10. Summary 45 References 47 Appendix 1 - Glossary 55 List of Tables Table 1: Summary of drug adulteration evidence 5 Table 2: Summary