When and How to Use Long-Acting Injectable Antipsychotics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of Psychosis: 30 Years of Progress
Journal of Clinical Pharmacy and Therapeutics (2006) 31, 523–534 REVIEW ARTICLE Treatment of psychosis: 30 years of progress I. R. De Oliveira* MD PhD andM.F.Juruena MD *Department of Neuropsychiatry, School of Medicine, Federal University of Bahia, Salvador, BA, Brazil and Department of Psychological Medicine, Institute of Psychiatry, King’s College, University of London, London, UK phrenia. Thirty years ago, psychiatrists had few SUMMARY neuroleptics available to them. These were all Background: Thirty years ago, psychiatrists had compounds, today known as conventional anti- only a few choices of old neuroleptics available to psychotics, and all were liable to cause severe extra them, currently defined as conventional or typical pyramidal side-effects (EPS). Nowadays, new antipsychotics, as a result schizophrenics had to treatments are more ambitious, aiming not only to suffer the severe extra pyramidal side effects. improve psychotic symptoms, but also quality of Nowadays, new treatments are more ambitious, life and social reinsertion. We briefly but critically aiming not only to improve psychotic symptoms, outline the advances in diagnosis and treatment but also quality of life and social reinsertion. Our of schizophrenia, from the mid 1970s up to the objective is to briefly but critically review the present. advances in the treatment of schizophrenia with antipsychotics in the past 30 years. We conclude DIAGNOSIS OF SCHIZOPHRENIA that conventional antipsychotics still have a place when just the cost of treatment, a key factor in Up until the early 1970s, schizophrenia diagnoses poor regions, is considered. The atypical anti- remained debatable. The lack of uniform diagnostic psychotic drugs are a class of agents that have criteria led to relative rates of schizophrenia being become the most widely used to treat a variety of very different, for example, in New York and psychoses because of their superiority with London, as demonstrated in an important study regard to extra pyramidal symptoms. -
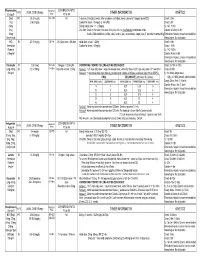
Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

Adjunctive Risperidone Treatment for Antidepressant-Resistant
Supplementary Online Content Krystal JH, Rosenheck RA, Cramer JA, et al. Adjunctive risperidone treatment for antidepressant- resistant symptoms of chronic military service–related PTSD. JAMA. 2011;306(5):493-502. eTable 1. Follow-up Drugs Started After Randomization eTable 2. Baseline Medications eTable 3. Number of Different Drugs From Each Major Class Each Patient Is Taking at Baseline eTable 4. Baseline Medication Combinations eTable 5. Adverse Events eFigure 1. Product-Limit Survival Estimates With Number of Subjects at Risk eFigure 2. Percentage of Veterans at Each CAPS Severity Level at 24 Weeks, by Treatment This supplementary material has been provided by the authors to give readers additional information about their work. © 2011 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/23/2021 eTable 1. Follow-up Drugs Started After Randomization Placebo Risperidone N= 134 N= 133 Total Patients % Patients % Patients % p-value Drugs started after randomization 46 34.3 59 44.4 105 39.3 0.10 Adrenergic Drugs 4 3.0 5 3.8 9 3.4 0.75 Atenolol 0 0.0 2 1.5 2 0.7 Metoprolol 3 2.2 2 1.5 5 1.9 Propranolol 1 0.7 1 0.8 2 0.7 Opiates 22 16.4 19 14.3 41 15.4 0.73 Codeine 1 0.7 1 0.8 2 0.7 Fentanyl 3 2.2 0 0.0 3 1.1 Hydrocodone (With Or Without 13 9.7 10 7.5 23 8.6 Acetaminophen) Methadone 1 0.7 0 0.0 1 0.4 Morphine 3 2.2 2 1.5 5 1.9 Oxycodone (With Or Without 4 3.0 7 5.3 11 4.1 Acetaminophen) Tramadol 3 2.2 2 1.5 5 1.9 Psycho-Stimulants 0 0.0 2 1.5 2 0.7 0.25 Methylphenidate 0 0.0 2 1.5 2 0.7 Muscle -
Management of Side Effects of Antipsychotics
Management of side effects of antipsychotics Oliver Freudenreich, MD, FACLP Co-Director, MGH Schizophrenia Program www.mghcme.org Disclosures I have the following relevant financial relationship with a commercial interest to disclose (recipient SELF; content SCHIZOPHRENIA): • Alkermes – Consultant honoraria (Advisory Board) • Avanir – Research grant (to institution) • Janssen – Research grant (to institution), consultant honoraria (Advisory Board) • Neurocrine – Consultant honoraria (Advisory Board) • Novartis – Consultant honoraria • Otsuka – Research grant (to institution) • Roche – Consultant honoraria • Saladax – Research grant (to institution) • Elsevier – Honoraria (medical editing) • Global Medical Education – Honoraria (CME speaker and content developer) • Medscape – Honoraria (CME speaker) • Wolters-Kluwer – Royalties (content developer) • UpToDate – Royalties, honoraria (content developer and editor) • American Psychiatric Association – Consultant honoraria (SMI Adviser) www.mghcme.org Outline • Antipsychotic side effect summary • Critical side effect management – NMS – Cardiac side effects – Gastrointestinal side effects – Clozapine black box warnings • Routine side effect management – Metabolic side effects – Motor side effects – Prolactin elevation • The man-in-the-arena algorithm www.mghcme.org Receptor profile and side effects • Alpha-1 – Hypotension: slow titration • Dopamine-2 – Dystonia: prophylactic anticholinergic – Akathisia, parkinsonism, tardive dyskinesia – Hyperprolactinemia • Histamine-1 – Sedation – Weight gain -

Sex-Specific Cannabidiol- and Iloperidone-Induced Neuronal Activity Changes in an in Vitro MAM Model System of Schizophrenia
International Journal of Molecular Sciences Article Sex-Specific Cannabidiol- and Iloperidone-Induced Neuronal Activity Changes in an In Vitro MAM Model System of Schizophrenia Rachel-Karson Thériault 1,2,†, Myles St-Denis 1,†, Tristen Hewitt 1,2, Jibran Y. Khokhar 2,3 , Jasmin Lalonde 1,2 and Melissa L. Perreault 2,3,* 1 Department of Molecular and Cellular Biology, University of Guelph, Guelph, ON N1G 2W1, Canada; [email protected] (R.-K.T.); [email protected] (M.S.-D.); [email protected] (T.H.); [email protected] (J.L.) 2 Collaborative Program in Neuroscience, University of Guelph, Guelph, ON N1G 2W1, Canada; [email protected] 3 Department of Biomedical Sciences, University of Guelph, Guelph, ON N1G 2W1, Canada * Correspondence: [email protected]; Tel.: +1-(519)-824-4120 (ext. 52013) † These authors contributed equally to this work. Abstract: Cortical circuit dysfunction is thought to be an underlying mechanism of schizophrenia (SZ) pathophysiology with normalization of aberrant circuit activity proposed as a biomarker for antipsychotic efficacy. Cannabidiol (CBD) shows potential as an adjunctive antipsychotic therapy; however, potential sex effects in these drug interactions remain unknown. In the present study, we sought to elucidate sex effects of CBD coadministration with the atypical antipsychotic iloperidone (ILO) on the activity of primary cortical neuron cultures derived from the rat methylazoxymethanol Citation: Thériault, R.-K.; St-Denis, acetate (MAM) model used for the study of SZ. Spontaneous network activity measurements were M.; Hewitt, T.; Khokhar, J.Y.; Lalonde, J.; Perreault, M.L. Sex-Specific obtained using a multielectrode array at baseline and following administration of CBD or ILO Cannabidiol- and Iloperidone- alone, or combined. -

Washington State Health Care Authority
Washington State Health Care Authority Prescription Drug Program 626 8th Ave SE, Olympia, WA 98501 ● 206-521-2029 https://www.hca.wa.gov/about-hca/prescription-drug-program February 17, 2021 Dear Interested Party, Based on recommendations by the Washington State Pharmacy and Therapeutics Committee, the Health Care Authority, Uniform Medical Plan (UMP), and the Department of Labor & Industries (L&I) have named the following drugs as preferred in their respective therapeutic classes on the Washington State Preferred Drug List (PDL), effective immediately: Antiplatelet reviewed 8/15/2018 Agency Coverage Ingredient Name Label Name of Preferred Product L&I UMP clopidogrel bisulfate clopidogrel tablet Not participating Yes The effect of this recommendation is no change to the Washington PDL. Second Generation Antipsychotics reviewed 12/18/2019 Agency Coverage Ingredient Name Label Name of Preferred Products L&I UMP aripiprazole Abilify Maintena® suspension reconstituted No Yes aripiprazole solution Yes Yes aripiprazole tablet Yes Yes aripiprazole ODT tablet dispersible Yes Yes aripiprazole lauroxil Aristada® injectable No Yes Aristada Initio® injectable No Yes asenapine maleate Saphris® sublingual Yes Yes brexpiprazole Rexulti® tablet Yes Yes cariprazine HCL Vraylar® capsule Yes Yes clozapine clozapine tablet Yes Yes clozapine ODT tablet dispersible Yes Yes iloperidone Fanapt® tablet Yes Yes Fanapt Titration Pack® tablet Yes Yes lurasidone HCL Latuda® tablet Yes Yes olanzapine olanzapine injectable No Yes olanzapine tablet Yes Yes olanzapine -

How to Identify and Manage Non-Response to Clozapine? T ⁎ Mujeeb U
Asian Journal of Psychiatry 45 (2019) 50–52 Contents lists available at ScienceDirect Asian Journal of Psychiatry journal homepage: www.elsevier.com/locate/ajp Short communication How to identify and manage non-response to clozapine? T ⁎ Mujeeb U. Shada,b,c, , Emma Felziena, Kamalika Roya,b, Simrat Sethib a School of Medicine, Oregon Health & Science University, Portland, Oregon, United States b Department of Psychiatry, Oregon State Hospital, Salem, Oregon, United States c Samaritan Mental Healthcare System, Corvallis, Oregon, United States ARTICLE INFO ABSTRACT Keywords: Clozapine is the only approved treatment for Treatment-Refractory Schizophrenia. Here we describe a case series Clozapine of three hospitalized patients with clozapine nonresponse. One of them responded to clozapine after dose ad- Non-response justments were made for an interaction between clozapine and ciprofloxacin. The other two cases remained Identify clozapine nonresponders despite optimizing clozapine treatment. However, both these patients responded to Manage other antipsychotic medications (APMs) with better tolerability than observed with clozapine treatment. This case series focuses on diagnosing a genuine from a pseudo-nonresponse to clozapine and to consider other APMs in genuine nonresponse before switching to invasive interventions, such as ECT. 1. Introduction medications (APMs), except in situations where bone marrow toxicity warrants clozapine discontinuation. Although augmentation strategies Since clozapine provides the only evidence-based treatment for with APMs, glutamate modulators and mood stabilizers have been patients with treatment-refractory schizophrenia (TRS) (Manu and proposed in ultra-treatment resistant schizophrenia (Naguy and Grudnikoff, 2016; Mukku et al., 2018), optimal efforts are warranted to Alamiri, 2019), a recent metanalysis reported a low quality of sup- confirm a true clozapine non-response before giving up on clozapine porting evidence for these clozapine augmentation strategies with the treatment. -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209 -

INVEGA SUSTENNA® (Paliperidone Palmitate)
INVEGA SUSTENNA® INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable suspension, for intramuscular use (paliperidone palmitate) extended-release injectable suspension, for intramuscular use --------------------------- DOSAGE FORMS AND STRENGTHS --------------------------- HIGHLIGHTS OF PRESCRIBING INFORMATION Extended-release injectable suspension: 39 mg/0.25 mL, 78 mg/0.5 mL, 117 mg/0.75 mL, These highlights do not include all the information needed to use 156 mg/mL, or 234 mg/1.5 mL (3) INVEGA SUSTENNA® safely and effectively. See full prescribing information for INVEGA SUSTENNA®. ----------------------------------- CONTRAINDICATIONS ----------------------------------- INVEGA SUSTENNA® (paliperidone palmitate) extended-release injectable Known hypersensitivity to paliperidone, risperidone, or to any excipients in suspension, for intramuscular use INVEGA SUSTENNA®. (4) Initial U.S. Approval: 2006 -----------------------------WARNINGS AND PRECAUTIONS ----------------------------- WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS • Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients with WITH DEMENTIA-RELATED PSYCHOSIS Dementia-Related Psychosis: Increased incidence of cerebrovascular adverse See full prescribing information for complete boxed warning. reactions (e.g. stroke, transient ischemic attack). (5.2) • Neuroleptic Malignant Syndrome: Manage with immediate discontinuation of Elderly patients with dementia-related psychosis treated with antipsychotic drug and close monitoring. (5.3) drugs are -

Treatment of Adult Major Depressive Disorder (MDD) Tool
Section: A B C D E F G Resources References Treatment of Adult Major Depressive Disorder (MDD) Tool This tool is designed to support primary care providers in the treatment of adult patients (≥ 18 years) who have major depressive disorder (MDD). MDD is the most prevalent depressive disorder, and approximately 7% of Canadians meet the diagnostic criteria every year.1,2 The treatment of MDD involves psychotherapy and/or pharmacotherapy. Providers should work with patients to create a treatment plan together using providers’ clinical expertise and keeping in mind the patient’s preferences, as well as the practicality, feasibility, availability and affordability of treatment. TABLE OF CONTENTS pg. 1 Section A: Overview of MDD pathway pg. 6 Section E: Complementary and alternative medicine pg. 2 Section B: Assessing suicidality and managing pg. 7 Section F: Follow-up and monitoring suicide-related behaviour pg. 9 Section G: Special patient populations pg. 3 Section C: Psychotherapy options pg. 10 Resources pg.3 Section D: Pharmacotherapy management SECTION A: Overview of MDD pathway Patient has suspected depression Talking Points It is important to provide your patient with non-judgmental care (e.g. “Being Consider unexpected life events (e.g. death in the family, diagnosed with depression is nothing to be ashamed of, it is very common and change in family status, financial crisis). Consider special many adults are diagnosed with it every year”) patient populations. • Don’t use clinical/psychiatric language (e.g. “mental health,” “psychiatric,” and/or “maladaptive”) unless the patient uses these terms first • Use understandable language for cognitive distortions (e.g. -

Optimal Duration of Risperidone Or Olanzapine Adjunctive Therapy to Mood Stabilizer Following Remission of a Manic Episode: a CANMAT Randomized Double-Blind Trial
Molecular Psychiatry (2016) 21, 1050–1056 OPEN © 2016 Macmillan Publishers Limited All rights reserved 1359-4184/16 www.nature.com/mp ORIGINAL ARTICLE Optimal duration of risperidone or olanzapine adjunctive therapy to mood stabilizer following remission of a manic episode: A CANMAT randomized double-blind trial LN Yatham1, S Beaulieu2, A Schaffer3, M Kauer-Sant’Anna4, F Kapczinski4, B Lafer5, V Sharma6, SV Parikh7, A Daigneault8, H Qian9, DJ Bond1, PH Silverstone10, N Walji1, R Milev11, P Baruch12, A da Cunha13, J Quevedo14, R Dias5, M Kunz4, LT Young15, RW Lam1 and H Wong16 Atypical antipsychotic adjunctive therapy to lithium or valproate is effective in treating acute mania. Although continuation of atypical antipsychotic adjunctive therapy after mania remission reduces relapse of mood episodes, the optimal duration is unknown. As many atypical antipsychotics cause weight gain and metabolic syndrome, they should not be continued unless the benefits outweigh the risks. This 52-week double-blind placebo-controlled trial recruited patients with bipolar I disorder (n = 159) who recently remitted from a manic episode during treatment with risperidone or olanzapine adjunctive therapy to lithium or valproate. Patients were randomized to one of three conditions: discontinuation of risperidone or olanzapine and substitution with placebo at (i) entry (‘0-weeks’ group) or (ii) at 24 weeks after entry (‘24-weeks’ group) or (iii) continuation of risperidone or olanzapine for the full duration of the study (‘52-weeks’ group). The primary outcome measure was time to relapse of any mood episode. Compared with the 0-weeks group, the time to any mood episode was significantly longer in the 24-weeks group (hazard ratio (HR) 0.53; 95% confidence interval (CI): 0.33, 0.86) and nearly so in the 52-weeks group (HR: 0.63; 95% CI: 0.39, 1.02).