A Science Writer's Guide to Multiple Myeloma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Us 8530498 B1 3
USOO853 0498B1 (12) UnitedO States Patent (10) Patent No.: US 8,530,498 B1 Zeldis (45) Date of Patent: *Sep. 10, 2013 (54) METHODS FORTREATING MULTIPLE 5,639,476 A 6/1997 OShlack et al. MYELOMAWITH 5,674,533 A 10, 1997 Santus et al. 3-(4-AMINO-1-OXO-1,3-DIHYDROISOINDOL- 395 A 22 N. 2-YL)PIPERIDINE-2,6-DIONE 5,731,325 A 3/1998 Andrulis, Jr. et al. 5,733,566 A 3, 1998 Lewis (71) Applicant: Celgene Corporation, Summit, NJ (US) 5,798.368 A 8, 1998 Muller et al. 5,874.448 A 2f1999 Muller et al. (72) Inventor: Jerome B. Zeldis, Princeton, NJ (US) 5,877,200 A 3, 1999 Muller 5,929,117 A 7/1999 Muller et al. 5,955,476 A 9, 1999 Muller et al. (73) Assignee: Celgene Corporation, Summit, NJ (US) 6,020,358 A 2/2000 Muller et al. - 6,071,948 A 6/2000 D'Amato (*) Notice: Subject to any disclaimer, the term of this 6,114,355 A 9, 2000 D'Amato patent is extended or adjusted under 35 SS f 1939. All et al. U.S.C. 154(b) by 0 days. 6,235,756 B1 5/2001 D'Amatoreen et al. This patent is Subject to a terminal dis- 6,281.230 B1 8/2001 Muller et al. claimer 6,316,471 B1 1 1/2001 Muller et al. 6,326,388 B1 12/2001 Man et al. 6,335,349 B1 1/2002 Muller et al. (21) Appl. No.: 13/858,708 6,380.239 B1 4/2002 Muller et al. -

Cereblon and Its Downstream Substrates As Molecular Targets of Immunomodulatory Drugs
Int J Hematol (2016) 104:293–299 DOI 10.1007/s12185-016-2073-4 PROGRESS IN HEMATOLOGY Mechanisms of action of novel drugs in multiple myeloma and those responsible for the acquired resistance Cereblon and its downstream substrates as molecular targets of immunomodulatory drugs Takumi Ito1,2 · Hiroshi Handa1 Received: 15 June 2016 / Revised: 19 July 2016 / Accepted: 19 July 2016 / Published online: 26 July 2016 © The Japanese Society of Hematology 2016 Abstract Thalidomide was first developed as a sedative History of immunomodulatory drugs (IMiDs) around 60 years ago, but exhibited teratogenicity, leading to serious defects such as limb deformities. Nevertheless, Immunomodulatory drugs (IMiDs) are a new class of anti- thalidomide is now recognized as a therapeutic drug for the cancer drugs for which the parent molecule is thalidomide. treatment of Hansen’s disease and myeloma. Immunomod- Thalidomide (Fig. 1) was developed as a sedative in 1950s ulatory drugs (IMiDs), a new class of anti-cancer drug by the German pharmaceutical company Grunenthal. derived from thalidomide, have also been developed and Experiments using rodents initially suggested it to be safe exert potent anti-cancer effects. Although the molecular for use in humans, and the drug was sold over 40 countries, mechanism of thalidomide and IMiDs remained unclear for including Japan. However, as is widely known, thalidomide a long time, cereblon, a substrate receptor of the CRL4 E3 was found to have serious teratogenic effects. Use during ubiquitin ligase was identified as a primary direct target by pregnancy is associated with developmental defects of the a new affinity technique. A growing body of evidence sug- limbs and ears. -

Characterization of Ocular Adverse Events in Patients Receiving
Characterization of Ocular Adverse Events in Patients Receiving Belantamab Mafadotin for ≥12 Months: Post-Hoc Analysis of DREAMM-2 Study in Relapsed/Refractory Multiple Myeloma S. LONIAL1; A.K. NOOKA1; P. THULASI2; A.Z. BADROS3; B.H. JENG3; N.S. CALLANDER4; D. SBOROV5; B.E. ZAUGG6; R. POPAT7; S. DEGLI ESPOSTI8; J. BARON9; A. DOHERTY9; E. LEWIS10; J. OPALINSKA9; P. PAKA9; T. PIONTEK9; I. GUPTA9; A.V. FAROOQ11; A. JAKUBOWIAK11 | 1Emory University, Winship Cancer Institute, Atlanta, GA, USA; 2Emory Eye Center, Emory University, Atlanta, GA, USA; 3University of Maryland School of Medicine, Baltimore, MD, USA; 4University of Wisconsin, Carbone Cancer Center, Madison, WI, USA; 5Huntsman Cancer Institute, University of Utah, Salt Lake City, UT, USA; 6Moran Eye Center, University of Utah, Salt Lake City, UT, USA; 7University College London Hospitals, NHS Foundation Trust, London, UK; 8NIHR Biomedical Research Centre at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology, London, UK; 9GlaxoSmithKline, Collegeville, PA, USA; 10GlaxoSmithKline, Research Triangle Park, NC, USA; 11University of Chicago Medical Center, Chicago, IL, USA Dose delays and reductions related to ocular adverse events INTRODUCTION RESULTS All 14 patients required ≥2 dose delays, with dose reduction (to 1.92 mg/kg) in CONCLUSIONS Belantamab mafodotin (belamaf; GSK2857916) is a first-in-class, monomethyl auristatin F (MMAF)-containing 12 patients (86%). Demographics, efficacy, and overall safety information for patients treated with belamaf In this subset of 14 patients from the DREAMM-2 study, the median duration of response was antibody–drug conjugate (ADC) that binds to B-cell maturation antigen (BCMA) and eliminates multiple myeloma cells by for ≥12 months ● Patients experienced a mean of 3.6 dose delays over the ≥12 months of treatment a multimodal mechanism of action.1 (median: 3.5, range: 2–6). -

Overcoming the Immunosuppressive Tumor Microenvironment in Multiple Myeloma
cancers Review Overcoming the Immunosuppressive Tumor Microenvironment in Multiple Myeloma Fatih M. Uckun 1,2,3 1 Norris Comprehensive Cancer Center and Childrens Center for Cancer and Blood Diseases, University of Southern California Keck School of Medicine (USC KSOM), Los Angeles, CA 90027, USA; [email protected] 2 Department of Developmental Therapeutics, Immunology, and Integrative Medicine, Drug Discovery Institute, Ares Pharmaceuticals, St. Paul, MN 55110, USA 3 Reven Pharmaceuticals, Translational Oncology Program, Golden, CO 80401, USA Simple Summary: This article provides a comprehensive review of new and emerging treatment strategies against multiple myeloma that employ precision medicines and/or drugs capable of improving the ability of the immune system to prevent or slow down the progression of multiple myeloma. These rationally designed new treatment methods have the potential to change the therapeutic landscape in multiple myeloma and improve the long-term survival outcome. Abstract: SeverFigurel cellular elements of the bone marrow (BM) microenvironment in multiple myeloma (MM) patients contribute to the immune evasion, proliferation, and drug resistance of MM cells, including myeloid-derived suppressor cells (MDSCs), tumor-associated M2-like, “alter- natively activated” macrophages, CD38+ regulatory B-cells (Bregs), and regulatory T-cells (Tregs). These immunosuppressive elements in bidirectional and multi-directional crosstalk with each other inhibit both memory and cytotoxic effector T-cell populations as well as natural killer (NK) cells. Immunomodulatory imide drugs (IMiDs), protease inhibitors (PI), monoclonal antibodies (MoAb), Citation: Uckun, F.M. Overcoming the Immunosuppressive Tumor adoptive T-cell/NK cell therapy, and inhibitors of anti-apoptotic signaling pathways have emerged as Microenvironment in Multiple promising therapeutic platforms that can be employed in various combinations as part of a rationally Myeloma. -

Outcomes of Relapsed Or Refractory Acute Myeloid Leukemia After Frontline Hypomethylating Agent and Venetoclax Regimens
Haematologica HAEMATOL/2020/252569 Version 4 Outcomes of relapsed or refractory acute myeloid leukemia after frontline hypomethylating agent and venetoclax regimens Abhishek Maiti, Caitlin R. Rausch, Jorge E. Cortes, Naveen Pemmaraju, Naval G. Daver, Farhad Ravandi, Guillermo Garcia-Manero, Gautam Borthakur, Kiran Naqvi, Maro Ohanian, Nicholas J. Short, Yesid Alvarado, Tapan M. Kadia, Koichi Takahashi, Musa Yilmaz, Nitin Jain, Steven Kornblau, Guillermo Montalban Bravo, Koji Sasaki, Michael Andreeff, Prithiviraj Bose, Alessandra Ferrajoli, Ghayas C. Issa, Elias J. Jabbour, Lucia Masarova, Philip A. Thompson, Sa Wang, Sergej Konoplev, Sherry A. Pierce, Jing Ning, Wei Qiao, John S. Welch, Hagop M. Kantarjian, Courtney D. DiNardo, and Marina Y. Konopleva Disclosures: AM: Research funding from Celgene Corporation CRR: None JEC: Research funding from Ambit BioSciences, ARIAD, Arog, Astellas Pharma, AstraZeneca, Bristol-Myers Squibb, Celator, Celgene, Novartis, Pfizer, Sanofi, Sun Pharma, Teva; consultant for Ambit BioSciences, ARIAD, Astellas Pharma, BiolineRx, Bristol-Myers Squibb, Novartis; Pfizer. NP: Consulting/honorarium: Celgene; Stemline; Incyte; Novartis; MustangBio; Roche Diagnostics, LFB; Research funding/clinical trials support: Stemline; Novartis; Abbvie; Samus; Cellectis; Plexxikon; Daiichi-Sankyo; Affymetrix; Grants/funding: Affymetrix, SagerStrong Foundation NGD: Sunesis Pharmaceuticals, Inc.: Consultancy, Research Funding; Karyopharm: Consultancy, Research Funding; Immunogen: Research Funding; Pfizer Inc.: Consultancy, Research -
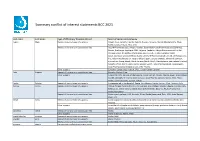
Summary Conflict of Interest Statements BCC 2021
Summary conflict of interest statements BCC 2021 Last name First name Type of affiliation/ financial interest Name of commercial company Aapro Matti Receipt of grants/research supports: Amgen, Eisai, Genomic Health, Helsinn, Hospira, Novartis, Merck, Mundipharma, Pfizer, Rache, Sandoz, Tesaro, Teva, Vifor Receipt of honoraria or consultation fees: Accord Pharmaceuticals, Amgen, Astellas, Bayer HealthCare Pharmaceuticals (Schering), Biocon, Boehringer Ingelheim, BMS, Celgene, Cephalon, Chugai Pharmaceutical Co. Ltd., Clinigen Group, Dr.Reddy's Laboratories, Eisai Co. Ltd., Eli Lilly, Genomic Health (Exact Sciences), GlaxoSmithKline (GSK), Glenmark Pharmaceuticals Limited, Gl Therapeutics, lnc., Helsinn Healthcare SA, Hospira (Pfizer), lpsen, Janssen Biotech, Johnson & Johnson, Kyowa Kirin Group, Merck, Merck Serono (Merck KGaA), Mundipharma International Limited, Novartis, Pfizer, Pierre Fabre, Rache, Sandoz, Sanofi, Taiho Pharmaceutical, Tesaro (GSK), Teva Pharmaceutical lndustries Ltd., Vifor Pharma Other support: European Cancer Organisation, SPCC, Cancer Center Genolier Aebi Stephan Receipt of honoraria or consultation fees: Novartis, Roche, Pfizer Other support: Support for CME lectures of the Lucerne Cancer Center: Amgen, Astellas, Bayer, Bristol-Myers Squibb, Debiopharm International SA, Eisai, Ipsen Pharma, Janssen, Merck, MSD, Pfizer, Roche, Sanofi Genzyme, Servier, Takeda André Fabrice Receipt of grants/research supports: Comepensated to the hospital: Roche, AstraZeneca, Daiichi Sankyo, Pfizer, Novartis, Lilly Barrios Carlos -

Watchdog Report for Celgene Corp
Celgene Corp. Watchdog Report ™ 10/4/2019 Celgene Corp. (CELG) Watchdog Report by Watchdog Research, Inc. CELG (NASDAQ Global) | CIK:816284 | United States Anticipating Gray Swan Events Sep 27, 2019 Jan 1, 2018 Jan 1, 2014 Key Facts RECENT PERIOD HISTORICAL PERIOD 10-Q led on Jul 30, 2019 for period ending Jun 2019 Business address: Summit, New Jersey, United States Industry: Pharmaceutical Preparation Manufacturing (NAICS 325412) Reporting Irregularities RECENT HISTORICAL SEC ler status: Large Accelerated Filer as of Jun 2019 Financial Restatements Index member: S&P 500, Russell 1000 Revisions Market Cap: $65.6b as of Jul 30, 2019 Annual revenue: $15.3b as of Dec 31, 2018 Out of Period Adjustments Corporate Governance Late Filings Impairments CEO: Mark Alles since 2016 CFO: David V. Elkins since 2018 Changes in Accounting Estimates 1st level Disclosure Controls Board Chairman: Mark Alles since 2018 Internal Controls Audit Committee Chair: James J. Loughlin 2nd level Critical / Key Audit Matters Auditor: KPMG LLP since 1986 Anomalies in the Numbers Outside Counsel (most recent): Quinn Emanuel Urquhart & Sullivan LLP RECENT HISTORICAL Saul Ewing Arnstein & Lehr LLP Benford's Law 3rd level Beneish M-Score SEC Reviewer: Sharon M Blume 4th level Accounting Disclosure Complexity Securities & Exchange Commission Concerns RECENT HISTORICAL SEC Letters to Management Revenue Recognition Non-GAAP Measures Lawsuits RECENT HISTORICAL Signicant Litigation Class Actions Watchdog Research, Inc., offers both individual and group subscriptions, Securities Law data feeds and/or custom company reports to our subscribers. Subscribe: We have delivered 300,000 public company reports to over External Pressures RECENT HISTORICAL 27,000 individuals, from over 9,000 investment rms and to 4,000+ public company corporate board members. -

Risk Stratification in Multiple Myeloma: Putting the Pieces Together Craig Reeder, MD Angela Mayo, MS, PA-C Mayo Clinic Financial Disclosure
Risk Stratification in Multiple Myeloma: Putting the Pieces Together Craig Reeder, MD Angela Mayo, MS, PA-C Mayo Clinic Financial Disclosure § Dr. Reeder has received research funding from Celgene, Millennium, and Novartis. § Ms. Mayo has received honoraria from Celgene, Millennium, and Novartis and has served on the Advanced Practice Provider Steering Committee for Celgene. Learning Objectives 1. Discuss agents for treatment of multiple myeloma (MM) and their side effects/management 2. Understand and discuss the heterogeneous genetic nature of MM 3. Learn the basic prognostic factors and how they impact treatment choices and outcomes 4. Understand the role of stem cell transplantation 5. Implement effective clinical strategies for minimizing toxicity 6. Utilize practical strategies for enhancing patients’ adherence to treatment Multiple Myeloma Statistics at a Glance Percentage of Estimated new Estimated deaths patients surviving cases (2015): (2015): 11,240 5 years: 46.6% 26,850 (2005–2011) Estimated number Percentage of all Percentage of all of people living cancer diagnoses: cancer deaths: with myeloma in 1.6% 1.9% US: 89,658 Siegel RL, et al. CA Cancer J Clin. 2015;65:5-29. Risk Factors for Multiple Myeloma Age (average age at diagnosis: 72) Male sex Monoclonal (58% vs. gammopathy 42%) African- Family American history race Most patients who are diagnosed have NO known risk factors! Siegel RL, et al. CA Cancer J Clin. 2015;65:5-29. Presenting Signs and Symptoms Patient-reported symptoms Objective findings § Fatigue § Anemia § Back/bone -

In the United States District Court for the District of New Jersey
Case 2:17-cv-07637-MCA-MAH Document 1 Filed 09/28/17 Page 1 of 102 PageID: 1 IN THE UNITED STATES DISTRICT COURT FOR THE DISTRICT OF NEW JERSEY New England Carpenters Health Benefits Fund, individually and on behalf of all others similarly situated, Civil Action No. ______________ Plaintiff CLASS ACTION COMPLAINT v. Celgene Corporation, JURY TRIAL DEMANDED Defendant CLASS ACTION COMPLAINT Plaintiff New England Carpenters Health Benefits Fund brings this class action on behalf of itself and all other similarly situated end-payors against Celgene Corporation (“Celgene”). Based on personal knowledge as to facts pertaining to it, and upon information and belief as to all other matters, Plaintiff alleges as follows: I. NATURE OF THE ACTION 1. This is a civil antitrust action seeking damages arising out of Celgene’s unlawful exclusion of competition from the market for thalidomide (“Thalomid”), which Celgene sells under the brand-name Thalomid, and lenalidomide (“Revlimid”), which Celgene sells under the brand-name Revlimid. 2. Celgene has sold Thalomid and Revlimid in capsule format, which are administered orally. Both drugs have dangerous side effects; namely, life- 1 Case 2:17-cv-07637-MCA-MAH Document 1 Filed 09/28/17 Page 2 of 102 PageID: 2 threatening birth defects when ingested by pregnant women. As a result, these drugs are highly regulated by the FDA. 3. Since 2006, Celgene has recorded more than $38.9 billion from the sale of Thalomid and Revlimid combined. A twenty-eight day supply of Thalomid could cost from between $8,000 to $10,000, and the same supply of Revlimid could cost approximately $15,000 to $20,000 in 2014. -

Pomalidomide Desensitization in a Patient Hypersensitive to Immunomodulating Agents
POMALIDOMIDE DESENSITIZATION, Seki et al. CASE REPORT Pomalidomide desensitization in a patient hypersensitive to immunomodulating agents † ‡ J.T. Seki PharmD,* N. Sakurai BSc MSc,* W. Lam BSc(Phm),* and D.E. Reece MD ABSTRACT Despite progressive treatments with tandem stem-cell transplantation, patients with incurable myeloma eventually succumb to relapsed or refractory disease if left untreated. Promising agents such as proteasome inhibitors and im- munomodulating imide drugs (imids), including the newer-generation agent pomalidomide, in combination with lower-dose dexamethasone, have been shown to be effective and to significantly improve and prolong survival in pretreated patients. Although the incidence of pomalidomide hypersensitivity reaction (hsr) in this class of drugs is not as well known, we have documented cutaneous toxicity (grade 3 by the Common Terminology Criteria for Adverse Events, version 4) in 2 separate cases (not yet published). Because the imids are chemically, structurally, and pharmacologi- cally similar, it is not unreasonable to consider possible cross-reactivity in pomalidomide recipients who developed hsr when receiving previous lines of imids. As a patient’s advocate, it is only prudent to provide a responsible, and yet practical, means to better address cross-sensitivity for patients. Intervention with the use of a rapid desensitization program (rdp) as a preventive measure should be introduced before initiating pomalidomide. Such a proactive measure for the patient’s safety will ensure a smooth transition into pomalidomide treatment. A hsr can be either related or non-related to immunoglobulin E. As imids become an essential treatment backbone for myeloma and other plasma-cell diseases, an increasing number of patients could experience skin and other life-threatening toxicities, resulting in unnecessary discontinuation of these life-prolonging agents. -

POMALYST Safely Capsules: 1 Mg, 2 Mg, 3 Mg, and 4 Mg (3) and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------- DOSAGE FORMS AND STRENGTHS ------------------------- These highlights do not include all the information needed to use POMALYST safely Capsules: 1 mg, 2 mg, 3 mg, and 4 mg (3) and effectively. See full prescribing information for POMALYST. -------------------------------- CONTRAINDICATIONS -------------------------------- POMALYST® (pomalidomide) capsules, for oral use Initial U.S. Approval: 2013 • Pregnancy (4.1) • Hypersensitivity (4.2) WARNING: EMBRYO-FETAL TOXICITY and VENOUS AND ARTERIAL --------------------------- WARNINGS AND PRECAUTIONS --------------------------- THROMBOEMBOLISM • Increased Mortality: Observed in patients with MM when pembrolizumab was added See full prescribing information for complete boxed warning to dexamethasone and a thalidomide analogue (5.4). EMBRYO-FETAL TOXICITY • Hematologic Toxicity: Neutropenia was the most frequently reported Grade 3/4 adverse • POMALYST is contraindicated in pregnancy. POMALYST is a thalidomide event. Monitor patients for hematologic toxicities, especially neutropenia (5.5). analogue. Thalidomide is a known human teratogen that causes severe • Hepatotoxicity: Hepatic failure including fatalities; monitor liver function tests monthly life-threatening birth defects (4, 5.1, 8.1). (5.6). • For females of reproductive potential: Exclude pregnancy before start of • Severe Cutaneous Reactions: Discontinue POMALYST (pomalidomide) for severe treatment. Prevent pregnancy during treatment by the use of 2 reliable reactions (5.7). -

Bluebird Bio and Celgene Corporation Present Initial Data From
bluebird bio and Celgene Corporation Present Initial Data from Ongoing Phase 1 Clinical Study of Next-Generation Anti-BCMA CAR T Cell Therapy bb21217 in Patients with Relapsed/Refractory Multiple Myeloma at ASH Annual Meeting bb21217 early safety profile consistent with CAR T platform therapies 83 percent objective response rate in 12 heavily pretreated multiple myeloma patients at first dose level studied Higher dose of bb21217 being assessed in the ongoing Phase 1 study CAMBRIDGE, Mass. and SUMMIT, N.J. – December 2, 2018 – bluebird bio, Inc. (Nasdaq: BLUE) and Celgene Corporation (NASDAQ: CELG) announced initial data from the ongoing Phase 1 clinical study of bb21217 (CRB-402), an investigational next-generation anti-BCMA CAR T cell therapy being studied in patients with relapsed/refractory multiple myeloma. The data were presented by Nina Shah, M.D., University of California, San Francisco, as an oral presentation at the 60th Annual Meeting of the American Society of Hematology (ASH). bb21217 is an investigational anti-BCMA CAR T cell therapy that uses the bb2121 chimeric antigen receptor (CAR) molecule with a manufacturing process designed to improve CAR T cell functional persistence. bb21217 has exhibited improved functional persistence and increased anti-tumor activity in preclinical animal studies. “Anti-BCMA CAR T therapy with bb2121 has shown clinical responses in a substantial proportion of patients with relapsed/refractory multiple myeloma. With the bb21217 program we are pursuing an approach intended to improve the in vivo persistence of functional CAR T cells with the hope that this provides a more durable benefit for patients,” said David Davidson, M.D., chief medical officer, bluebird bio.