Pomalidomide Desensitization in a Patient Hypersensitive to Immunomodulating Agents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Us 8530498 B1 3
USOO853 0498B1 (12) UnitedO States Patent (10) Patent No.: US 8,530,498 B1 Zeldis (45) Date of Patent: *Sep. 10, 2013 (54) METHODS FORTREATING MULTIPLE 5,639,476 A 6/1997 OShlack et al. MYELOMAWITH 5,674,533 A 10, 1997 Santus et al. 3-(4-AMINO-1-OXO-1,3-DIHYDROISOINDOL- 395 A 22 N. 2-YL)PIPERIDINE-2,6-DIONE 5,731,325 A 3/1998 Andrulis, Jr. et al. 5,733,566 A 3, 1998 Lewis (71) Applicant: Celgene Corporation, Summit, NJ (US) 5,798.368 A 8, 1998 Muller et al. 5,874.448 A 2f1999 Muller et al. (72) Inventor: Jerome B. Zeldis, Princeton, NJ (US) 5,877,200 A 3, 1999 Muller 5,929,117 A 7/1999 Muller et al. 5,955,476 A 9, 1999 Muller et al. (73) Assignee: Celgene Corporation, Summit, NJ (US) 6,020,358 A 2/2000 Muller et al. - 6,071,948 A 6/2000 D'Amato (*) Notice: Subject to any disclaimer, the term of this 6,114,355 A 9, 2000 D'Amato patent is extended or adjusted under 35 SS f 1939. All et al. U.S.C. 154(b) by 0 days. 6,235,756 B1 5/2001 D'Amatoreen et al. This patent is Subject to a terminal dis- 6,281.230 B1 8/2001 Muller et al. claimer 6,316,471 B1 1 1/2001 Muller et al. 6,326,388 B1 12/2001 Man et al. 6,335,349 B1 1/2002 Muller et al. (21) Appl. No.: 13/858,708 6,380.239 B1 4/2002 Muller et al. -

Cereblon and Its Downstream Substrates As Molecular Targets of Immunomodulatory Drugs
Int J Hematol (2016) 104:293–299 DOI 10.1007/s12185-016-2073-4 PROGRESS IN HEMATOLOGY Mechanisms of action of novel drugs in multiple myeloma and those responsible for the acquired resistance Cereblon and its downstream substrates as molecular targets of immunomodulatory drugs Takumi Ito1,2 · Hiroshi Handa1 Received: 15 June 2016 / Revised: 19 July 2016 / Accepted: 19 July 2016 / Published online: 26 July 2016 © The Japanese Society of Hematology 2016 Abstract Thalidomide was first developed as a sedative History of immunomodulatory drugs (IMiDs) around 60 years ago, but exhibited teratogenicity, leading to serious defects such as limb deformities. Nevertheless, Immunomodulatory drugs (IMiDs) are a new class of anti- thalidomide is now recognized as a therapeutic drug for the cancer drugs for which the parent molecule is thalidomide. treatment of Hansen’s disease and myeloma. Immunomod- Thalidomide (Fig. 1) was developed as a sedative in 1950s ulatory drugs (IMiDs), a new class of anti-cancer drug by the German pharmaceutical company Grunenthal. derived from thalidomide, have also been developed and Experiments using rodents initially suggested it to be safe exert potent anti-cancer effects. Although the molecular for use in humans, and the drug was sold over 40 countries, mechanism of thalidomide and IMiDs remained unclear for including Japan. However, as is widely known, thalidomide a long time, cereblon, a substrate receptor of the CRL4 E3 was found to have serious teratogenic effects. Use during ubiquitin ligase was identified as a primary direct target by pregnancy is associated with developmental defects of the a new affinity technique. A growing body of evidence sug- limbs and ears. -

Characterization of Ocular Adverse Events in Patients Receiving
Characterization of Ocular Adverse Events in Patients Receiving Belantamab Mafadotin for ≥12 Months: Post-Hoc Analysis of DREAMM-2 Study in Relapsed/Refractory Multiple Myeloma S. LONIAL1; A.K. NOOKA1; P. THULASI2; A.Z. BADROS3; B.H. JENG3; N.S. CALLANDER4; D. SBOROV5; B.E. ZAUGG6; R. POPAT7; S. DEGLI ESPOSTI8; J. BARON9; A. DOHERTY9; E. LEWIS10; J. OPALINSKA9; P. PAKA9; T. PIONTEK9; I. GUPTA9; A.V. FAROOQ11; A. JAKUBOWIAK11 | 1Emory University, Winship Cancer Institute, Atlanta, GA, USA; 2Emory Eye Center, Emory University, Atlanta, GA, USA; 3University of Maryland School of Medicine, Baltimore, MD, USA; 4University of Wisconsin, Carbone Cancer Center, Madison, WI, USA; 5Huntsman Cancer Institute, University of Utah, Salt Lake City, UT, USA; 6Moran Eye Center, University of Utah, Salt Lake City, UT, USA; 7University College London Hospitals, NHS Foundation Trust, London, UK; 8NIHR Biomedical Research Centre at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology, London, UK; 9GlaxoSmithKline, Collegeville, PA, USA; 10GlaxoSmithKline, Research Triangle Park, NC, USA; 11University of Chicago Medical Center, Chicago, IL, USA Dose delays and reductions related to ocular adverse events INTRODUCTION RESULTS All 14 patients required ≥2 dose delays, with dose reduction (to 1.92 mg/kg) in CONCLUSIONS Belantamab mafodotin (belamaf; GSK2857916) is a first-in-class, monomethyl auristatin F (MMAF)-containing 12 patients (86%). Demographics, efficacy, and overall safety information for patients treated with belamaf In this subset of 14 patients from the DREAMM-2 study, the median duration of response was antibody–drug conjugate (ADC) that binds to B-cell maturation antigen (BCMA) and eliminates multiple myeloma cells by for ≥12 months ● Patients experienced a mean of 3.6 dose delays over the ≥12 months of treatment a multimodal mechanism of action.1 (median: 3.5, range: 2–6). -

Overcoming the Immunosuppressive Tumor Microenvironment in Multiple Myeloma
cancers Review Overcoming the Immunosuppressive Tumor Microenvironment in Multiple Myeloma Fatih M. Uckun 1,2,3 1 Norris Comprehensive Cancer Center and Childrens Center for Cancer and Blood Diseases, University of Southern California Keck School of Medicine (USC KSOM), Los Angeles, CA 90027, USA; [email protected] 2 Department of Developmental Therapeutics, Immunology, and Integrative Medicine, Drug Discovery Institute, Ares Pharmaceuticals, St. Paul, MN 55110, USA 3 Reven Pharmaceuticals, Translational Oncology Program, Golden, CO 80401, USA Simple Summary: This article provides a comprehensive review of new and emerging treatment strategies against multiple myeloma that employ precision medicines and/or drugs capable of improving the ability of the immune system to prevent or slow down the progression of multiple myeloma. These rationally designed new treatment methods have the potential to change the therapeutic landscape in multiple myeloma and improve the long-term survival outcome. Abstract: SeverFigurel cellular elements of the bone marrow (BM) microenvironment in multiple myeloma (MM) patients contribute to the immune evasion, proliferation, and drug resistance of MM cells, including myeloid-derived suppressor cells (MDSCs), tumor-associated M2-like, “alter- natively activated” macrophages, CD38+ regulatory B-cells (Bregs), and regulatory T-cells (Tregs). These immunosuppressive elements in bidirectional and multi-directional crosstalk with each other inhibit both memory and cytotoxic effector T-cell populations as well as natural killer (NK) cells. Immunomodulatory imide drugs (IMiDs), protease inhibitors (PI), monoclonal antibodies (MoAb), Citation: Uckun, F.M. Overcoming the Immunosuppressive Tumor adoptive T-cell/NK cell therapy, and inhibitors of anti-apoptotic signaling pathways have emerged as Microenvironment in Multiple promising therapeutic platforms that can be employed in various combinations as part of a rationally Myeloma. -

COMPARISON of the WHO ATC CLASSIFICATION & Ephmra/Intellus Worldwide ANATOMICAL CLASSIFICATION
COMPARISON OF THE WHO ATC CLASSIFICATION & EphMRA/Intellus Worldwide ANATOMICAL CLASSIFICATION: VERSION June 2019 2 Comparison of the WHO ATC Classification and EphMRA / Intellus Worldwide Anatomical Classification The following booklet is designed to improve the understanding of the two classification systems. The development of the two systems had previously taken place separately. EphMRA and WHO are now working together to ensure that there is a convergence of the 2 systems rather than a divergence. In order to better understand the two classification systems, we should pay attention to the way in which substances/products are classified. WHO mainly classifies substances according to the therapeutic or pharmaceutical aspects and in one class only (particular formulations or strengths can be given separate codes, e.g. clonidine in C02A as antihypertensive agent, N02C as anti-migraine product and S01E as ophthalmic product). EphMRA classifies products, mainly according to their indications and use. Therefore, it is possible to find the same compound in several classes, depending on the product, e.g., NAPROXEN tablets can be classified in M1A (antirheumatic), N2B (analgesic) and G2C if indicated for gynaecological conditions only. The purposes of classification are also different: The main purpose of the WHO classification is for international drug utilisation research and for adverse drug reaction monitoring. This classification is recommended by the WHO for use in international drug utilisation research. The EphMRA/Intellus Worldwide classification has a primary objective to satisfy the marketing needs of the pharmaceutical companies. Therefore, a direct comparison is sometimes difficult due to the different nature and purpose of the two systems. -

Australian Pi – Pomalyst (Pomalidomide) Capsules
AUSTRALIAN PI – POMALYST (POMALIDOMIDE) CAPSULES Teratogenic effects: Pomalyst (pomalidomide) is a thalidomide analogue. Thalidomide is a known human teratogen that causes severe life-threatening human birth defects. If pomalidomide is taken during pregnancy, it may cause birth defects or death to an unborn baby. Women should be advised to avoid pregnancy whilst taking Pomalyst (pomalidomide), during dose interruptions, and for 4 weeks after stopping the medicine. 1 NAME OF THE MEDICINE Australian Approved Name: pomalidomide 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each 1 mg capsule contains 1 mg pomalidomide. Each 2 mg capsule contains 2 mg pomalidomide. Each 3 mg capsule contains 3 mg pomalidomide. Each 4 mg capsule contains 4 mg pomalidomide. For the full list of excipients, see Section 6.1. Description Pomalidomide is a yellow solid powder. It is practically insoluble in water over the pH range 1.2-6.8 and is slightly soluble (eg. acetone, methylene chloride) to practically insoluble (eg. heptanes, ethanol) in organic solvents. Pomalidomide has a chiral carbon atom and exists as a racemic mixture of the R(+) and S(-) enantiomers. 3 PHARMACEUTICAL FORM Pomalyst (pomalidomide) 1 mg capsules: dark blue/yellow size 4 gelatin capsules marked “POML” in white ink and “1 mg” in black ink. Each 1 mg capsule contains 1 mg of pomalidomide. Pomalyst (pomalidomide) 2 mg capsules: dark blue/orange size 2 gelatin capsules marked “POML 2 mg” in white ink. Each 2 mg capsule contains 2 mg of pomalidomide. Pomalyst (pomalidomide) 3 mg capsules: dark blue/green size 2 gelatin capsules marked “POML 3 mg” in white ink. -

Pomalidomide the POMALYST® Program
Pomalidomide The POMALYST® Program Overview Multiple myeloma is a type of cancer that begins in plasma cells in bone marrow. Plasma cells are white blood cells that make antibodies. The abnormal plasma cells build up in the bone marrow and sometimes in the solid part of the bone. Pomalidomide (brand name Pomalyst®) is approved to treat certain patients with multiple myeloma, but only under a restricted distribution program. Before you start taking this drug, you and your loved ones should read the important information in this brochure about the medication, side effects, and the rules you must follow if you choose pomalidomide, including the requirement to use birth control. Safety Pomalidomide is similar to the drug thalidomide and can cause the same life threatening birth defects. Both medications are approved by the Food and Drug Administration (FDA) to treat multiple myeloma within restricted distribution programs. For pomalidomide, the program is called Pomalyst REMS™ (Risk Evaluation and Mitigation Strategy). The program is in place to make sure that everyone is following the established safety guidelines. Only providers (doctors, nurse practitioners, etc.) and pharmacies certified by this program can write prescriptions for this medication or dispense it. To be considered for pomalidomide: • you must have already tried at least 2 other therapies, including lenalidomide and bortezomib • your disease must have progressed within 60 days of completing your last therapy • you must enroll in the Pomalyst REMS program and agree to comply with the program’s requirements (detailed in this brochure) Your healthcare provider will counsel you about the risks and benefits of this therapy. -
Australian Public Assessment Report for Apremilast
Australian Public Assessment Report for Apremilast Proprietary Product Name: Otezla Sponsor: Celgene Pty Ltd October 2015 Therapeutic Goods Administration About the Therapeutic Goods Administration (TGA) · The Therapeutic Goods Administration (TGA) is part of the Australian Government Department of Health and is responsible for regulating medicines and medical devices. · The TGA administers the Therapeutic Goods Act 1989 (the Act), applying a risk management approach designed to ensure therapeutic goods supplied in Australia meet acceptable standards of quality, safety and efficacy (performance), when necessary. · The work of the TGA is based on applying scientific and clinical expertise to decision- making, to ensure that the benefits to consumers outweigh any risks associated with the use of medicines and medical devices. · The TGA relies on the public, healthcare professionals and industry to report problems with medicines or medical devices. TGA investigates reports received by it to determine any necessary regulatory action. · To report a problem with a medicine or medical device, please see the information on the TGA website <https://www.tga.gov.au>. About AusPARs · An Australian Public Assessment Report (AusPAR) provides information about the evaluation of a prescription medicine and the considerations that led the TGA to approve or not approve a prescription medicine submission. · AusPARs are prepared and published by the TGA. · An AusPAR is prepared for submissions that relate to new chemical entities, generic medicines, major variations, and extensions of indications. · An AusPAR is a static document, in that it will provide information that relates to a submission at a particular point in time. · A new AusPAR will be developed to reflect changes to indications and/or major variations to a prescription medicine subject to evaluation by the TGA. -
Unsupported Price Increase Report
Unsupported Price Increase Report 2019 Assessment October 8, 2019 (Updated November 6, 2019) ©Institute for Clinical and Economic Review, 2019 Authors David M. Rind, MD, MSc Eric Borrelli, PharmD, MBA Chief Medical Officer Evidence Synthesis Intern Institute for Clinical and Economic Review Institute for Clinical and Economic Review Foluso Agboola, MBBS, MPH Steven D. Pearson, MD, MSc Director, Evidence Synthesis President Institute for Clinical and Economic Review Institute for Clinical and Economic Review Varun M. Kumar, MBBS, MPH, MSc (Former) Associate Director of Health Economics Institute for Clinical and Economic Review None of the above authors disclosed any conflicts of interest. DATE OF PUBLICATION: October 8, 2019 (Updated November 6, 2019) We would also like to thank Laura Cianciolo and Maria M. Lowe for their contributions to this report. ©Institute for Clinical and Economic Review, 2019 Page ii Unsupported Price Increase Report About ICER The Institute for Clinical and Economic Review (ICER) is an independent non-profit research organization that evaluates medical evidence and convenes public deliberative bodies to help stakeholders interpret and apply evidence to improve patient outcomes and control costs. Through all its work, ICER seeks to help create a future in which collaborative efforts to move evidence into action provide the foundation for a more effective, efficient, and just health care system. More information about ICER is available at http://www.icer-review.org. The funding for this report comes from the Laura and John Arnold Foundation. No funding for this work comes from health insurers, pharmacy benefit managers (PBMs), or life science companies. ICER receives approximately 21% of its overall revenue from these health industry organizations to run a separate Policy Summit program, with funding approximately equally split between insurers/PBMs and life science companies. -

Outcomes of Relapsed Or Refractory Acute Myeloid Leukemia After Frontline Hypomethylating Agent and Venetoclax Regimens
Haematologica HAEMATOL/2020/252569 Version 4 Outcomes of relapsed or refractory acute myeloid leukemia after frontline hypomethylating agent and venetoclax regimens Abhishek Maiti, Caitlin R. Rausch, Jorge E. Cortes, Naveen Pemmaraju, Naval G. Daver, Farhad Ravandi, Guillermo Garcia-Manero, Gautam Borthakur, Kiran Naqvi, Maro Ohanian, Nicholas J. Short, Yesid Alvarado, Tapan M. Kadia, Koichi Takahashi, Musa Yilmaz, Nitin Jain, Steven Kornblau, Guillermo Montalban Bravo, Koji Sasaki, Michael Andreeff, Prithiviraj Bose, Alessandra Ferrajoli, Ghayas C. Issa, Elias J. Jabbour, Lucia Masarova, Philip A. Thompson, Sa Wang, Sergej Konoplev, Sherry A. Pierce, Jing Ning, Wei Qiao, John S. Welch, Hagop M. Kantarjian, Courtney D. DiNardo, and Marina Y. Konopleva Disclosures: AM: Research funding from Celgene Corporation CRR: None JEC: Research funding from Ambit BioSciences, ARIAD, Arog, Astellas Pharma, AstraZeneca, Bristol-Myers Squibb, Celator, Celgene, Novartis, Pfizer, Sanofi, Sun Pharma, Teva; consultant for Ambit BioSciences, ARIAD, Astellas Pharma, BiolineRx, Bristol-Myers Squibb, Novartis; Pfizer. NP: Consulting/honorarium: Celgene; Stemline; Incyte; Novartis; MustangBio; Roche Diagnostics, LFB; Research funding/clinical trials support: Stemline; Novartis; Abbvie; Samus; Cellectis; Plexxikon; Daiichi-Sankyo; Affymetrix; Grants/funding: Affymetrix, SagerStrong Foundation NGD: Sunesis Pharmaceuticals, Inc.: Consultancy, Research Funding; Karyopharm: Consultancy, Research Funding; Immunogen: Research Funding; Pfizer Inc.: Consultancy, Research -
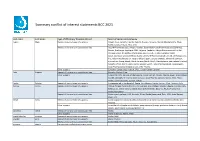
Summary Conflict of Interest Statements BCC 2021
Summary conflict of interest statements BCC 2021 Last name First name Type of affiliation/ financial interest Name of commercial company Aapro Matti Receipt of grants/research supports: Amgen, Eisai, Genomic Health, Helsinn, Hospira, Novartis, Merck, Mundipharma, Pfizer, Rache, Sandoz, Tesaro, Teva, Vifor Receipt of honoraria or consultation fees: Accord Pharmaceuticals, Amgen, Astellas, Bayer HealthCare Pharmaceuticals (Schering), Biocon, Boehringer Ingelheim, BMS, Celgene, Cephalon, Chugai Pharmaceutical Co. Ltd., Clinigen Group, Dr.Reddy's Laboratories, Eisai Co. Ltd., Eli Lilly, Genomic Health (Exact Sciences), GlaxoSmithKline (GSK), Glenmark Pharmaceuticals Limited, Gl Therapeutics, lnc., Helsinn Healthcare SA, Hospira (Pfizer), lpsen, Janssen Biotech, Johnson & Johnson, Kyowa Kirin Group, Merck, Merck Serono (Merck KGaA), Mundipharma International Limited, Novartis, Pfizer, Pierre Fabre, Rache, Sandoz, Sanofi, Taiho Pharmaceutical, Tesaro (GSK), Teva Pharmaceutical lndustries Ltd., Vifor Pharma Other support: European Cancer Organisation, SPCC, Cancer Center Genolier Aebi Stephan Receipt of honoraria or consultation fees: Novartis, Roche, Pfizer Other support: Support for CME lectures of the Lucerne Cancer Center: Amgen, Astellas, Bayer, Bristol-Myers Squibb, Debiopharm International SA, Eisai, Ipsen Pharma, Janssen, Merck, MSD, Pfizer, Roche, Sanofi Genzyme, Servier, Takeda André Fabrice Receipt of grants/research supports: Comepensated to the hospital: Roche, AstraZeneca, Daiichi Sankyo, Pfizer, Novartis, Lilly Barrios Carlos -

Samaritan Fund
Items supported by the Samaritan Fund (a) Non-drug Items supported by the Fund (b) Other items supported by the Samaritan Fund Mechanism (c) Self-financed Drugs supported by the Samaritan Fund (SF) and Community Care Fund (CCF) Medical Assistance Programme (First Phase Programme) (for specified self- financed cancer drugs) (a) Non-drug Items supported by the Fund 1. Percutaneous Transluminal Coronary Angioplasty (PTCA) and other consumables for interventional cardiology 2. Cardiac Pacemakers 3. Myoelectric Prosthesis 4. Custom-made Prosthesis 5. Appliances for prosthetic and orthotic services, physiotherapy and occupational therapy services (e.g. prosthesis) 6. Home use equipment and appliances (e.g. wheelchair, replacement of external speech processor for patients done with cochlear implant) 7. Gamma knife surgery 8. Harvesting of marrow in a foreign country for marrow transplant The Fund will only support the model which can meet the basic medical needs of the patients. (b) Other items supported by the Samaritan Fund Mechanism 1. Positron Emission Tomography (PET) service (c) Drugs supported by the Samaritan Fund The following specific self-financed drugs are supported by the Samaritan Fund: Item Drug Types of Clinical indications diseases 1 Abatacept Rheumatology Rheumatoid arthritis 2a Adalimumab Dermatology Severe psoriasis 2b Ophthalmology Non-infectious intermediate, posterior and panuveitis 2c Paediatric chronic non-infectious anterior uveitis 2d Rheumatology Ankylosing spondylitis 2e Juvenile idiopathic arthritis 2f Psoriatic