Handout Page 1 of 8
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vacutainer Tubes
Vacutainer Tube Guide - Order of Draw for routine volumes See separate guide for micro-tainers Number of Tube Inversions at Label Blood Collection Volume Tubes/Bottles Abbrev. Additive (Do Not Shake) General Laboratory Use Draw 1 Aerobic and 1 5 Blood Culture / requires Adapter 20 mL Anaerobic Culture Note: A separate venipuncture for trace BLCLT Bottles metal analysis is required if blood cultures are ordered at the same time. NAYYP Clot activator 8 Trace Element serum tube for Copper 6 mL Royal Trace Element whole blood for Aluminum, NAVYE 2 Call 2-5002 Blue K EDTA Lead, Zinc, Selenium, Manganese, Mercury, 8 for tubes Cadmium, Arsenic Discard tube or secondary sterile specimen 6 mL Clear None 0 tube 3 mL 2.7 mL Light (Blue) BLUE Sodium Citrate (3.2%) Coagulation Testing on Plasma Blue 3-4 1.8 mL (Blue/clear) Serum determinations where a gel-barrier is 6 mL Red RED Clot Activator 5 contraindicated; Therapeutic Drug 4 mL Monitoring (TDM) Clot Activator and gel SST - Serum determinations in Chemistry, Gold SST 5 5 mL for serum separation Immunology, Serology; HLA Ab screen, DSA Light Lithium heparin and PST PST - Plasma determinations in Chemistry 4.5 mL Green gel - plasma separation 8 GLI Lithium heparin 8 Whole Blood Plasma: Troponin, Lactic Acid, Ion. Ca+ 6 mL Dark 4 mL Green GNA Sodium heparin 8 Whole Blood Plasma: Tissue typing, plasma hemoglobin, plasma catecholamine, chromosome analysis Pink PINK Dry K2EDTA 8 Blood Bank / Transfusion; HLA Typing 6 mL Tan TAN K2EDTA 8 Lead Testing only 3 mL LAV 4 Whole Blood Hematology; some Flow, 4 mL Lavender Dry K2EDTA 8 Molecular, and Genetic tests; HIV Viral 2 mL LAV6 Load Whole Blood tube with Glycolytic inhibitor Potassium Oxalate / for GTT, Gray 6 mL GRAY Sodium fluoride 8 Post-Prandial Glucose, D-Xylose, and Volatiles panel ACDA ACD Whole Blood tube for Flow Yellow (Acid Citrate Dextrose 8 immunophenotyping; HLA cross matching; 8.5 mL ACDB Solution A) genetic and other referred tests ALWAYS Check Expiration Dates before use! If unsure of use, refer to the on-line “Lab User’s Guide” or call the lab at 25002 . -
Laboratory-General Specimen Collection and Handling Guidelines
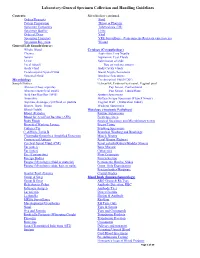
Laboratory-General Specimen Collection and Handling Guidelines Contents: Microbiology continued. Orders/Requests Stool Patient Preparation Throat or Pharynx Specimen Containers Tuberculosis (TB) Specimen Quality Urine Order of Draw Viral Specimen Transport VRE Surveillance (Vancomycin- Resistant entercoccus) Specimen Rejection Wound General Lab Sample/Source: Whole Blood Cytology (Cytopathology) Plasma Aspiration, Fine Needle Serum Aspiration, Cyst Fluids Urine Submission of slide Fecal (Stool) Tips on making smears Body Fluid Body Cavity Fluids Cerebrospinal Spinal Fluid Breast Nipple Secretions Synovial Fluid Brushing Specimens Microbiology Cerebrospinal Fluid (CSF) Sample/Source: Ectocervix, Endocervical canal, Vaginal pool Abscess (Deep aspirate) Pap Smear, Conventional Abscess (superficial swab) Pap Smear, Liquid Base Acid Fast Bacillus (AFB) Sputum Specimens Anaerobic Surface Scrape Specimen (Tzanck Smear) Aspirate, drainage, cyst fluid, or pustule Vaginal Wall (Maturation Index) Biopsy, Bone, Tissue Washing Specimens Blood (Adult) Histology (Anatomic Pathology) Blood )Pediatric Routine Submission Blood for Acid Fast Bacillus (AFB) Fresh Specimen Body Fluids Surgical Specimen and Microbiology test(s) Bronchial Washing Lavage Breast Tissue Catheter Tip Brushing Specimens C. difficile Toxin B Bronchial Washing and Brushings Chlamydia/Gonorrhea Amplified Detection Muscle Biopsy Crytococcal Antigen Renal Biopsy (Kidney) Cerebral Spinal Fluid (CSF) Renal calculi (Kidney/Bladder Stones) Ear (outer) Bone Marrow Ear (inner) Cytogenics Eye -

Research Article Comparison of Small-Volume Tubes and Vacuum
INTERNATIONAL JOURNAL OF MEDICAL BIOCHEMISTRY DOI: 10.14744/ijmb.2018.69188 Int J Med Biochem 2019;2(1):24-9 Research Article Comparison of small-volume tubes and vacuum blood tubes for complete blood count Kubranur Unal Department of Biochemistry, Polatlı Public Hospital, Ankara, Turkey Abstract Objectives: A complete blood count (CBC) is one of the most commonly requested clinical laboratory tests. Vacuum blood tubes are used routinely, and now, new small-volume tubes (SVTs) containing dipotassium ethylenediaminete- traacetic acid (K2EDTA) are also in use. The aim of this research was to compare SVTs with vacuum blood tubes for use in a CBC. Methods: Venous blood samples were taken from 40 healthy volunteers and were collected in BD Vacutainer (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) K2EDTA tubes and BD Microtainer (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) K2EDTA tubes. CBC parameters were analyzed using an ABX Pentra DF 120 device (Horiba, Ltd., Kyoto, Japan). Results: Red blood cells (RBC), hemoglobin (HGB), hematocrit (HCT), mean corpuscular hemoglobin (MCH), mean cor- puscular hemoglobin concentration (MCHC), and basophil (BASO) levels were found to be statistically significantly higher, while platelet (PLT) levels were determined to be statistically significantly lower in the SVT analyses compared with those of the vacuum blood tubes. When the percentage difference was compared with the total allowable error, RBC, HGB, HCT, MCH, MCHC, red cell distribution width, white blood cell count, neutrophil, lymphocyte, monocyte, eosinophil, and BASO values demonstrated a general trend of positive bias, while PLT values demonstrated a general trend of negative bias on a Bland-Altman bias plot. -

2017 LAB GUIDE TEST MENU March 2017Edition
2017 LAB GUIDE TEST MENU March 2017Edition Replaces: Sept 2015 Edition STAT TESTING MENU (2 Pages) 30 Minute In-Lab Turnaround Time (TAT) Unless Further Noted Below (In-Lab Time) MICROBIOLOGY 1. Spinal Fluid Culture set up and Gram Stain of sediment, India Ink prep 2. Gram Stain, other sites 3. Planting of cultures 4. Wet prep 5. Rapid Strep A Antigen Test (15 min. TAT) 6. Rapid Influenza A & B Antigen test 7. Rapid RSV Antigen test 8. Malaria Prep (60 min. TAT), Evening and Night shifts will only report “Parasites present or absent” 9. Screen, Gastric Urease, for Helicobacter Pylori (60 min. TAT) 10. Clostridium difficile DNA amplification (60 min. TAT) BLOOD BANK 1. Compatibility testing (leuko-reduced packed cells) 2. Type and Screen (60 min. TAT) 3. Cord Blood (2 hours) HEMATOLOGY 1. Complete Blood Count (CBC) SEE NOTE #1 2. Fibrinogen 3. Hemogram (ABC) 4. Monospot Test 5. Partial Thromboplastin Time (PTT) (60 min. TAT) 6. Prothrombin Time (PT) (60 min. TAT) 7. Fluid Cell Count (60 min. TAT) 8. Complete Urinalysis 9. D-dimer 10. Fluid pH CHEMISTRY 1. Arterial Blood Gases 2. Acetone 3. Ammonia 4. Amylase 5. Basic Metabolic Panel: Sodium, Potassium, Chloride, CO2, Creatinine, BUN, Glucose, and Calcium 6. Bilirubin (Total) 7. Blood Urea Nitrogen (BUN) 8. Calcium (Total and Ionized) 9. CPK (Total) (60 min. TAT for CPK total with MB fraction. CPKMB only run if CPK total > 113) UVM HEALTH NETWORK-CVPH 2 TEST MENU 10. Creatinine 11. CSF (Glucose and Protein) 12. Electrolytes: Sodium (Na), Potassium (K), Chloride (Cl), CO2 13. -

Phlebotomy Venipuncture Procedure PRINCIPLE: This Policy Establishes Criteria for the Correct Collection of Blood Specimens by Venipuncture
LTR9992 Phlebotomy Venipuncture Procedure PRINCIPLE: This policy establishes criteria for the correct collection of blood specimens by venipuncture. POLICY: By establishing a procedure for the correct collection of blood by venipuncture many pre- analytical errors and patient management complications can be avoided. Patient safety is the ultimate goal above all other considerations. Cost, efficiency, etc are secondary to ensuring that in no way will the patient be harmed by the phlebotomy procedure. This includes all aspects of the procedure including ordering, drawing, labeling, handling and transporting the specimen. The quality of the patient results is directly dependent upon the quality of the specimen. By providing the highest standard of safety and quality of care customer service satisfaction can be achieved. PROCEDURE: NOTE: Because it is often impossible to know what isolates or specimens might be infectious, all patient and laboratory specimens are treated as infectious and handled according to “Universal Precautions”. Needles and holders are not to be reused. They are to be properly discarded immediately after the phlebotomy procedure. All needles and syringes must be taken out of the original package in the patient’s presence. Never preassemble the vacutainer apparatus with a needle prior to use. Supplies for Venipuncture: Blood Collecting Trays- Blood collecting trays should be lightweight and easy to handle with enough space and compartments for the various supplies. Gloves- Disposable latex, vinyl, polyethylene, or nitrile gloves provide barrier protection. Needles and Holders- Needles and holders should be compatible with the tubes selected for use. Needles and winged blood collection sets are individually color-coded according to their respective gauge sizes. -

Blood Collection Tubes
Blood Collection Tubes MINIMUM SAMPLE VOLUMES The laboratory receives many requests to supply informa- The alphabetical test listing section of this manual tion regarding the minimum sample volumes for lab tests. details specific specimen requirements including storage Of particular concern are pediatric patients from whom temperature, special handling notes and whether testing excess blood collection must be avoided. is performed by HealthLab or a reference laboratory. We are unable to provide absolute minimum blood Storage temperature is specified as either room tempera- sample volumes for all tests because they require ture (18 o to 22o C), refrigerated (2o to 8o C) or frozen information regarding the patient’s hematocrit and/or the (-20o C or colder). More extensive instructions for combinations of tests that are to be collected. A combina- cytology, anatomic pathology, microbiology and tion of multiple tests may share the same dead-volume challenge test specimen collections are included in requirements on analytical equipment, which have to be following sections. factored into the requirements. Using the appropriate phlebotomy supplies is imperative MINIMUM VOLUMES FOR COMMON TESTS for accurate test results. Each vacutainer tube is color- coded to facilitate proper specimen collection. Please be The sample volumes listed below are recommended sure to use the proper tube for the desired test. sample test volumes and not necessarily the whole blood collection requirements. The sample volumes are the Color Codes for Vacutainer Tubes: minimum necessary to assure an accurate test result Color Contents on patients with normal hematocrits and include Lavender EDTA repeat testing. Blue Sodium citrate 3.2% CBC with Visual Differential Light Green Lithium heparin Collect whole blood to the third line on a purple Green Sodium heparin microtainer tube (0.5 ml). -

Exercise 2: Venipuncture Using Vacuum Collection System
EXERCISE 2: VENIPUNCTURE USING VACUUM COLLECTION SYSTEM Skills 30 points Objectives 1. Identify the routine site and three alternate sites for venipuncture. 2. List the three veins of the forearm used for venipuncture, describe where they are positioned, order of selection and the reason for the selection order. 3. Demonstrate concern for the safety and welfare of yourself and others by consistently using appropriate infection control techniques. 4. Demonstrate appropriate concern for your classmate by explaining the procedure. 5. State the importance and proper method for identifying patients in the hospital and out patient settings. 6. Describe and demonstrate the steps in the selection and preparation of the venipuncture site. 7. Describe the appearance of a properly applied tourniquet, maximum time it may be applied and the effects of tourniquet application and hand squeezing on the quality of the sample. 8. List and describe the equipment and supplies necessary for performance of the venipuncture. 9. Recognize proper needle insertion and withdrawal techniques including direction, angle, depth, aspiration and number of times the procedure may be attempted. 10. List, in chronological order, the correct steps in the proper performance of a venipuncture using the vacuum blood collection system 11. State the correct order of the draw. 12. State the reason that the correct order of the draw must be followed. 13. List ten stopper colors, additive present and laboratory tests which will be drawn into each. 14. State when, where and the minimum information which must be present for labeling blood samples. 15. List and describe problems which may be encountered during blood collection. -

BD Vacutainer® Venous Blood Collection
BD Vacutainer ® Venous Blood Collection Tube Guide ® For the full array of BD Vacutainer Blood Collection Tubes, visit www.bd.com/vacutainer. Many are available in a variety of sizes and draw volumes (for pediatric applications). Refer to our website for full descriptions. BD Vacutainer® Tubes BD Vacutainer® Tubes Inversions with with at Blood Your Lab’s BD Hemogard™ Closure Conventional Stopper Additive Collection* Laboratory Use Draw Volume/Remarks • Clot activator and gel 5 For serum determinations in chemistry. for serum separation May be used for routine blood donor Red/ screening and diagnostic testing of serum Gold Gray for infectious disease.** Tube inversions ensure mixing of clot activator with blood. Blood clotting time: 30 minutes. • Lithium heparin 8 For plasma determinations in chemistry. and gel for plasma Tube inversions ensure mixing of anticoagulant Light Green/ separation (heparin) with blood to prevent clotting. Green Gray • Silicone coated (glass) 0 For serum determinations in chemistry. • Clot activator, Silicone 5 May be used for routine blood donor screening and diagnostic testing of serum Red Red coated (plastic) for infectious disease.** Tube inversions ensure mixing of clot activator with blood. Blood clotting time: 60 minutes. • Thrombin 8 For stat serum determinations in chemistry. Tube inversions ensure mixing of clot activator Gray/ Orange (thrombin) with blood to activate clotting. Yellow • Clot activator 8 For trace-element, toxicology, and (plastic serum) nutritional-chemistry determinations. 8 Special stopper formulation provides • K2EDTA (plastic) Royal low levels of trace elements Blue (see package insert). Tube inversions ensure mixing of either clot activator or anticoagulant (EDTA) with blood. • Sodium heparin 8 For plasma determinations in chemistry. -

Venipuncture Blood Collection LABORATORY
Venipuncture Blood Collection LABORATORY Effective Date: 10/17 /2018 Revision Level:3 Page 1 of 15 Printed copies are for reference only. Please refer to the electronic copy for the current version. PURPOSE: The level of technology and monitored quality control programs for the laboratory are ineffective if the specimens collected for analysis are compromised in their integrity as a result of poor collection techniques or faulty identification. Proper specimen collections and specimen handling are critical since most errors occur in the preanalytical phases of testing. Pediatric specimen collection requires special training and skill. It is important to draw enough blood, but not too much. SCOPE: This document applies to the collection of specimens for testing performed at AnMed Health Laboratories or its reference laboratories. RESPONSIBILITY: Any individual collecting specimens to be processed by AnMed Health Laboratory Services. REFERENCES: 1. College of American pathologists, “So You’re Going to Collect a Blood Specimen”, 2013 2. Kathleen Becan-McBride, et al., Phlebotomy Handbook, 2010 3. The National Committee for Clinical Laboratory Standards. Document H3-A5, Procedures for the Collection of Diagnostic Blood Specimens by Venipuncture, Fifth Edition, Volume 23, Number 32, 2003. 4. Faber, Virginia, “Phlebotomy and the Aging Patient”, Advance for Medical Laboratory Professionals, December 21, 1998, pp.12-14. 5. Clinical Laboratory Standards Institute CLSI document H3-A6 Vol 27 #26 Procedures for the Collection of Diagnostic Blood Specimens by Venipuncture, Sixth Edition, Volume 27, Number 26, October 2007. 6. Clinical Laboratory Standards Institute, 5.3.1, GP41, 7 th edition. RELATED DOCUMENTS: Laboratory Patient Identification LABORATORY Therapeutic Drug Monitoring LABORATORY Registration and Order Entry DOE and ROE LABORATORY POLICY/PROCEDURE: SPECIMEN: Not applicable EQUIPMENT / MATERIALS / REAGENTS: 1. -

Complete Blood Count
Laboratory Procedure Manual Analyte: Complete Blood Count Matrix: Whole Blood Method: Complete Blood Count with 5-Part Differential Method No.: Revised: as performed by: Contact: September 2013 Important Information for Users CDC periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. 7-1 Complete Blood Count using HMX NHANES 2011-2012 Public Release Data Set Information This document details the Lab Protocol for testing the items listed in the following table: Lab Number Analyte SAS Label LBXWBCSI White blood cell count (1000 cells/uL) LBXLYPCT Lymphocyte (%) LBXMOPCT Monocyte (%) LBXNEPCT Segmented neutrophils (%) LBXEOPCT Eosinophils (%) LBXBAPCT Basophils (%) LBDLYMNO Lymphocyte number (1000 cells/uL) LBDMONO Monocyte number (1000 cells/uL) LBDNENO Segmented neutrophils number (1000 cells/uL) LBDEONO Eosinophils number (1000 cells/uL) CBC_G LBDBANO Basophils number (1000 cells/uL) LBXRBCSI Red cell count (million cells/uL) LBXHGB Hemoglobin (g/dL) LBXHCT Hematocrit (%) LBXMCVSI Mean cell volume (fL) LBXMCHSI Mean cell hemoglobin (pg) LBXMC MCHC (g/dL) LBXRDW Red cell distribution width (%) LBXPLTSI Platelet count ((1000 cells/uL)) LBXMPSI Mean platelet volume (fL) 2 Complete Blood Count using HMX NHANES 2011-2012 COMPLETE BLOOD COUNT (CBC) Perform a complete blood count (CBC) in duplicate on all survey participants age 1 and older. Perform the CBC on the Coulter® HMX. Run a CBC on the participant’s EDTA blood tubes. I. Purpose and Principle of Test CBC Analysis The Coulter method accurately counts and sizes cells by detecting and measuring changes in electrical resistance when a particle (such as a cell) in a conductive liquid passes through a small aperture. -

Venipuncture Procedure Using a Syringe
ROUTINE VENIPUNCTURE GUIDELINES MATERIALS 1. Safety Needles, 22g or less 2. Butterfly needles. 21g or less 3. Syringes 4. Vacutainer tube holder 5. Transfer Device 6. Blood Collection Tubes. The vacuum tubes are designed to draw a predetermined volume of blood. Tubes with different additives are used for collecting blood specimens for specific types of tests. The color of cap is used to identify these additives. 7. Tourniquets. Single use, disposable, latex-free tourniquets 8. Antiseptic. Individually packaged 70% isopropyl alcohol wipes. 9. 2x2 Gauze 10. Sharps Disposal Container. An OSHA acceptable, puncture proof container marked "Biohazardous". 11. Bandages or tape SAFETY 1. Observe universal (standard) safety precautions. 2. Observe all applicable isolation procedures. 3. PPE's will be worn at all times. 4. Wash hands in warm, running water with a appropriate hand washing product, 5. If hands are not visibly contaminated a commercial foaming hand wash product may be used before and after each patient collection. 6. Gloves are to be worn during all phlebotomies, and changed between patient collections. 7. Palpation of phlebotomy site may be performed without gloves providing the skin is not broken. 8. A lab coat or gown must be worn during blood collection procedures. 9. Needles and hubs are single use and are disposed of in an appropriate 'sharps' container as one unit. 10. Needles are never recapped, removed, broken, or bent after phlebotomy procedure. 11. Gloves are to be discarded in the appropriate container immediately after the phlebotomy procedure. 12. All other items used for the procedure must be disposed of according to proper biohazardous waste disposal policy. -

Blood Collection Tubes Effective Date: 4/13/2020
1507.P009.A4 Order of Draw – Blood Collection Tubes Effective Date: 4/13/2020 I. Purpose The procedure follows guidelines set forth by the Clinical and Laboratory Standards Institute™ (CLSI) to ensure quality specimens are collected for laboratory testing. A. According to CLSI guidelines, all phlebotomy procedures must be performed with the correct order of draw. B. All tubes must be gently inverted 8 – 10 times to provide thorough mixing of additives. C. Shaking the tube vigorously may cause hemolysis of the blood (separating of red blood cells). II. Order of Draw for Vacutainer Collection Tubes 1. Blood Culture Bottles – Used for bacterial and fungal cultures. Must be drawn first to reduce the potential hazard of bacterial, fungal, quantitative, CMV, and/or any other specimen contamination. a. Aerobic (Blue / Pink) bottle – Contains enriched Soybean – Casein digest broth medium capable of supporting the growth of aerobic organisms and resins for antibiotic neutralizations. b. Anaerobic (Purple) bottle – Contains Lytic Anaerobic medium designed to increase the detection and recovery of anaerobes. It contains a detergent to lyse red and white blood cells present in the sample, releasing any intracellular organisms. c. Yellow stopper Isolator tubes – Contain a nutrient solution d. Black stopper Isolator tubes – Contain a blood lysis solution 2. Blue Top – Tube contains Sodium Citrate. Most often used for coagulation studies. Must be drawn prior to collection of serum tubes to prevent contamination with clot activator and interference with coagulation cascade. a. When collecting the following Special Coagulation studies: Platelet Function Screen and Whole Blood Platelet Aggregation of Platelet Mapping, a discard of 1mL of blood must be drawn into a blue top citrate tube.