Blood Collection Tubes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Handout Page 1 of 8
MLT 112: Principles of Phlebotomy Learning Unit 3: Handout Specimen Collection – Venipuncture Procedure I. Collecting and Processing of Specimens A. Blood 1. Venipuncture Procedure (arm + dorsal/hand) – vacutainer, syringe, butterfly a. Approaching the Patient Correct patient identification Wash hands Have patient recite his/her name Wrist identification – mandatory must match requisition check ankle on babies and peds Out-patients – ask patient to spell name In-patients – see wrist ID Unconscious patient – see wrist ID Unidentified patient – emergency – use temporary I.D. band non-emergency – wait for I.D. Explanation and Reassurance – Inspire confidence Conversation Ensure that patient has complied with test requirements, such as fasting (only water), NPO (nothing per oral), etc. Check for any allergies, such as to latex, adhesive bandages, etc. b. Positions Positioning the patient Vein accessibility Sitting vs. lying down Phlebotomist position – always in front in case of fainting. c. Applying the Tourniquet See previous lecture Page 1 of 8 MLT 112: Principles of Phlebotomy Learning Unit 3: Handout d. Veins Used - Antecubital Fossa Cephalic Median Cephalic Median Basilic Median Cubital Vein – vein of choice, anchored best Other Structures – avoid Brachial artery – apply pressure 5 minutes Cutaneous nerve – very painful Tendon for the biceps muscle – always draw below crease e. Other Vein Sites Wrist (never palm side) Hand Ankle Foot f. Preparing Equipment Syringes Assembly – always work plunger before procedure. Plunger position – must -

Vacutainer Tubes
Vacutainer Tube Guide - Order of Draw for routine volumes See separate guide for micro-tainers Number of Tube Inversions at Label Blood Collection Volume Tubes/Bottles Abbrev. Additive (Do Not Shake) General Laboratory Use Draw 1 Aerobic and 1 5 Blood Culture / requires Adapter 20 mL Anaerobic Culture Note: A separate venipuncture for trace BLCLT Bottles metal analysis is required if blood cultures are ordered at the same time. NAYYP Clot activator 8 Trace Element serum tube for Copper 6 mL Royal Trace Element whole blood for Aluminum, NAVYE 2 Call 2-5002 Blue K EDTA Lead, Zinc, Selenium, Manganese, Mercury, 8 for tubes Cadmium, Arsenic Discard tube or secondary sterile specimen 6 mL Clear None 0 tube 3 mL 2.7 mL Light (Blue) BLUE Sodium Citrate (3.2%) Coagulation Testing on Plasma Blue 3-4 1.8 mL (Blue/clear) Serum determinations where a gel-barrier is 6 mL Red RED Clot Activator 5 contraindicated; Therapeutic Drug 4 mL Monitoring (TDM) Clot Activator and gel SST - Serum determinations in Chemistry, Gold SST 5 5 mL for serum separation Immunology, Serology; HLA Ab screen, DSA Light Lithium heparin and PST PST - Plasma determinations in Chemistry 4.5 mL Green gel - plasma separation 8 GLI Lithium heparin 8 Whole Blood Plasma: Troponin, Lactic Acid, Ion. Ca+ 6 mL Dark 4 mL Green GNA Sodium heparin 8 Whole Blood Plasma: Tissue typing, plasma hemoglobin, plasma catecholamine, chromosome analysis Pink PINK Dry K2EDTA 8 Blood Bank / Transfusion; HLA Typing 6 mL Tan TAN K2EDTA 8 Lead Testing only 3 mL LAV 4 Whole Blood Hematology; some Flow, 4 mL Lavender Dry K2EDTA 8 Molecular, and Genetic tests; HIV Viral 2 mL LAV6 Load Whole Blood tube with Glycolytic inhibitor Potassium Oxalate / for GTT, Gray 6 mL GRAY Sodium fluoride 8 Post-Prandial Glucose, D-Xylose, and Volatiles panel ACDA ACD Whole Blood tube for Flow Yellow (Acid Citrate Dextrose 8 immunophenotyping; HLA cross matching; 8.5 mL ACDB Solution A) genetic and other referred tests ALWAYS Check Expiration Dates before use! If unsure of use, refer to the on-line “Lab User’s Guide” or call the lab at 25002 . -

Coagulation Testing: High Hematocrit-Anticoagulant Adjustment
PREANALYTIC PULSE Coagulation Testing: High Hematocrit-Anticoagulant Adjustment In 1980, CLSI released H21-A4 guidelines for coagulation testing, which included the recommendation to adjust/correct the amount of citrate in blue-top evacuated blood collection tubes for patients presenting hematocrits greater than 55%. In addition to the CLSI guidelines, the CAP hematology checklist HEM.22830 includes the question, “Are there documented guidelines for the detection and special handling of specimens with elevated hematocrits?” Principle The adjustment is to assure the plasma:anticoagulant ratio (not the blood:anticoagulant ratio) stays consistent. A patient with high hematocrit, greater than 55%, will result in less plasma after centrifugation. The plasma fraction will contain an increased concentration of sodium citrate anticoagulant. The increased concentration may result in falsely prolonged test results for Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT). Formula 1. To calculate the corrected 3.2% sodium citrated whole blood for hematocrit > 55%, adjust the citrate to the proper volume with the following formula: -3 C = (1.85 x 10 )(100-HCT)(Vblood) Where: C = volume of sodium citrate required for that volume of blood HCT = patient’s hematocrit V = volume of blood required in the blood collection tube (example if a 3mL tube is used the blood draw volume is 2.7mL) 1.85 x 10-3 is a constant (considering the citrate volume, blood volume, and citrate concentration). 2. Example: Patient has a Hct of 60% and the patient’s blood will be drawn into a 3mL VACUETTE® sodium citrate (blue-top) blood collection tube. Adjustment of the sodium citrate volume is calculated as: C = (1.85 x 10-3)(100-60)(2.7mL) C = 0.20mL (rounded up from 01.998mL) Remove: 0.30 - 0.20 = 0.10mL of sodium citrate to be removed (0.30 is the difference between the total tube volume of 3.0mL and the blood drawn into the tube of 2.7mL) Method The instructions to prepare an adjusted sodium citrate tube are to be documented in the Laboratory Standard Operating Procedures. -
Role of Real-Time / Accurate Diagnostic Testing in Patient Blood Management Programs
ROLE OF REAL-TIME / ACCURATE DIAGNOSTIC TESTING IN PATIENT BLOOD MANAGEMENT PROGRAMS POINT-OF-CARE TESTING “Diagnostic testing is an essential component of Patient Blood Management. The accurate assessment of the true causes of bleeding dysfunction facilitates the employment of evidence based, goal directed therapy to rapidly prevent and treat excess blood loss. “ Sherri Ozawa RN, Clinical Director, Institute of Patient Blood Management, Englewood Hospital Medical Center, Englewood, New Jersey. PATIENT BLOOD MANAGEMENT Interdisciplinary Managing Blood Conservation Anemia Modalities “The timely application of evidence based medical and surgical concepts designed to manage IMPROVED anemia, optimize hemostasis, and PATIENT minimize blood loss in order to OUTCOMES improve patient outcomes.” SABM© 2018 - Society for the Advancement of Blood Management (SABM.org) Optimizing Patient-Centered Coagulation Decision Making Point-of-care testing forms an integral part of PBM, enabling accurate and real-time diagnosis of anemia and bleeding and facilitating precise and targeted hemostatic intervention. 1 Conventional coagulation tests are unable to provide needed information on actual bleeding risk/defects 1, thus delaying appropriate and targeted treatment. Slow turnaround times for laboratory-based conventional coagulation tests are one of the major drivers of empirical treatment regimens, which inevitably result in some patients receiving unnecessary, inappropriate and avoidable transfusions, with associated increased morbidity and mortality, and -
Global Assays of Hemostasis in the Diagnostics of Hypercoagulation and Evaluation of Thrombosis Risk Elena N Lipets1 and Fazoil I Ataullakhanov1,2,3,4,5,6*
Lipets and Ataullakhanov Thrombosis Journal (2015) 13:4 DOI 10.1186/s12959-015-0038-0 REVIEW Open Access Global assays of hemostasis in the diagnostics of hypercoagulation and evaluation of thrombosis risk Elena N Lipets1 and Fazoil I Ataullakhanov1,2,3,4,5,6* Abstract Thrombosis is a deadly malfunctioning of the hemostatic system occurring in numerous conditions and states, from surgery and pregnancy to cancer, sepsis and infarction. Despite availability of antithrombotic agents and vast clinical experience justifying their use, thrombosis is still responsible for a lion’s share of mortality and morbidity in the modern world. One of the key reasons behind this is notorious insensitivity of traditional coagulation assays to hypercoagulation and their inability to evaluate thrombotic risks; specific molecular markers are more successful but suffer from numerous disadvantages. A possible solution is proposed by use of global, or integral, assays that aim to mimic and reflect the major physiological aspects of hemostasis process in vitro. Here we review the existing evidence regarding the ability of both established and novel global assays (thrombin generation, thrombelastography, thrombodynamics, flow perfusion chambers) to evaluate thrombotic risk in specific disorders. The biochemical nature of this risk and its detectability by analysis of blood state in principle are also discussed. We conclude that existing global assays have a potential to be an important tool of hypercoagulation diagnostics. However, their lack of standardization currently impedes their application: different assays and different modifications of each assay vary in their sensitivity and specificity for each specific pathology. In addition, it remains to be seen how their sensitivity to hypercoagulation (even when they can reliably detect groups with different risk of thrombosis) can be used for clinical decisions: the risk difference between such groups is statistically significant, but not large. -

64Th Annual SSC Meeting, in Conjunction with the 2018 ISTH Congress in Dublin, Ireland Meeting Minutes Standing Committees Coagulation Standards Committee
64th Annual SSC meeting, in conjunction with the 2018 ISTH Congress in Dublin, Ireland Meeting Minutes Standing Committees Coagulation Standards Committee............................................................... 3 Subcommittees Animal, Cellular and Molecular Models ........................................................ 6 Biorheology .................................................................................................. 9 Control of Anticoagulation ............................................................................ 15 Disseminated Intravascular Coagulation ...................................................... 20 Factor VIII, Factor IX and Rare Coagulation Disorders ................................ 23 Factor XI and the Contact System ............................................................... 27 Factor XIII and Fibrinogen ............................................................................ 30 Fibrinolysis ................................................................................................... 34 Genomics in Thrombosis and Hemostasis ................................................... 38 Hemostasis and Malignancy ........................................................................ 47 Lupus Anticoagulant/Phospholipid Dependent Antibodies ........................... 51 Pediatric and Neonatal Hemostasis and Thrombosis ................................... 57 Perioperative and Critical Care Thrombosis and Hemostasis ...................... 66 Plasma Coagulation Inhibitors ..................................................................... -

Pre-Analytical Variables in the Coagulation Lab: Why Does It Matter?
Generate Knowledge Pre-Analytical Variables in the Coagulation Lab: Why Does It Matter? Paul Riley, PhD, MBA Pre-Analytical Variables: Objectives 1. Define Pre-Analytical variables 2. Explain how blood collection may impact test results 3. Describe best practices for sample transport and storage 4. Review sample processing procedures 5. Identify patient variables that may affect coagulation testing What are Pre-Analytical Variables? Includes everything that may affect a patient specimen from the clinician ordering the test to the point of analysis Some patient variables are out of the lab’s control (medications, lipemia, icterus, etc.) The biggest source of laboratory error - far exceeds analytical error Scope? Up to 70% of testing errors occur in the pre-analytical phase1 It is not always clear when a sample is received in the lab that it may be unsuitable or compromised Lab results lead to clinical action 70-80% of all clinical decisions regarding patient care are based on lab results Coag samples are especially susceptible Sample collection initiates clotting PT and PTT are complex enzymatic reactions 1. Plebani M: Quality indicators to detect pre-analytical errors in Laboratory testing. Clin Biochem Rev 2012; 33:85-88 Scope? What are the ramifications of pre-analytical errors for the patient? Misdiagnosis Inappropriate treatment Diligence is required on the part of the laboratory to prevent incorrect results Must have quality indicators in place to monitor the steps of the pre- analytical phase Event management where errors are investigated and corrected so that repeat events are prevented Scope? When a sample is compromised: • the test result may reflect the status of the sample • but not reflect the clinical status of the patient Guidelines In order to improve the quality of patients results, sample collection and handling should follow the CLSI guideline H21-A5; 2008 Test Ordering Is the right test ordered on the right patient? Coag is confusing - Names sound alike! Factor X vs. -
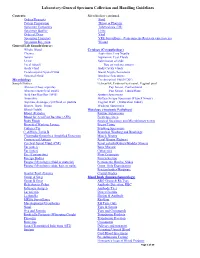
Laboratory-General Specimen Collection and Handling Guidelines
Laboratory-General Specimen Collection and Handling Guidelines Contents: Microbiology continued. Orders/Requests Stool Patient Preparation Throat or Pharynx Specimen Containers Tuberculosis (TB) Specimen Quality Urine Order of Draw Viral Specimen Transport VRE Surveillance (Vancomycin- Resistant entercoccus) Specimen Rejection Wound General Lab Sample/Source: Whole Blood Cytology (Cytopathology) Plasma Aspiration, Fine Needle Serum Aspiration, Cyst Fluids Urine Submission of slide Fecal (Stool) Tips on making smears Body Fluid Body Cavity Fluids Cerebrospinal Spinal Fluid Breast Nipple Secretions Synovial Fluid Brushing Specimens Microbiology Cerebrospinal Fluid (CSF) Sample/Source: Ectocervix, Endocervical canal, Vaginal pool Abscess (Deep aspirate) Pap Smear, Conventional Abscess (superficial swab) Pap Smear, Liquid Base Acid Fast Bacillus (AFB) Sputum Specimens Anaerobic Surface Scrape Specimen (Tzanck Smear) Aspirate, drainage, cyst fluid, or pustule Vaginal Wall (Maturation Index) Biopsy, Bone, Tissue Washing Specimens Blood (Adult) Histology (Anatomic Pathology) Blood )Pediatric Routine Submission Blood for Acid Fast Bacillus (AFB) Fresh Specimen Body Fluids Surgical Specimen and Microbiology test(s) Bronchial Washing Lavage Breast Tissue Catheter Tip Brushing Specimens C. difficile Toxin B Bronchial Washing and Brushings Chlamydia/Gonorrhea Amplified Detection Muscle Biopsy Crytococcal Antigen Renal Biopsy (Kidney) Cerebral Spinal Fluid (CSF) Renal calculi (Kidney/Bladder Stones) Ear (outer) Bone Marrow Ear (inner) Cytogenics Eye -

Point of Care Coagulation Testing
POINT OF CARE COAGULATION TESTING Dr Danny Morland Royal Victoria Infirmary Newcastle upon Tyne 11 th October 2016 Introduction Declarations of Interest: None CONTENT Introduction to POCT Principles Interpretation Treatment Literature NUTH Experience Point Of Care Testing (POCT) Medical diagnostic testing at (or near) the point of care. POCT PROS CONS • Quick • Cost (potentially) • Convenient • Quality • Reliable • Training • Efficient • Workload • Recording • Risk of inappropriate decision-making Point of Care Coagulation Testing (POCCT) Viscoelastic properties of whole blood clot Thromboelastography = Thromboelastometry (TEG) (ROTEM) Purported Benefits over Standard Tests • Measures whole blood, not just plasma • Looks at clot generation and propagation beyond the point of clot appearance • Allows comment on clot ‘quality’ • Can identify fibrinolysis FAST –potential information on clotting status within 5mins of test starting POCCT vs Standard Lab Tests POCCT LAB • Whole blood • Highly standardised • Clot beyond first • Trained, professional staff appearance • Quality control • Clot quality • Well established • Identify fibrinolysis • Complete picture • FAST • Cost PRINCIPLES Viscoelasticity Hardware OUTPUTS Panel Testing – Normal results INTERPRETATION Normal Low Platelets Normal Hypo-fibrinogenaemia Heparin Effect Normal TREATMENT LIMITATIONS AND WARNINGS • Treatment should be administered according to the clinical picture (e.g. volume & current rate of blood loss) • Viscoelastic devices are not uniformly sensitive to all disturbances -

PDF Download
364 Review Article Can We Measure the Individual Prothrombotic or Prohemorrhagic Tendency by Global Coagulation Tests? Ã Ã Sara Reda1, Laure Morimont2,3, Jonathan Douxfils2,3 Heiko Rühl1 1 Institute of Experimental Hematology and Transfusion Medicine, Address for correspondence Heiko Rühl, MD, Institute of University of Bonn, Bonn, Germany Experimental Hematology and Transfusion Medicine, University of 2 Department of Pharmacy, Namur Thrombosis and Hemostasis Bonn, Venusberg-Campus 1, 53127 Bonn, Germany Center,UniversityofNamur,Namur,Belgium (e-mail: [email protected]). 3 Qualiblood s.a., Namur, Belgium Hämostaseologie 2020;40:364–378. Abstract Hemostasis is a complex process in which abnormalities can cause shifts toward prothrombotic or prohemorrhagic states resulting in thrombosis or bleeding, respec- tively. Several coagulation tests may be required to characterize these defects but may yet not always reflect a patient’s true hemostatic capacity. Thus, global coagulation tests aiming to simulate the coagulation process in vitro instead of measuring single components thereof are certainly of interest to assess prothrombotic or prohemor- rhagic tendencies. This review describes the development and application of global Keywords coagulation tests, concentrating on the more widely used methods of viscoelastometry ► global coagulation and thrombin generation. A focus is placed on conditions characterized by simulta- tests neous changes of various components of hemostasis, such as anticoagulant therapy or ► hypercoagulability hormone-induced coagulopathy, in which global coagulation tests are especially ► bleeding promising. If the key challenges of standardization and automation of these tests ► anticoagulant drugs are solved, as is the case with automated thrombogram or clot waveform analysis, ► hormone-induced global coagulation assays will play an important role in the future of laboratory coagulopathy diagnostics of hemostasis and thrombosis. -

Five-Minute Preparation of Platelet-Poor Plasma for Routine Coagulation Testing A
املجلة الصحية لرشق املتوسط املجلد السادس عرش العدد الثاين Five-minute preparation of platelet-poor plasma for routine coagulation testing A. Sultan1 إعداد يستغرق 5دقائق للبﻻزما الفقرية بالصفيحات من أجل اﻻختبار الروتيني للتخثر أمحد حسن سلطان تتطلب اخلﻻصـة:الدﻻئل اﻹرشادية ملؤسسة املعايري اﻹكلينيكية ومعايري املختربات أن جترى اﻻختبارات الروتينية للتخثر ببﻻزما فقرية بالصفيحات )أقل من 000 10 صفيحة/مكرولرت(، وحترض من كامل الدم املضاف إليه السرتات وجرى تنبيذه برسعة منخفضة ملدة 10 – 30 دقيقة. وملقارنة النتائج التي تم احلصول عليها من البﻻزما التي خضعت للتنبيذ ملدة 5دقائق برسعة 3000جاذبية أو ملدة 10 دقائق برسعة 2000 جاذبية، أجريت مقايسة شملت 46عينة مأخوذة من بالغني أصحاء أسوياء بقصد التعرف عىل زمن الربوثرومني، وزمن الثرومبوبﻻستني اجلزئي املفعّل لواملعدَّ الدويل املسوَّ ى. ﻻ يوجد اختﻻفات يعتد هبا يف نتائج اﻻختبار، ُواستنتج ِأن النبذ ملدة مخس دقائق بمقدار g 3000يعترب ًاختيارا ًموثوقا فيه ًومفيدا للحد من الوقت املستغرق يف هذه اﻻختبارات. ABSTRACT Clinical and Laboratory Standard Institute guidelines require that routine coagulation tests are performed with platelet-poor plasma (< 10 000 platelets/µL) and prepared from whole citrated blood centrifuged at low speed for 10–30 minutes. To compare results obtained from plasma centrifuged for 5 minutes at 3000 g or for 10 minutes at 2000 g, 46 blood samples from normal healthy adults were assayed for prothrombin time, international normalized ratio and activated partial thromboplastin time. No significant differences were found in test results and it was concluded that 5 minutes centrifugation at 3000 g is a reliable and useful option to reduce the turnaround time for these tests. Préparation en cinq minutes d’un plasma pauvre en plaquettes pour les tests d’hémostase de routine RÉSUMÉ Les recommandations du CLSI (Clinical and Laboratory Standard Institute) imposent que les tests d’hémostase soient réalisés avec du plasma pauvre en plaquettes (< 10 000 plaquettes/µL) et préparés à partir de sang total citraté, centrifugé à vitesse lente pendant 10 à 30 minutes. -

Research Article Comparison of Small-Volume Tubes and Vacuum
INTERNATIONAL JOURNAL OF MEDICAL BIOCHEMISTRY DOI: 10.14744/ijmb.2018.69188 Int J Med Biochem 2019;2(1):24-9 Research Article Comparison of small-volume tubes and vacuum blood tubes for complete blood count Kubranur Unal Department of Biochemistry, Polatlı Public Hospital, Ankara, Turkey Abstract Objectives: A complete blood count (CBC) is one of the most commonly requested clinical laboratory tests. Vacuum blood tubes are used routinely, and now, new small-volume tubes (SVTs) containing dipotassium ethylenediaminete- traacetic acid (K2EDTA) are also in use. The aim of this research was to compare SVTs with vacuum blood tubes for use in a CBC. Methods: Venous blood samples were taken from 40 healthy volunteers and were collected in BD Vacutainer (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) K2EDTA tubes and BD Microtainer (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) K2EDTA tubes. CBC parameters were analyzed using an ABX Pentra DF 120 device (Horiba, Ltd., Kyoto, Japan). Results: Red blood cells (RBC), hemoglobin (HGB), hematocrit (HCT), mean corpuscular hemoglobin (MCH), mean cor- puscular hemoglobin concentration (MCHC), and basophil (BASO) levels were found to be statistically significantly higher, while platelet (PLT) levels were determined to be statistically significantly lower in the SVT analyses compared with those of the vacuum blood tubes. When the percentage difference was compared with the total allowable error, RBC, HGB, HCT, MCH, MCHC, red cell distribution width, white blood cell count, neutrophil, lymphocyte, monocyte, eosinophil, and BASO values demonstrated a general trend of positive bias, while PLT values demonstrated a general trend of negative bias on a Bland-Altman bias plot.