Caring for the Working Artist
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Actors Rhea Perlman, Kevin Sorbo Headline Lights on Afterschool!
NEWS RELEASE CONTACT: Gretchen Wright October 12, 2005 202/371-1999 Actors Rhea Perlman, Kevin Sorbo Headline Lights On Afterschool! As afterschool programs nationwide gear up for the nation’s largest rally for afterschool, award-winning actress Rhea Perlman is preparing to reprise her role as national spokesperson for Lights On Afterschool, and actor Kevin Sorbo is joining Lights On events in Los Angeles and Washington, DC. Perlman is best known for her role as Carla on the long-running television show “Cheers;” she also volunteers with LA’s BEST, an afterschool program in Los Angeles. Sorbo is a spokesperson for the Afterschool Alliance and played the title role in the hit television series, “Hercules: The Legendary Journeys.” The Afterschool Alliance organizes Lights On Afterschool, and the JCPenney Afterschool Fund is National Presenting Sponsor. Sorbo participated in the national kick-off event, featuring the Lights On Afterschool Traveling Light Bulb, on Sunday, October 2 in Los Angeles. Some 4,000 children, parents and community members joined him at the event, which was sponsored by the Beyond the Bell Branch of the Los Angeles Unified School District. He will also moderate a congressional event on Thursday, October 20 – Lights On Afterschool Day. Perlman will participate in a national media tour, spreading the word about Lights On Afterschool and the importance of afterschool programs. “We are delighted that Rhea and Kevin are joining us this year to help get out the word that afterschool programs are vitally important to children, families and communities,” said Afterschool Alliance Executive Director Jodi Grant. “Afterschool programs keep kids safe, help working families and inspire children to learn. -

Black History Trivia Bowl Study Questions Revised September 13, 2018 B C D 1 CATEGORY QUESTION ANSWER
Black History Trivia Bowl Study Questions Revised September 13, 2018 B C D 1 CATEGORY QUESTION ANSWER What national organization was founded on President National Association for the Arts Advancement of Colored People (or Lincoln’s Birthday? NAACP) 2 In 1905 the first black symphony was founded. What Sports Philadelphia Concert Orchestra was it called? 3 The novel Uncle Tom’s Cabin was published in what Sports 1852 4 year? Entertainment In what state is Tuskegee Institute located? Alabama 5 Who was the first Black American inducted into the Pro Business & Education Emlen Tunnell 6 Football Hall of Fame? In 1986, Dexter Gordan was nominated for an Oscar for History Round Midnight 7 his performance in what film? During the first two-thirds of the seventeenth century Science & Exploration Holland and Portugal what two countries dominated the African slave trade? 8 In 1994, which president named Eddie Jordan, Jr. as the Business & Education first African American to hold the post of U.S. Attorney President Bill Clinton 9 in the state of Louisiana? Frank Robinson became the first Black American Arts Cleveland Indians 10 manager in major league baseball for what team? What company has a successful series of television Politics & Military commercials that started in 1974 and features Bill Jell-O 11 Cosby? He worked for the NAACP and became the first field Entertainment secretary in Jackson, Mississippi. He was shot in June Medgar Evers 12 1963. Who was he? Performing in evening attire, these stars of The Creole Entertainment Show were the first African American couple to perform Charles Johnson and Dora Dean 13 on Broadway. -

David Rabe's Good for Otto Gets Star Studded Cast with F. Murray Abraham, Ed Harris, Mark Linn-Baker, Amy Madigan, Rhea Perl
David Rabe’s Good for Otto Gets Star Studded Cast With F. Murray Abraham, Ed Harris, Mark Linn-Baker, Amy Madigan, Rhea Perlman and More t2conline.com/david-rabes-good-for-otto-gets-star-studded-cast-with-f-murray-abraham-ed-harris-mark-linn-baker-amy- madigan-rhea-perlman-and-more/ Suzanna January 30, 2018 Bowling F. Murray Abraham (Barnard), Kate Buddeke (Jane), Laura Esterman (Mrs. Garland), Nancy Giles (Marci), Lily Gladstone (Denise), Ed Harris (Dr. Michaels), Charlotte Hope (Mom), Mark Linn- Baker (Timothy), Amy Madigan (Evangeline), Rileigh McDonald (Frannie), Kenny Mellman (Jerome), Maulik Pancholy (Alex), Rhea Perlman (Nora) and Michael Rabe (Jimmy), will lite up the star in the New York premiere of David Rabe’s Good for Otto. Rhea Perlman took over the role of Nora, after Rosie O’Donnell, became ill. Directed by Scott Elliott, this production will play a limited Off-Broadway engagement February 20 – April 1, with Opening Night on Thursday, March 8 at The Pershing Square Signature Center (The Alice Griffin Jewel Box Theatre, 480 West 42nd Street). Through the microcosm of a rural Connecticut mental health center, Tony Award-winning playwright David Rabe conjures a whole American community on the edge. Like their patients and their families, Dr. Michaels (Ed Harris), his colleague Evangeline (Amy Madigan) and the clinic itself teeter between breakdown and survival, wielding dedication and humanity against the cunning, inventive adversary of mental illness, to hold onto the need to fight – and to live. Inspired by a real clinic, Rabe finds humor and compassion in a raft of richly drawn characters adrift in a society and a system stretched beyond capacity. -

031906 It's a Parade of Stars As Tv Land Honors Dallas
Contacts: Jennifer Zaldivar Vanessa Reyes TV Land TV Land 646/228-2479 310/752-8081 IT’S A PARADE OF STARS AS TV LAND HONORS DALLAS, CHEERS, GOOD TIMES, BATMAN AND GREY’S ANATOMY Diana Ross, Billy Crystal, Hilary Swank, Patrick Dempsey, Robert Downey Jr., Mary Tyler Moore, Sid Caesar, Patrick Duffy, Larry Hagman, Ted Danson, Kelsey Grammer, John Amos, Jimmy “JJ” Walker, Jeremy Piven and Quentin Tarantino Among Dozens of Performers Celebrating Classic TV Santa Monica, CA, March 19, 2006 – It was an unforgettable evening as celebrities from television, music and film bestowed special tribute awards tonight to some of television’s most beloved series and stars at the fourth annual TV Land Awards: A Celebration of Classic TV . The honored shows included Cheers (Legend Award), Dallas (Pop Culture Award), Good Times (Impact Award), Batman (40 th Anniversary) and Grey’s Anatomy (Future Classic Award). The TV Land Awards was taped at The Barker Hangar on Sunday, March 19 and will air on TV Land (and simulcast on Nick at Nite) Wednesday, March 22 from 9 p.m. to 11 p.m. ET/PT. This star-studded extravaganza featured some unforgettable moments such as when actor and comedian Billy Crystal presented TV icon Sid Caesar with The Pioneer Award. Grammy award-winning superstar Diana Ross performing a medley of her famous hits including “Touch Me in the Morning,” “The Boss,” “Do You Know,” and “Ain’t No Mountain High Enough.” Acclaimed actor Robert Downey Jr. presented two-time Oscar winner Hilary Swank with the Big Screen/Little Star award. -

Reminder List of Productions Eligible for the 88Th Academy Awards
REMINDER LIST OF PRODUCTIONS ELIGIBLE FOR THE 88TH ACADEMY AWARDS ADULT BEGINNERS Actors: Nick Kroll. Bobby Cannavale. Matthew Paddock. Caleb Paddock. Joel McHale. Jason Mantzoukas. Mike Birbiglia. Bobby Moynihan. Actresses: Rose Byrne. Jane Krakowski. AFTER WORDS Actors: Óscar Jaenada. Actresses: Marcia Gay Harden. Jenna Ortega. THE AGE OF ADALINE Actors: Michiel Huisman. Harrison Ford. Actresses: Blake Lively. Kathy Baker. Ellen Burstyn. ALLELUIA Actors: Laurent Lucas. Actresses: Lola Dueñas. ALOFT Actors: Cillian Murphy. Zen McGrath. Winta McGrath. Peter McRobbie. Ian Tracey. William Shimell. Andy Murray. Actresses: Jennifer Connelly. Mélanie Laurent. Oona Chaplin. ALOHA Actors: Bradley Cooper. Bill Murray. John Krasinski. Danny McBride. Alec Baldwin. Bill Camp. Actresses: Emma Stone. Rachel McAdams. ALTERED MINDS Actors: Judd Hirsch. Ryan O'Nan. C. S. Lee. Joseph Lyle Taylor. Actresses: Caroline Lagerfelt. Jaime Ray Newman. ALVIN AND THE CHIPMUNKS: THE ROAD CHIP Actors: Jason Lee. Tony Hale. Josh Green. Flula Borg. Eddie Steeples. Justin Long. Matthew Gray Gubler. Jesse McCartney. José D. Xuconoxtli, Jr.. Actresses: Kimberly Williams-Paisley. Bella Thorne. Uzo Aduba. Retta. Kaley Cuoco. Anna Faris. Christina Applegate. Jennifer Coolidge. Jesica Ahlberg. Denitra Isler. 88th Academy Awards Page 1 of 32 AMERICAN ULTRA Actors: Jesse Eisenberg. Topher Grace. Walton Goggins. John Leguizamo. Bill Pullman. Tony Hale. Actresses: Kristen Stewart. Connie Britton. AMY ANOMALISA Actors: Tom Noonan. David Thewlis. Actresses: Jennifer Jason Leigh. ANT-MAN Actors: Paul Rudd. Corey Stoll. Bobby Cannavale. Michael Peña. Tip "T.I." Harris. Anthony Mackie. Wood Harris. David Dastmalchian. Martin Donovan. Michael Douglas. Actresses: Evangeline Lilly. Judy Greer. Abby Ryder Fortson. Hayley Atwell. ARDOR Actors: Gael García Bernal. Claudio Tolcachir. -
Sunday Morning Grid 12/24/17 Latimes.Com/Tv Times
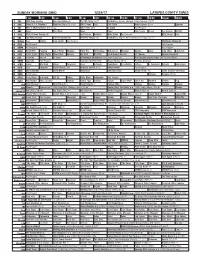
SUNDAY MORNING GRID 12/24/17 LATIMES.COM/TV TIMES 7 am 7:30 8 am 8:30 9 am 9:30 10 am 10:30 11 am 11:30 12 pm 12:30 2 CBS CBS News Sunday Face the Nation (N) The NFL Today (N) Å Football Los Angeles Chargers at New York Jets. (N) Å 4 NBC Today in L.A. Weekend Meet the Press (N) (TVG) NBC4 News Paid PGA TOUR Action Sports (N) Å Spartan 5 CW KTLA 5 Morning News at 7 (N) Å KTLA News at 9 In Touch Paid Program 7 ABC News This Week News News Jack Hanna Ocean Sea Rescue Wildlife 9 KCAL KCAL 9 News Sunday (N) Joel Osteen Schuller Mike Webb Paid Program REAL-Diego Paid 11 FOX Fox News Sunday FOX NFL Kickoff (N) FOX NFL Sunday (N) Football Los Angeles Rams at Tennessee Titans. (N) Å 13 MyNet Paid Matter Fred Jordan Paid Program Christmas Miracle at 18 KSCI Paid Program Paid Program 22 KWHY Paid Program Paid Program 24 KVCR Paint With Painting Joy of Paint Wyland’s Paint This Oil Painting Milk Street Mexican Martha Jazzy Julia Child Chefs Life 28 KCET 1001 Nights 1001 Nights Mixed Nutz Edisons Biz Kid$ Biz Kid$ 53rd Annual Wassail St. Thomas Holiday Handbells 30 ION Jeremiah Youseff In Touch A Firehouse Christmas (2016) Anna Hutchison. The Spruces and the Pines (2017) Jonna Walsh. 34 KMEX Conexión Paid Program Grandma Got Run Over Netas Divinas (TV14) Premios Juventud 40 KTBN James Win Walk Prince Carpenter Jesse In Touch PowerPoint It Is Written Jeffress K. -

Page 1 1 ALL in the FAMILY ARCHIE Bunker Emmy AWARD
ALL IN THE FAMILY ARCHIE Bunker Based on the British sitcom Till MEATHEAD Emmy AWARD winner for all DEATH Us Do Part MIKE Stivic four lead actors DINGBAT NORMAN Lear (creator) BIGOT EDITH Bunker Archie Bunker’s PLACE (spinoff) Danielle BRISEBOIS FIVE consecutive years as QUEENS CARROLL O’Connor number-one TV series Rob REINER Archie’s and Edith’s CHAIRS GLORIA (spinoff) SALLY Struthers displayed in Smithsonian GOOD Times (spinoff) Jean STAPLETON Institution 704 HAUSER (spinoff) STEPHANIE Mills CHECKING In (spinoff) The JEFFERSONS (spinoff) “STIFLE yourself.” “Those Were the DAYS” MALAPROPS Gloria STIVIC (theme) MAUDE (spinoff) WORKING class T S Q L D A H R S Y C V K J F C D T E L A W I C H S G B R I N H A A U O O A E Q N P I E V E T A S P B R C R I O W G N E H D E I E L K R K D S S O I W R R U S R I E R A P R T T E S Z P I A N S O T I C E E A R E J R R G M W U C O G F P B V C B D A E H T A E M N F H G G A M A L A P R O P S E E A N L L A R C H I E M U L N J N I O P N A M R O N Z F L D E I D R E D O O G S T I V I C A E N I K H T I D E T S A L L Y Y U A I O M Y G S T X X Z E D R S Q M 1 84052-2 TV Trivia Word Search Puzzles.indd 1 10/31/19 12:10 PM THE BIG BANG THEORY The show has a science Sheldon COOPER Mayim Bialik has a Ph.D. -

Emmy Award Winners
CATEGORY 2035 2034 2033 2032 Outstanding Drama Title Title Title Title Lead Actor Drama Name, Title Name, Title Name, Title Name, Title Lead Actress—Drama Name, Title Name, Title Name, Title Name, Title Supp. Actor—Drama Name, Title Name, Title Name, Title Name, Title Supp. Actress—Drama Name, Title Name, Title Name, Title Name, Title Outstanding Comedy Title Title Title Title Lead Actor—Comedy Name, Title Name, Title Name, Title Name, Title Lead Actress—Comedy Name, Title Name, Title Name, Title Name, Title Supp. Actor—Comedy Name, Title Name, Title Name, Title Name, Title Supp. Actress—Comedy Name, Title Name, Title Name, Title Name, Title Outstanding Limited Series Title Title Title Title Outstanding TV Movie Name, Title Name, Title Name, Title Name, Title Lead Actor—L.Ser./Movie Name, Title Name, Title Name, Title Name, Title Lead Actress—L.Ser./Movie Name, Title Name, Title Name, Title Name, Title Supp. Actor—L.Ser./Movie Name, Title Name, Title Name, Title Name, Title Supp. Actress—L.Ser./Movie Name, Title Name, Title Name, Title Name, Title CATEGORY 2031 2030 2029 2028 Outstanding Drama Title Title Title Title Lead Actor—Drama Name, Title Name, Title Name, Title Name, Title Lead Actress—Drama Name, Title Name, Title Name, Title Name, Title Supp. Actor—Drama Name, Title Name, Title Name, Title Name, Title Supp. Actress—Drama Name, Title Name, Title Name, Title Name, Title Outstanding Comedy Title Title Title Title Lead Actor—Comedy Name, Title Name, Title Name, Title Name, Title Lead Actress—Comedy Name, Title Name, Title Name, Title Name, Title Supp. Actor—Comedy Name, Title Name, Title Name, Title Name, Title Supp. -
What's New in the Arts
THE SAN DIEGO UNION-TRIBUNE SUNDAY• MARCH 28, 2021 E9 V IRTUALLY SPEAKING UCTV University of California Televi- sion (UCTV) is making a host of videos available on its website (uctv.tv/life-of-the-mind) during What’s new this period of social distancing. Among them, with descriptions ARMCHAIR TRAVEL courtesy of UCTV (text written by the UCTV staff): in DININGthe arts “Tales of Human History Told by Neanderthal and Denisovan DNA”: It’s well known that as Celebrating 50 years of Queen with 50 weeks’ worth of free clips anatomically modern humans THEATER dispersed out of Africa, they BY DAVID L. CODDON encountered and mated with The film adaptation of playwright other hominins such as Neander- Kemp Powers’ “One Night in thals and Denisovans. The ability e’ve all got a list of those bands we wish we’d seen in concert but never did. Miami,” for which he wrote the to identify and excavate extinct screenplay, earned Powers an At the top of mine would be Queen with Freddie Mercury. hominin DNA from the genomes Oscar nomination. Having really It’s hard to believe it’ll be 30 years this November since the passing of of contemporary individuals enjoyed it, I looked forward Mercury, he of arguably the most distinctive voice in rock ’n’ roll history. reveals considerable information eagerly to streaming a staged W about human history and how The 2018 biopic “Bohemian Rhapsody” was a diverting reminder of Mercury’s talent, reading of Powers’ new play those encounters with Neander- “Christa McAuliffe’s Eyes Were but a new clips show on Queen’s official YouTube Channel honoring the group’s 50-year thals and Denisovans shaped the Blue.” anniversary is a gift for fans that will keep on giving — for 50 weeks. -

'Oliver's Ghost'
‘OLIVER’S GHOST’ CAST BIOS MARTIN MULL (Clive) – Well known for his roles in “Rosanne,” “Ellen,” “Two and a Half Men” and “Clue,” actor and comedian Martin Mull has made himself a household name with his extensive career among Hollywood’s leading actors. Born in Chicago and raised in Ohio and Connecticut, funnyman Mull planned to become a painter when he enrolled in the Rhode Island School of Design. Although he graduated with a Bachelor of Fine Arts and a Masters in painting, Mull’s uncanny talent for stand-up comedy and satire led him to a career as a nightclub comedian, and eventually led to roles on television and film. Mull’s first role was on the nighttime absurdist soap opera “Mary Hartman, Mary Hartman,” in which his character was impaled by a Christmas tree, only to be brought back as that character’s twin brother. That led to spin-off talk shows “Fernwood Tonight” and “America 2-Night,” where Mull shared the screen with Fred Willard. Other television credits include a guest role on “The Golden Girls,” a long-running role as the gay boss of the lead character on “Roseanne,” starring Roseanne Barr, the CBS sitcom “Domestic Life” and “Gary Unmarried.” He has had series regular roles on “The Ellen Show,” opposite Ellen DeGeneres, “Sabrina, The Teenage Witch,” “Family Dog,” “The Jackie Thomas Show,” “Two and a Half Men,” “’Til Death” and, most recently, “American Dad!” His recent guest star credits include roles on “Eastwick,” “Reno 911,” “Just Shoot Me,” “Life With Bonnie,” “Less Than Perfect,” “Reba,” “My Boys,” “Mad Love” and “Law & Order: Special Victims Unit.” He also appeared as a guest star on the popular game show “Hollywood Squares,” appearing as the center square during the show’s final season in 2004. -

•Now Pitcbincj: Sam Malone• Written by Ken Levine, David Isaacs
, CBDRS •Now PitcbincJ: Sam Malone• 160591-016 Written By Ken Levine, David Isaacs Created and Developed By James Burrows Glen Charles Les Charles Return to Script Department PARAMOUNT PIC'l'traES CORPORATION PINAL DRAFT 5555 Melrose Avenue Hollywood, California 90038 December 9, 1982 CBEBRS •Now Pitcbin91 ~ SAM MALONE ••••••••••••••••••••••••••••••••• DD DANSON DIANE CBAMBERS ••••••••••••••••••••••••••••• SBBLLBY LONG COACH ERNll PANTUSSO ••••• •••••••••••••••••• NICX COLASANTO CARLA TORffLLI • • • • • • • • • • • • • • • • • • • • • • • • • • • • • RHEA PERLMAN CI.IPF • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • .. • JORN' RA'tZENBERGER NORM. • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • GEORGB 1IENDT LANA MARSHALL •••••••••••••••••••••••••••••• BARBARA BABCOCK TIBOR SVE'l'KOVIC. • • • • • • • • • • • • • • • • • • • • • • • • • • • RICX BILL PAUL.. • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • •.• • • PAOL VAUGHN LUIS TIANT ••••••••• • • • • • • • • • • • • • • • • • • • • • • • • BIMSBLF DIRECTOR ••••• •••••••••••••••••••••••••• • ••• nrr. BAR INT. SAM'S OFFICE CHBBRS •Nov Pitching: Sam Malone• .. TEASER -X FADE IN: INT. BAR - CLOSING TIME SAM AND COACH ARE CLOSING tJP. AS THEY HEAD FOR THE DOOR, COACH STOPS AND LOOKS AROUND. COACH Y'know Sam, this is my favorite time of day. SAM Closing time, Coach? COACH No, 1:37. SOmething about it, I don't know ••• SAM Yeah, it's nice. Everybody's probably got their favorite 1:37 story. 2. (X) 1eah. What time of day do you like, S&m? SAM Gee, I don't Jcnow ••• 8115'• nice. COACH I used to like 8:15, but I kinda outgrew it. AS THBY 'l'ALK, SAM 'l'tJRNS 00'1' THE LIGHTS. 'l'BBY GO 00'1' 'l'HB DOOR, UP '1'BB S'l'EPS AND DISAPPEAR. AP'l'ER A BEA'l' NORM COMES ROSSING QY! OP 'l'HB BATHROOM. NORM Wait a minute, I ••• BB STOPS, A THOOGH'l' OCCURS TO HIM. HE LOOKS AROUND,; GOES OVER AND TtJRNS ON 'l'HE TV. -

Big Band Early Jazz New Orleans Jazz Brass Band R
21st C. 21st C. Elec- 21st C. 21st C. 21st C. 90s/ Jazz Rock tronica R&B Rap Sacred Music 2000s Jason Moran Brittany Howard DJ Spooky The Roots Frank Ocean Kendrick Lamar Aeolians of Oakwood Kamasi Washington Gary Clark, Jr. Carl Craig Beyoncé Usher Kanye West Tasha Cobbs Concert & Roy Hargrove Janelle Monae Flying Lotus Rihanna Solange Nicki Minaj Jonathan McReynolds 90s Gospel Joshua Redman Stew Alicia Keys Jay-Z Marvin Sapp Terri Lyne Carrington Tamar-kali 50 Cent Kierra Sheard Kirk Franklin Classical Afropunk Trey McLaughlin Donnie McClurkin Mary Mary Audra McDonald, Soprano Donald Lawrence Lawrence Brownlee, Tenor Sounds of Blackness Morris Robinson, Bass 80s/90s Rock Techno 90s R&B 90s Rap Yolanda Adams Janinah Burnett, Soprano Nicole Mitchell, Composer Bad Brains Living Colour Doug Pinnick Juan Atkins R. Kelly Maxwell De La Soul Nas Tania Leon, Composer Fishbone Chocolate Genius Toshi Reagon Derrick May Mariah Carey Mary J. Blige A Tribe Called Jay-Z George E. Lewis, Composer Lenny Kravitz Garland Jeffreys Kevin Saunderson MeShell Erykah Badu Quest The Notorious 80s Superstars Terence Blanchard, Composer Tracy Chapman Slash D. Wynn NdegéOcello Boyz II Men Ice Cube B.I..G. Nkeiru Okoye, Composer D’Angelo Dr. Dre Lil’ Kim Michael Jackson Prince Lionel Richie Courtney Bryan, Composer Snoop Doggy Missy Elliott Tina Turner Whitney Houston Imani Winds, Wind quintet Dogg Lauryn Hill Wu-Tang Clan Outkast 80s Jazz House 80s Rap 2Pac 80s R&B 80s 70s/80s Wynton Greg Osby Frankie Knuckles Sugar Hill Gang LL Cool J Public Enemy Stevie Wonder Marsalis Geri Allen Ron Hardy Grandmaster Flash MC Lyte N .W.