Technology Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

First Reversals of Cognitive Decline in Alzheimer's Disease and Its
1/12/2017 First Reversals of Cognitive Decline in Alzheimer’sSystems Therapeutics, Disease and its PresidentPrecursors, Obama, MCI and and the End ofSCI Alzheimer’s Disease Dale E. Bredesen, M.D. Augustus Rose Professor Easton Laboratories for Neurodegenerative Disease Research UCLA Founding President, Buck Institute “There is nothing that will prevent, reverse, or slow the progress of Alzheimer’s disease.” “Everyone knows someone who is a cancer survivor; no one knows an Alzheimer’s survivor.” 1 1/12/2017 30,000,000 patients in 2012 3rd leading cause (James, B. D. et al. Contribution of Alzheimer disease to mortality in the United States. Neurology 82, 1045-1050, doi:10.1212/WNL. 0240 (2014) Pres. Obama and NAPA, 2011 160,000,000 patients in 2050 2 1/12/2017 Women at the epicenter of the epidemic •65% of patients •60% of caregivers •More common than breast cancer 0 Cures 3 1/12/2017 Alzheimer’s Disease (AD) Therapeutic Landscape A production APPROVED A aggregation Donepezil (Aricept) A clearance Rivastigmine (Exelon) Tau aggregation/phosph Galantamine (Razadyne) Cholinergic drugs Tacrine (Cognex) Others Memantine (Namenda) PHASE 3 PHASE 2 PHASE 1 Solanezumab ELND005 PBT2 AL-108 GSK933776 NIC5-15 PF04360365 AF102B MABT5102A Bapineuzmab Valproate Bryostatin-1 Nicotinamide Talsaclidine EHT-0202 NP12 ACC001 UB311 Alzemed Antioxidant BMS708163 Lithium AN1792 R1450 Begacestat Semagacestat Statins ABT089 NGF CAD106 V950 PF3084014 AZD3480 SB742457 Flurizan Dimebon E2012 Huperzine-A PRX03140 CTS21166 Rosiglitazone EGCg EVP6124 PUFA MK0752 MEM3454 TTP448 Phenserine CHF5074 PF-04447943 Clinical Trial in AD terminated “Game of Throwns” (243/244) R.I.P. R.I.P. R.I.P. -
Mode of Action
STROKE TBI DEMENTIA Mode of Action Reconnecting Neurons. Empowering for Life. NEW MULTI-MODAL THERAPIES FOR NEUROLOGICAL DISORDERS Sonic hedgehog (Shh) The Sonic Hedgehog (Shh) signalling pathway regulates the development Smoothened of organs including the organization of the brain. For example, the Shh (Smo) Patched (Ptch) activates the Gli complex, which is responsible for the expression of develop- mental genes underpinning neurorecovery and leading to an amplification of natural recovery. Gli Complex Gli Repressor Gli Activator Cerebrolysin activates the Shh pathway1 Cerebrolysin has a promoting effect on neurogenesis and oligodendrogenesis via stimulating the expression of the Shh signalling pathway. Cerebrolysin increases mRNA modulation of Shh and its receptors ‘Patched’ (Ptch) and ‘Smoothened’ (Smo). Shh PTCH Smo 5 * * 3 * 3 4 (n=9) (n=9) *p<0.05 (n=9) *p<0.05 *p<0.05 3 2 2 2 1 1 Fold changes (mean±SE) changes Fold (mean±SE) changes Fold 1 (mean±SE) changes Fold 0 0 0 0 20 0 20 0 20 CERE (µl/ml) CERE (µl/ml) CERE (µl/ml) Figure 1: Cerebrolysin stimulates the expression of the sonic hedgehog signalling pathway components in neural progenitor cells. Graphs show mRNA levels in an in vitro experiment. Studies confirm the important role of the sonic hedgehog pathway in post-stroke brain repair and functional recovery, and suggests the Shh pathway to be a possible target for prolongation of the therapeutic window after stroke.2 MAINTENANCE AND RECOVERY OF THE NEURONAL NETWORK Neurotrophic factors (NTFs) are signaling molecules that maintain, protect, and restore the neuronal network and ensure proper functioning of the brain. -

Workbook Psychiatry and Narcology
Kharkiv National Medical University Department of Psychiatry, Narcology and Medical Psychology WORKBOOK MANUAL FOR INDIVIDUAL WORK FOR MEDICAL STUDENTS PSYCHIATRY AND NARCOLOGY (Part 2) Student ___________________________________________________________ Faculty _________________________________________________________ Course _________________ Group _____________________________________ Kharkiv 2019 Затверджено вченою радою ХНМУ Протокол №5 від 23.05.2019 р. Psychiatry (Part 2) : workbook manual for individual work of students / I. Strelnikova, G. Samardacova, К. Zelenska – Kharkiv, 2019. – 103 p. Копіювання для розповсюдження в будь-якому вигляді частин або повністю можливо тільки з дозволу авторів навчального посібника. CLASS 7. NEUROTIC DISORDERS. CLINICAL FORMS. TREATMENT AND REHABILITATION. POSTTRAUMATIC STRESS DISORDER. TREATMENT AND REHABILITATION. Psychogenic diseases are a large and clinically varied group of diseases resulting from an effect of acute or long-term psychic traumas, which manifest themselves by both mental and somatoneurological disorders and, as a rule, are reversible. Psychogenic diseases are caused by a psychic trauma, i.e. some events which affect significant aspects of existence of the human being and result in deep psychological feelings. These may be subjectively significant events, i.e. those which are pathogenic for the majority of people. Besides, the psyche may be traumatized by conventionally pathogenic events, which cause feelings in an individual because of his peculiar hierarchy of values. Unfavorable psychogenic effects on the human being cause stress in him, i.e. a nonspecific reaction at the physiological, psychological and behavioural levels. Stress may exert some positive, mobilizing influence, but may result in disorganization of the organism activity. The stress, which exerts a negative influence and causes various disturbances and even diseases, is termed distress. Classification of neurotic disorders I. -

The Ndac (Neurology and Psychiatry) Held on 17.12.2011
1. RECOMMENDATIONS OF THE NDAC (NEUROLOGY AND PSYCHIATRY) HELD ON 17.12.2011:- The NDAC (Neurology and Psychiatry) deliberated the proposals on 17.12.2011and recommended the following:- AGENDA DRUG NAME RECOMMENDATIONS NO. Global Clinical Trials The drug has not yet been studied / approved in the country in adults. The tools to assess the cognitive affects are also not included in the 1 Rufinamide protocol except CBCL (child behaviours check list) which is not adequate. In view of above, the proposal to conduct the study in children 1 to 4 years of age was not recommended. DEFFREED Recommended for granting permission for the conduct of proposed study subject to following conditions: That subject from extension study 01050256 2 Lurasidone HCl should only be rolled over to the proposed study. Patients aged 18 to 65 years only should be included in the study. Since the study involves use of placebo without rescue medication in one arm in patients with 3 OPC-34712 acute schizophrenia, the proposal was not recommended for grant of permission. Since the study involves use of placebo without rescue medication in one arm in patients with 4 OPC-34712 acute schizophrenia, the proposal was not recommended for grant of permission. Recommended for granting permission for the 5 BMS-820836 conduct of proposed study. Patients aged 18 to 65 years only should be included in the study. Recommended for granting permission for the 6 BMS-820836 conduct of proposed study. Patients aged 18 to 65 years only should be included in the study. There were earlier studies conducted in USA which had failed as there was no statistically significant effect of the study drug at dose level of 5, 10 mg per day over placebo. -
Cphi & P-MEC China Exhibition List展商名单version版本20180116
CPhI & P-MEC China Exhibition List展商名单 Version版本 20180116 Booth/ Company Name/公司中英文名 Product/产品 展位号 Carbosynth Ltd E1A01 Toronto Research Chemicals Inc E1A08 SiliCycle Inc. E1A10 SA TOURNAIRE E1A11 Indena SpA E1A17 Trifarma E1A21 LLC Velpharma E1A25 Anuh Pharma E1A31 Chemclone Industries E1A51 Hetero Labs Limited E1B09 Concord Biotech Limited E1B10 ScinoPharm Taiwan Ltd E1B11 Dongkook Pharmaceutical Co., Ltd. E1B19 Shenzhen Salubris Pharmaceuticals Co., Ltd E1B22 GfM mbH E1B25 Leawell International Ltd E1B28 DCS Pharma AG E1B31 Agno Pharma E1B32 Newchem Spa E1B35 APEX HEALTHCARE LIMITED E1B51 AMRI E1C21 Aarti Drugs Limited E1C25 Espee Group Innovators E1C31 Ruland Chemical Co., Ltd. E1C32 Merck Chemicals (Shanghai) Co., Ltd. E1C51 Mediking Pharmaceutical Group Ltd E1C57 珠海联邦制药股份有限公司/The United E1D01 Laboratories International Holdings Ltd. FMC Corporation E1D02 Kingchem (Liaoning) Chemical Co., Ltd E1D10 Doosan Corporation E1D22 Sunasia Co., Ltd. E1D25 Bolon Pharmachem Co., Ltd. E1D26 Savior Lifetec Corporation E1D27 Alchem International Pvt Ltd E1D31 Polish Investment and Trade Agency E1D57 Fischer Chemicals AG E1E01 NGL Fine Chem Limited E1E24 常州艾柯轧辊有限公司/ECCO Roller E1E25 Linnea SA E1E26 Everlight Chemical Industrial Corporation E1E27 HARMAN FINOCHEM E1E28 Zhechem Co Ltd E1F01 Midas Pharma GmbH Shanghai Representativ E1F03 Supriya Lifescience Ltd E1F10 KOA Shoji Co Ltd E1F22 NOF Corporation E1F24 上海贺利氏工业技术材料有限公司/Heraeus E1F26 Materials Technology Shanghai Ltd. Novacyl Asia Pacific Ltd E1F28 PharmSol Europe Limited E1F32 Bachem AG E1F35 Louston International Inc. E1F51 High Science Co Ltd E1F55 Chemsphere Technology Inc. E1F57a PharmaCore Biotech Co., Ltd. E1F57b Rockwood Lithium GmbH E1G51 Sarv Bio Labs Pvt Ltd E1G57 抗病毒类、抗肿瘤类、抗感染类和甾体类中间体、原料药和药物制剂及医药合约研发和加工服务 上海创诺医药集团有限公司/Shanghai Desano APIs and Finished products of ARV, Oncology, Anti-infection and Hormone drugs and E1H01 Pharmaceuticals Co., Ltd. -

Alzheimer's Disease: Overview and Treatment Options
Alzheimer’s Disease: Overview and Treatment Options Jillian Blair Thomas, Pharm.D. Candidate 2013 Michael W. Frye, Pharm.D. Candidate 2013 Bernie R. Olin, Pharm.D., Associate Clinical Professor and Director Drug Information Center Auburn University, Harrison School of Pharmacy Universal Activity #: 0178-0000-12-114-H04-P | 1.5 credit hours (.15 CEUs) | Expires Dec. 12, 2015 Alabama Pharmacy Association | 334.271.4222 | www.aparx.org | [email protected] Introduction toxicity. The rate of progression of dementia may be slowed by controlling hypertension. Diabetes Alzheimer’s disease (AD) is the most may increase the risk of dementia through common cause of dementia in the United States multiple mechanisms. Glucose metabolites may affecting an estimated 5.4 million people, with have a toxic effect on the brain, specifically over 60% of those diagnosed being women. structures of the hippocampus, and vasculature. Worldwide, an estimated 24.3 million, possibly Insulin itself may increase the risk of AD due to as many as 35 million, people have been disturbances in insulin signaling pathways 1-6 diagnosed with Alzheimer’s disease. It is peripherally and in the brain.2,5 Insulin may also estimated that by the year 2050 between 13 and have a role in the regulation of metabolism of Aβ 2, 3 16 million Americans will be affected by AD. and tau protein.2 Alzheimer’s disease is more prevalent in African Dominantly inherited forms of AD 1 Americans and Hispanics than in whites. The account for only a small percentage of cases; majority of patients with AD are 65 years or however, there is a definite genetic link.1,2,5 older at the time of diagnosis, but about 5% of There is a high familial occurrence of AD linked patients diagnosed with AD are under the age of to autosomal dominant traits on chromosomes 65. -
Dementia Summary
Agency for Healthcare Research and Quality Evidence Report/Technology Assessment Number 97 Pharmacological Treatment of Dementia Summary Introduction 1. Does pharmacotherapy for dementia syndromes improve cognitive symptoms and The focus of this review is the pharmacological outcomes? treatment of dementia. Pharmacotherapy is often 2. Does pharmacotherapy delay cognitive the central intervention used to improve deterioration or delay disease onset of symptoms or delay the progression of dementia dementia syndromes? syndromes. The available agents vary with respect 3. Are certain drugs, including alternative to their therapeutic actions, and are supported by medicines (non-pharmaceutical), more varying levels of evidence for efficacy. This report effective than others? is a systematic evaluation of the evidence for 4. Do certain patient populations benefit more pharmacological interventions for the treatment from pharmacotherapy than others? of dementia in the domains of cognition, global 5. What is the evidence base for the treatment function, behavior/mood, quality of life/activities of ischemic vascular dementia (VaD)? of daily living (ADL) and caregiver burden. This review considers different types of Many medications have been studied in dementia populations (not just Alzheimer’s dementia patients. These agents can be classified Disease [AD]) in subjects from both community into three broad categories: and institutional settings. The studies eligible in 1. Cholinergic neurotransmitter modifying this systematic review were restricted to parallel agents, such as acetylcholinesterase inhibitors. RCTs of high methodological quality. 2. Non-cholinergic neurotransmitters/ neuropeptide modifying agents. Methods 3. Other pharmacological agents. A team of content specialists was assembled Although only five agents have been approved from both international and local experts. -

Counteracting EMF Toxicity with Peptides (Forget Global Warming Emfs Are Killing Us)
Counteracting EMF Toxicity with Peptides (Forget Global Warming EMFs are Killing Us) Dr. Kent Holtorf, MD Medical Director/CEO, Holtorf Medical Group (HoltorfMed.com) Medical Director/CEO, National Academy of Hypothyroidism (NAHypothyroidism.org) Medical Director, Integrative Peptides (IntegrativePeptides.com) Disclosure Statement Owner/CEO - Holtorf Medical Group HoltorfMed.com A multi-specialty medical group specializing in the treatment of complex endocrine dysfunction, CFS/fibromyalgia, chronic infectious diseases, immune dysfunction, neurodegenerative disease, and other complex chronic illnesses. Chief Medical Officer - The Non-Profit, The National Academy of Hypothyroidism and Integrative Sciences (NAHIS) NAHypothyroidism.org NAHIS is a non- profit, multidisciplinary medical society dedicated to the dissemination of new information on the diagnosis and treatment of hypothyroidism and complex conditions. NAHIS receives grants for clinical and laboratory research for novel methods in the diagnosis and treatment of hypothyroidism and chronic illnesses Chief Medical Officer - Integrative Peptides IntegrativePeptides.com Currently sells orally active and absorbable natural peptides in oral supplement form with unique delivery methods 2 Disclosure Statement Important Disclaimer In the interest of full disclosure, I am the All studies have limitations, and there is no perfect study. As with other studies, the studies Chief Medical Officer of Integrative Peptides. mentioned in this presentation and during the summit have limitations that should be considered when evaluating the efficacy of any treatment, including peptides, and determining the The opinions expressed are mine and do not appropriateness of peptide therapy for consumer use. A short summary, the abstract or reference to necessarily reflect those of Integrative a study may be discussed or provided. We are happy to provide you the entire study for your review of any study discussed, mentioned, presented or referenced. -

EVIDENCE-BASED REVIEW of STROKE REHABILITATION (18Th
EVIDENCE-BASED REVIEW OF STROKE REHABILITATION (18th Edition) Robert Teasell MD1, Andreea Cotoi MSc1, Jeffrey Chow MSc1, Joshua Wiener BHSc1, Alice Iliescu BSc1, Norhayati Hussein MBBS, Norine Foley MSc, Katherine Salter PhD (cand.) 1Collaboration of Rehabilitation Research Institute, Parkwood Institute Research, Lawson Health Research Institute, St. Joseph’s Health Care London, London, Ontario Executive Summary The Stroke Rehabilitation Evidence-Based Review (SREBR) reviews techniques, therapies, devices, procedures and medications associated with stroke rehabilitation. The purpose of the Evidence-Based Review of Stroke Rehabilitation was to fulfil the 12th recommendation of The Stroke Rehabilitation Consensus Panel Report that supported the continuing review of stroke rehabilitation research with the “purpose of maintaining timely and accurate information on effective stroke rehabilitation, identifying ideas for further research, supporting continuous peer-review and encouraging improved evidence-based practice.” The aim of the SREBR was to: • Be an up-to-date review of the current evidence in stroke rehabilitation. • Provide a comprehensive and accessible review to facilitate best-practice. • Provide specific conclusion based on evidence that could be used to help direct stroke care at the bedside and at home. Since its original publication in April 2002, the SREBR has undergone eighteen major revisions and now includes articles published up to December 2016. To date, we have included over 2,300 randomized controlled trials (RCTs). Methods For the first edition of the SREBR a literature search using multiple databases (MEDLINE, EBASE, MANTIS, PASCAL, and Sci Search) was conducted to identify all potential trials published from 1970- 2001, regardless of study design. The search was restricted to the English language and excluded animal studies. -

Lessons Learned
Prevention and Reversal of Chronic Disease Copyright © 2019 RN Kostoff PREVENTION AND REVERSAL OF CHRONIC DISEASE: LESSONS LEARNED By Ronald N. Kostoff, Ph.D., School of Public Policy, Georgia Institute of Technology 13500 Tallyrand Way, Gainesville, VA, 20155 [email protected] KEYWORDS Chronic disease prevention; chronic disease reversal; chronic kidney disease; Alzheimer’s Disease; peripheral neuropathy; peripheral arterial disease; contributing factors; treatments; biomarkers; literature-based discovery; text mining ABSTRACT For a decade, our research group has been developing protocols to prevent and reverse chronic diseases. The present monograph outlines the lessons we have learned from both conducting the studies and identifying common patterns in the results. The main product of our studies is a five-step treatment protocol to reverse any chronic disease, based on the following systemic medical principle: at the present time, removal of cause is a necessary, but not necessarily sufficient, condition for restorative treatment to be effective. Implementation of the five-step treatment protocol is as follows: FIVE-STEP TREATMENT PROTOCOL TO REVERSE ANY CHRONIC DISEASE Step 1: Obtain a detailed medical and habit/exposure history from the patient. Step 2: Administer written and clinical performance and behavioral tests to assess the severity of symptoms and performance measures. Step 3: Administer laboratory tests (blood, urine, imaging, etc) Step 4: Eliminate ongoing contributing factors to the chronic disease Step 5: Implement treatments for the chronic disease This individually-tailored chronic disease treatment protocol can be implemented with the data available in the biomedical literature now. It is general and applicable to any chronic disease that has an associated substantial research literature (with the possible exceptions of individuals with strong genetic predispositions to the disease in question or who have suffered irreversible damage from the disease). -
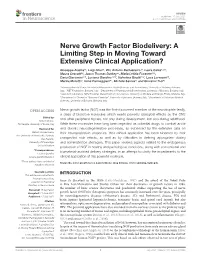
Nerve Growth Factor Biodelivery: a Limiting Step in Moving Toward Extensive Clinical Application?
fnins-15-695592 July 9, 2021 Time: 19:4 # 1 REVIEW published: 15 July 2021 doi: 10.3389/fnins.2021.695592 Nerve Growth Factor Biodelivery: A Limiting Step in Moving Toward Extensive Clinical Application? Giuseppe Alastra1†, Luigi Aloe2†, Vito Antonio Baldassarro1†, Laura Calzà1,2,3†, Maura Cescatti2†, Jason Thomas Duskey4†, Maria Letizia Focarete1,5†, Daria Giacomini1,5†, Luciana Giardino2,6*†, Valentina Giraldi1,5†, Luca Lorenzini6†, Marzia Moretti2†, Irene Parmeggiani4†, Michele Sannia1† and Giovanni Tosi4† 1 Interdepartmental Centre for Industrial Research in Health Sciences and Technologies, University of Bologna, Bologna, Italy, 2 IRET Foundation, Bologna, Italy, 3 Department of Pharmacy and Biotechnology, University of Bologna, Bologna, Italy, 4 Nanotech Laboratory, TeFarTI Center, Department of Life Sciences, University of Modena and Reggio Emilia, Modena, Italy, 5 Department of Chemistry “Giacomo Ciamician”, University of Bologna, Bologna, Italy, 6 Department of Veterinary Medical Sciences, University of Bologna, Bologna, Italy Nerve growth factor (NGF) was the first-discovered member of the neurotrophin family, a class of bioactive molecules which exerts powerful biological effects on the CNS Edited by: and other peripheral tissues, not only during development, but also during adulthood. Robert Nistico, Tor Vergata University of Rome, Italy While these molecules have long been regarded as potential drugs to combat acute Reviewed by: and chronic neurodegenerative processes, as evidenced by the extensive data on Hubert Hondermarck,