A Machine-Learning Approach to Measuring Tumor Ph Using MRI
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MDCT and Contrast Media: What Are the Risks?
071_078_00_Thomsen:Thomsen 13-02-2008 9:32 Pagina 71 MDCT and Contrast Media: What are the Risks? Henrik S. Thomsen Department of Diagnostic Radiology, Copenhagen University Hospital Herlev, Herlev Department of Diagnostic Sciences, Faculty of Health Sciences, University of Copenhagen, Denmark Introduction Renal Adverse Reactions With the advent of multi-detector computed to- Contrast-material-induced kidney damage is imme- mography (MDCT) technology, the number of pa- diate, starting as soon as the first CM molecule reach- tients undergoing contrast-enhanced CT (CECT) es the kidney; however, it takes several hours or days studies has steadily grown in the last 6 years. In for a deterioration of renal function to be detected. 2005, approximately 22 million CECT examinations Despite more than 30 years of research, the patho- were carried out in the European Union, and 32 mil- physiology of CM-induced nephropathy (CIN) is lion in the United States (The Imaging Market Guide poorly elucidated. Nonetheless, several risk factors 2005. Arlington Medical Resources, Inc., Philadel- are well-known and can be divided into CM- and pa- phia, PA). Unfortunately, post-contrast-material-re- tient-related factors. lated adverse events, i.e., all those unintended and unfavorable signs, symptoms, or diseases temporally associated with the use of an iodinated contrast ma- Contrast-Medium-Related Factors terial (CM), are a common occurrence in radiology departments. Most adverse events occur within the More than 25 years ago, Barrett and Carlisle [1] first 60 min following CM administration (“imme- showed that the incidence of CIN is significantly diate” or “acute” adverse events), with the greatest higher after the administration of high-osmolarity risk in the first 20 min. -

Pharmacologyonline 2: 727-753 (2010) Ewsletter Bradu and Rossini
Pharmacologyonline 2: 727-753 (2010) ewsletter Bradu and Rossini COTRAST AGETS - IODIATED PRODUCTS. SECOD WHO-ITA / ITA-OMS 2010 COTRIBUTIO O AGGREGATE WHO SYSTEM-ORGA CLASS DISORDERS AD/OR CLUSTERIG BASED O REPORTED ADVERSE REACTIOS/EVETS Dan Bradu and Luigi Rossini* Servizio Nazionale Collaborativo WHO-ITA / ITA-OMS, Università Politecnica delle Marche e Progetto di Farmacotossicovigilanza, Azienda Ospedaliera Universitaria Ospedali Riuniti di Ancona, Regione Marche, Italia Summary From the 2010 total basic adverse reactions and events collected as ADRs preferred names in the WHO-Uppsala Drug Monitoring Programme, subdivided in its first two twenty years periods as for the first seven iodinated products diagnostic contrast agents amidotrizoate, iodamide, iotalamate, iodoxamate, ioxaglate, iohexsol and iopamidol, their 30 WHO-system organ class disorders (SOCDs) aggregates had been compared. Their common maximum 97% levels identified six SOCDs only, apt to evaluate the most frequent single ADRs for each class, and their percentual normalization profiles for each product. The WILKS's chi square statistics for the related contingency tables, and Gabriel’s STP procedure applied to the extracted double data sets then produced profile binary clustering, as well as Euclidean confirmatory plots. They finally showed similar objectively evaluated autoclassificative trends of these products, which do not completely correspond to their actual ATC V08A A, B and C subdivision: while amidotrizoate and iotalamate, and respectively iohesol and iopamidol are confirmed to belong to the A and B subgroups, ioxaglate behaves fluctuating within A, B and C, but iodamide looks surprizingly, constantly positioned together with iodoxamate as binary/ternary C associated. In view of the recent work of Campillos et al (Science, 2008) which throws light on the subject, the above discrepancies do not appear anymore unexpected or alarming. -

Page 1 Note: Within Nine Months from the Publication of the Mention
Europäisches Patentamt (19) European Patent Office & Office européen des brevets (11) EP 1 411 992 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 49/04 (2006.01) A61K 49/18 (2006.01) 13.12.2006 Bulletin 2006/50 (86) International application number: (21) Application number: 02758379.8 PCT/EP2002/008183 (22) Date of filing: 23.07.2002 (87) International publication number: WO 2003/013616 (20.02.2003 Gazette 2003/08) (54) IONIC AND NON-IONIC RADIOGRAPHIC CONTRAST AGENTS FOR USE IN COMBINED X-RAY AND NUCLEAR MAGNETIC RESONANCE DIAGNOSTICS IONISCHES UND NICHT-IONISCHES RADIOGRAPHISCHES KONTRASTMITTEL ZUR VERWENDUNG IN DER KOMBINIERTEN ROENTGEN- UND KERNSPINTOMOGRAPHIEDIAGNOSTIK SUBSTANCES IONIQUES ET NON-IONIQUES DE CONTRASTE RADIOGRAPHIQUE UTILISEES POUR ETABLIR DES DIAGNOSTICS FAISANT APPEL AUX RAYONS X ET A L’IMAGERIE PAR RESONANCE MAGNETIQUE (84) Designated Contracting States: (74) Representative: Minoja, Fabrizio AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Bianchetti Bracco Minoja S.r.l. IE IT LI LU MC NL PT SE SK TR Via Plinio, 63 20129 Milano (IT) (30) Priority: 03.08.2001 IT MI20011706 (56) References cited: (43) Date of publication of application: EP-A- 0 759 785 WO-A-00/75141 28.04.2004 Bulletin 2004/18 US-A- 5 648 536 (73) Proprietor: BRACCO IMAGING S.p.A. • K HERGAN, W. DORINGER, M. LÄNGLE W.OSER: 20134 Milano (IT) "Effects of iodinated contrast agents in MR imaging" EUROPEAN JOURNAL OF (72) Inventors: RADIOLOGY, vol. 21, 1995, pages 11-17, • AIME, Silvio XP002227102 20134 Milano (IT) • K.M. -

ACR Manual on Contrast Media
ACR Manual On Contrast Media 2021 ACR Committee on Drugs and Contrast Media Preface 2 ACR Manual on Contrast Media 2021 ACR Committee on Drugs and Contrast Media © Copyright 2021 American College of Radiology ISBN: 978-1-55903-012-0 TABLE OF CONTENTS Topic Page 1. Preface 1 2. Version History 2 3. Introduction 4 4. Patient Selection and Preparation Strategies Before Contrast 5 Medium Administration 5. Fasting Prior to Intravascular Contrast Media Administration 14 6. Safe Injection of Contrast Media 15 7. Extravasation of Contrast Media 18 8. Allergic-Like And Physiologic Reactions to Intravascular 22 Iodinated Contrast Media 9. Contrast Media Warming 29 10. Contrast-Associated Acute Kidney Injury and Contrast 33 Induced Acute Kidney Injury in Adults 11. Metformin 45 12. Contrast Media in Children 48 13. Gastrointestinal (GI) Contrast Media in Adults: Indications and 57 Guidelines 14. ACR–ASNR Position Statement On the Use of Gadolinium 78 Contrast Agents 15. Adverse Reactions To Gadolinium-Based Contrast Media 79 16. Nephrogenic Systemic Fibrosis (NSF) 83 17. Ultrasound Contrast Media 92 18. Treatment of Contrast Reactions 95 19. Administration of Contrast Media to Pregnant or Potentially 97 Pregnant Patients 20. Administration of Contrast Media to Women Who are Breast- 101 Feeding Table 1 – Categories Of Acute Reactions 103 Table 2 – Treatment Of Acute Reactions To Contrast Media In 105 Children Table 3 – Management Of Acute Reactions To Contrast Media In 114 Adults Table 4 – Equipment For Contrast Reaction Kits In Radiology 122 Appendix A – Contrast Media Specifications 124 PREFACE This edition of the ACR Manual on Contrast Media replaces all earlier editions. -
ACR Manual on Contrast Media – Version 9, 2013 Table of Contents / I
ACR Manual on Contrast Media Version 9 2013 ACR Committee on Drugs and Contrast Media ACR Manual on Contrast Media – Version 9, 2013 Table of Contents / i ACR Manual on Contrast Media Version 9 2013 ACR Committee on Drugs and Contrast Media © Copyright 2013 American College of Radiology ISBN: 978-1-55903-012-0 Table of Contents Topic Last Updated Page 1. Preface. V9 – 2013 . 3 2. Introduction . V7 – 2010 . 4 3. Patient Selection And Preparation Strategies . V7 – 2010 . 5 4. Injection of Contrast Media . V7 – 2010 . 13 5. Extravasation Of Contrast Media . V7 – 2010 . 17 6. Allergic-Like And Physiologic Reactions To Intravascular Iodinated Contrast Media . V9 – 2013 . 21 7. Contrast Media Warming . V8 – 2012 . 29 8. Contrast-Induced Nephrotoxicity . V8 – 2012 . 33 9. Metformin . V7 – 2010 . 43 10. Contrast Media In Children . V7 – 2010 . 47 11. Gastrointestinal (GI) Contrast Media In Adults: Indications And Guidelines V9 – 2013 . 55 12. Adverse Reactions To Gadolinium-Based Contrast Media . V7 – 2010 . 77 13. Nephrogenic Systemic Fibrosis . V8 – 2012 . 81 14. Treatment Of Contrast Reactions . V9 – 2013 . 91 15. Administration Of Contrast Media To Pregnant Or Potentially Pregnant Patients . V9 – 2013 . 93 16. Administration Of Contrast Media To Women Who Are Breast-Feeding . V9 – 2013 . 97 Table 1 – Indications for Use of Iodinated Contrast Media . V9 – 2013 . 99 Table 2 – Organ and System-Specific Adverse Effects from the Administration of Iodine-Based or Gadolinium-Based Contrast Agents. V9 – 2013 . 100 Table 3 – Categories of Acute Reactions . V9 – 2013 . 101 Table 4 – Treatment of Acute Reactions to Contrast Media in Children . V9 – 2013 . -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Injection of Contrast Media V7 – 2010 13 5
ACR Manual on Contrast Media Version 8 2012 ACR Committee on Drugs and Contrast Media ACR Manual on Contrast Media Version 8 2012 ACR Committee on Drugs and Contrast Media © Copyright 2012 American College of Radiology ISBN: 978-1-55903-009-0 Table of Contents Topic Last Updated Page 1. Preface. V8 – 2012 . 3 2. Introduction . V7 – 2010 . 4 3. Patient Selection and Preparation Strategies . V7 – 2010 . 5 4. Injection of Contrast Media . V7 – 2010 . 13 5. Extravasation of Contrast Media . V7 – 2010 . 17 6. Adverse Events After Intravascular Iodinated Contrast Media . V8 – 2012 . 21 Administration 7. Contrast Media Warming . V8 – 2012 . 29 8. Contrast-Induced Nephrotoxicity . V8 – 2012 . 33 9. Metformin . V7 – 2010 . 43 10. Contrast Media in Children . V7 – 2010 . 47 11. Iodinated Gastrointestinal Contrast Media in Adults: Indications . V7 – 2010 . 55 and Guidelines 12. Adverse Reactions to Gadolinium-Based Contrast Media . V7 – 2010 . 59 13. Nephrogenic Systemic Fibrosis (NSF) . V8 – 2012 . 63 14. Treatment of Contrast Reactions . V8 – 2012 . 73 15. Administration of Contrast Media to Pregnant or Potentially . V6 – 2008. 75 Pregnant Patients 16. Administration of Contrast Media to Breast-Feeding Mothers . V6 – 2008 . 79 Table 1 – Indications for Use of Iodinated Contrast Media . V6 – 2008 . 81 Table 2 – Organ or System-Specific Adverse Effects from the Administration . V7 – 2010 . 82 of Iodine-Based or Gadolinium-Based Contrast Agents Table 3 – Categories of Reactions . V7 – 2010 . 83 Table 4 – Management of Acute Reactions in Children . V7 – 2010 . 84 Table 5 – Management of Acute Reactions in Adults . V6 – 2008 . 86 Table 6 – Equipment for Emergency Carts . V6 – 2008 . -

The Risk of Contrast Media-Induced Ventricular Fibrillation Is Low in Canine Coronary Arteriography with Ioxilan
FULL PAPER Surgery The Risk of Contrast Media-Induced Ventricular Fibrillation is Low in Canine Coronary Arteriography with Ioxilan Kazuhiro MISUMI, Oki TATENO, Makoto FUJIKI, Naoki MIURA and Hiroshi SAKAMOTO Department of Veterinary Medicine, Kagoshima University, 21–24 Korimoto 1-chome, Kagoshima 890–0065, Japan (Received 5 August 1999/Accepted 28 December 1999) ABSTRACT. Previous studies have proposed that sodium supplement to nonionic contrast media (CM) can decrease the risk of ventricular fibrillation (VF). This study was designed to compare the occurence of VF induced by ioxilan (containing 9 mmol/LNa+) with other nonionic CMs. After wedging a catheter in the right coronary artery, test solutions including ioxilan, ioversol, iomeprol, and iopromide were infused for 30 sec at the rate of 0.4 ml/sec or until VF occurred. Then, incidence of VF, contact time (i.e. the time required to produce VF), and QTc were measured. Also, the CMs other than ioxilan were investigated at sodium levels adjusted to 9 and 20 mmol/L Na+. The incidence of VF with ioxilan (0% ) was the lowest of all. In the other CMs, the incidence decreased in accordance with increase of sodium. Iomeprol and iopromide showed significant reduction of VF incidence at the sodium level of 20 mmol/L. The higher sodium supplements also prolonged the contact times. The increase of QTc was the greatest in ioxilan. Ioxilan has the least arrythmogenic property among the current low-osmolality nonionic CMs. This property might be attributable to an optimal sodium concentration of 9 mmol/L in the CM.—KEY WORDS: contrast media, coronary arteriography, ioxilan, ventricular fibrillation. -

Active Moiety Name FDA Established Pharmacologic Class (EPC) Text
FDA Established Pharmacologic Class (EPC) Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: Active Moiety Name “(Drug) is a (FDA EPC Text Phrase) indicated for [indication(s)].” For each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13. -

Premedication for Contrast Medium Allergies Factfinder
Published March 2014 Premedication for Contrast Medium Allergies FactFinder Committed to providing helpful information to International Spine Intervention Society members about key patient safety issues, the Society’s Patient Safety Committee has developed a FactFinder series. FactFinders will explore and debunk myths surrounding patient safety issues. The intent of this FactFinder is to present the evidence regarding the effectiveness of premedication for contrast medium allergies that impact the delivery of spinal procedures. Myth #1: In patients with radiocontrast media (RCM) allergy, it is safe to proceed with RCM injection as long as the patient is premedicated with steroids and antihistamines. Fact: Although premedication likely reduces the risks associated with injecting RCM, no premedication regimen has been proven safe for a RCM allergic reaction. Conclusions & Recommendations The International Spine Intervention Society Guidelines recommend the use of RCM for nearly all spinal diagnostic and treatment procedures.1 An understanding of the severity and frequency of reactions to RCM is paramount prior to discussing premedication. Reactions to RCM are immediate, defined as within the first hour, with 70% occurring within the first five minutes; or late, occurring between one hour and one week later. The late reactions are typically cutaneous.2 There are three types of immediate reactions: mild, moderate, and severe. Mild reactions: include nausea, vomiting, and mild urticaria. These signs and symptoms appear self-limited without evidence of progression. Treatment usually entails only observation and reassurance, however, these reactions may progress into a more severe category. Moderate reactions: include moderate urticaria, vasovagal reaction, mild bronchospasm, and tachycardia. These reactions require treatment, but are not immediately life threatening. -
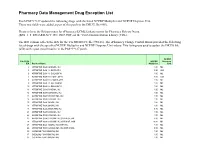
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

FDA Listing of Established Pharmacologic Class Text Phrases January 2021
FDA Listing of Established Pharmacologic Class Text Phrases January 2021 FDA EPC Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: “(Drug) is a (FDA EPC Text Phrase) indicated for Active Moiety Name [indication(s)].” For each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13.