Glaucoma Related to Ocular and Orbital Tumors Sonal P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
ICO Residency Curriculum 2Nd Edition and Updated Community Eye Health Section
ICO Residency Curriculum 2nd Edition and Updated Community Eye Health Section The International Council of Ophthalmology (ICO) Residency Curriculum offers an international consensus on what residents in ophthalmology should be taught. While the ICO curriculum provides a standardized content outline for ophthalmic training, it has been designed to be revised and modified, with the precise local detail for implementation left to the region’s educators. Download the Curriculum from the ICO website: icoph.org/curricula.html. www.icoph.org Copyright © International Council of Ophthalmology 2016. Adapt and translate this document for your noncommercial needs, but please include ICO credit. All rights reserved. First edition 201 6 . First edition 2006, second edition 2012, Community Eye Health Section updated 2016. International Council of Ophthalmology Residency Curriculum Introduction “Teaching the Teachers” The International Council of Ophthalmology (ICO) is committed to leading efforts to improve ophthalmic education to meet the growing need for eye care worldwide. To enhance educational programs and ensure best practices are available, the ICO focuses on "Teaching the Teachers," and offers curricula, conferences, courses, and resources to those involved in ophthalmic education. By providing ophthalmic educators with the tools to become better teachers, we will have better-trained ophthalmologists and professionals throughout the world, with the ultimate result being better patient care. Launched in 2012, the ICO’s Center for Ophthalmic Educators, educators.icoph.org, offers a broad array of educational tools, resources, and guidelines for teachers of residents, medical students, subspecialty fellows, practicing ophthalmologists, and allied eye care personnel. The Center enables resources to be sorted by intended audience and guides ophthalmology teachers in the construction of web-based courses, development and use of assessment tools, and applying evidence-based strategies for enhancing adult learning. -

Download Report Appendixes [PDF · 224
Appendices Appendix A. Selected Internet Links Appendix Table A1. Internet links for radiotherapy organizations Organization URL address Deutsche Gesellschaft fur http://www.degro.org/jsp_public/cms/index.jsp Radiooncologie European Society for Therapeutic http://www.estroweb.org/estro/index.cfm Radiology and Oncology American Society for Therapeutic http://www.astro.org/ Radiology and Oncology National Association for Proton http://www.proton-therapy.org/ Therapy Particle Therapy Cooperative http://ptcog.web.psi.ch/ Group (Accessed June 16, 2008) Appendix Table A2. Internet links for particle beam instrumentation companies Company URL address Ion Beam Applications (IBA) http://www.iba-worldwide.com/ Solutions Still River Systems Inc http://www.stillriversystems.com/ Optivus Proton Therapy http://www.optivus.com/ Siemens http://www.medical.siemens.com/ Hitachi: Proton beam Therapy http://www.pi.hitachi.co.jp/rd-eng/product/industrial-sys/accelerator- sys/proton-therapy-sys/proton-beam-therapy/index.html ACCEL Instruments http://www.proton-therapy.com/ (Accessed June 16, 2008) Appendix Table A3. Internet links for particle beam treatment centers in the USA Center/Institute URL address Francis H. Burr Proton Therapy http://www.massgeneral.org/cancer/about/providers/radiation/proton/i Center (NPTC) ndex.asp Loma Linda University Proton http://www.llu.edu/proton/index.html Therapy Center University of California, Crocker http://media.cnl.ucdavis.edu/crocker/website/default.php Nuclear Lab Midwest Proton Radiotherapy http://www.mpri.org/ Institute, Bloomington M.D. Anderson Proton Therapy http://www.mdanderson.org/care_centers/radiationonco/ptc/ Center, Houston University of Florida Proton http://www.floridaproton.org/ Therapy Institute, Jacksonville (Accessed June 16, 2008) A-1 Appendix B. -

Ocular Oncology and Pathology 2018 Hot Topics in Ocular Pathology and Oncology— an Update
Ocular Oncology and Pathology 2018 Hot Topics in Ocular Pathology and Oncology— An Update Program Directors Patricia Chévez-Barrios MD and Dan S Gombos MD In conjunction with the American Association of Ophthalmic Oncologists and Pathologists McCormick Place Chicago, Illinois Saturday, Oct. 27, 2018 Presented by: The American Academy of Ophthalmology 2018 Ocular Oncology and Pathology Subspecialty Day Advisory Committee Staff Planning Group Daniel S Durrie MD Melanie R Rafaty CMP DES, Director, Patricia Chévez-Barrios MD Associate Secretary Scientific Meetings Program Director Julia A Haller MD Ann L’Estrange, Subspecialty Day Manager Dan S Gombos MD Michael S Lee MD Carolyn Little, Presenter Coordinator Program Director Francis S Mah MD Debra Rosencrance CMP CAE, Vice R Michael Siatkowski MD President, Meetings & Exhibits Former Program Directors Kuldev Singh MD MPH Patricia Heinicke Jr, Copy Editor 2016 Carol L Shields MD Mark Ong, Designer Maria M Aaron MD Gina Comaduran, Cover Designer Patricia Chévez-Barrios MD Secretary for Annual Meeting 2014 Hans E Grossniklaus MD Arun D Singh MD ©2018 American Academy of Ophthalmology. All rights reserved. No portion may be reproduced without express written consent of the American Academy of Ophthalmology. ii Planning Group 2018 Subspecialty Day | Ocular Oncology & Pathology 2018 Ocular Oncology and Pathology Planning Group On behalf of the American Academy of Ophthalmology and the American Association of Ophthalmic Oncologists and Pathologists, it is our pleasure to welcome you to Chicago and -
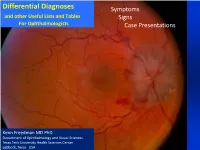
Differential Diagnoses Symptoms and Other Useful Lists and Tables Signs for Ophthalmologists Case Presentations
Differential Diagnoses Symptoms and other Useful Lists and Tables Signs For Ophthalmologists Case Presentations Kenn Freedman MD PhD Department of Ophthalmology and Visual Sciences Texas Tech University Health Sciences Center Lubbock, Texas USA Acknowledgments and Disclaimer The differential diagnoses and lists contained herein are not meant to be exhaustive, but are to give in most cases the most common causes of many ocular / visual symptoms, signs and situations. Included also in these lists are also some less common, but serious conditions that must be “ruled-out”. These lists have been based on years of experience, and I am grateful for God’s help in developing them. I also owe gratitude to several sources* including Roy’s classic text on Ocular Differential Diagnosis. * Please see references at end of document This presentation, of course, will continue to be a work in progress and any concerns or suggestions as to errors or omissions or picture copyrights will be considered. Please feel free to contact me at [email protected] Kenn Freedman Lubbock, Texas - October 2018 Disclaimer: The diagnostic algorithm for the diagnosis and management of Ocular or Neurological Conditions contained in this presentation is not intended to replace the independent medical or professional judgment of the physician or other health care providers in the context of individual clinical circumstances to determine a patient’s care. Use of this Presentation The lists are divided into three main areas 1. Symptoms 2. Signs from the Eight Point Eye Exam 3. Common Situations and Case Presentations The index for all of the lists is given on the following 3 pages. -

Uveal Melanoma National Guidelines
Uveal Melanoma Guidelines – Draft for Consultation Uveal Melanoma National Guidelines Draft for public consulation June 2014 This project is the independent work of the Uveal Melanoma Guideline Development Group and is funded by Melanoma Focus (http://melanomafocus.com/) um_guideline_cons_draft_v2_23_6_14 Last saved by Nancy Turnbull Date 16 June 2014 Page 1 of 93 Uveal Melanoma Guidelines – Draft for Consultation Uveal Melanoma 1. Executive Summary ......................................................................................................................... 6 1.1 Care Pathway .......................................................................................................................... 6 1.2 Recommendations .................................................................................................................. 8 1.2.1 Patient Choice and Shared decision-making .................................................................. 8 1.2.2 Service Configuration ...................................................................................................... 8 1.2.3 General Guidance............................................................................................................ 8 1.2.4 Primary management ..................................................................................................... 9 1.2.5 Prognostication ............................................................................................................. 11 1.2.6 Surveillance .................................................................................................................. -

Uveal Melanoma National Guidelines
Uveal Melanoma Guidelines January 2015 Uveal Melanoma National Guidelines January 2015 Authors: Nathan P, Cohen V, Coupland S, Curtis K, Damato B, Evans J, Fenwick S, Kirkpatrick L, Li O, Marshall E, McGuirk K, Ottensmeier C, Pearce N, Salvi S, Stedman B, Szlosarek P, Turnbull N This project is the independent work of the Uveal Melanoma Guideline Development Group and is funded by Melanoma Focus (http://melanomafocus.com/) Page 1 of 112 Uveal Melanoma Guidelines January 2015 Uveal Melanoma 1. Executive Summary ......................................................................................................................... 6 1.1 Care Pathway .......................................................................................................................... 6 1.2 Recommendations ................................................................................................................ 10 1.2.1 Patient Choice and Shared decision-making ................................................................ 10 1.2.2 Service Configuration .................................................................................................... 10 1.2.3 General Guidance.......................................................................................................... 10 1.2.4 Primary management ................................................................................................... 11 1.2.5 Prognostication ............................................................................................................. 14 -

Ciliary Body Melanoma
Central JSM Ophthalmology Case Report *Corresponding author Maria Luisa Gois da Fonseca, Department of Retina and Vitreous, Federal Fluminense University Niterói, Marques do Parana Avenue 303 Centro- Niterói, Brazil, Ciliary Body Melanoma: A Case Tel: 24033900 21 26299000; Email: [email protected] Submitted: 20 April 2020 Report With A Satisfactory Accepted: 29 April 2020 Published: 30 April 2020 Clinical Evolution ISSN: 2333-6447 Copyright Carolina Correa Leal Lima, Maria Luisa Gois da Fonseca*, © 2020 Leal Lima CC, et al. Guilherme Herzog Neto and Raul Nunes Galvarro Vianna OPEN ACCESS Department of Retina and Vitreous, Federal Fluminense University Niterói, Brazil Keywords Abstract • Melanoma • Oculoplastics Ciliary body melanomas are rare uveal disorders. Due to its anatomical location, it • Oncology is usually incidentally discovered in advanced stages. There is no established treatment • Ophthalmology for metastatic disease and the one-year survival rate of these patients is only fifteen • Uveal melanoma percent. We intend to report a case of ciliary body melanoma with good clinical outcomes. INTRODUCTION Ciliary body melanomas represent twelve percent of the uveal melanomas. Usually asymptomatic, it is incidentally discovered in the sixth decade of life. Owing to the anatomy of the eye, commonly the diagnosis is only made in advanced stages [1]. The present article intends to report a ciliary body melanoma case and literature review. CASE PRESENTATION Male, 80 years, one-eyed, right eye vision loss after a central retinal vein occlusion that evolved to neovascular glaucoma, has been attended at Federal Fluminense University Hospital Antonio Pedro for left eye (LE), cataracts surgery evaluation. At the Figure 1 Biomicroscopy illustrating vascularized hyperpigmented examination, best-corrected visual acuity (BCVA), was no light nodular lesion between bulbar conjunctiva and inferior tarsus in the perception right eye (RE), and 20/50 LE. -

Primary Cysts of the Iris
PRIMARY CYSTS OF THE IRIS BY Jerry A. Shields, MD INTRODUCTION PRIMARY IRIS CYSTS ARE RELATIVELY UNCOMMON, AND THERE HAVE BEEN NO LARGE studies which define the clinical characteristics and natural course of these lesions. The purpose of this thesis is to summarize the available literature on primary iris cysts, to review the clinical data on 62 affected patients who have been evaluated and followed by the author, and to document their clinical features with anterior segment photographs. On the basis of these observations, certain misconceptions in the literature regarding primary iris cysts will be challenged and a simple classification of such lesions will be proposed. DEFINITIONS For purposes of this report a cyst is defined as an epithelial-lined space. A primary iris cyst is an epithelial-lined space which involves a portion of the iris and which has no recognizable etiology. A secondary iris cyst is an epithelial-lined space which involves a portion of the iris and which has a recognizable etiology, such as surgical trauma, nonsurgical trauma, or miotic drugs. Such secondary iris cysts have already been thoroughly and accurately described in the literature. They will be included in the overall classification but will not be included in the statistical part of this report. REVIEW OF THE LITERATURE The literature on primary iris cysts is rather confusing because most reports have cited only a single example or a small series of patients and no writer has accumulated enough cases to classify the lesions into clini- cally meaningful categories. A review of the available literature indicated that such cysts may occur on the pupillary margin, in the posterior epithelial layer of the iris, or as free-floating cysts in the aqueous or vitreous chambers. -

Brachytherapy for Patients with Uveal Melanoma: Historical Perspectives and Future Treatment Directions
Journal name: Clinical Ophthalmology Article Designation: Review Year: 2018 Volume: 12 Clinical Ophthalmology Dovepress Running head verso: Brewington et al Running head recto: UM brachytherapy-early beginning to the molecular era open access to scientific and medical research DOI: 129645 Open Access Full Text Article REVIEW Brachytherapy for patients with uveal melanoma: historical perspectives and future treatment directions Beatrice Y Brewington1 Abstract: Surgical management with enucleation was the primary treatment for uveal melanoma Yusra F Shao2 (UM) for over 100 years. The Collaborative Ocular Melanoma Study confirmed in 2001 that Fredrick H Davidorf1 globe-preserving episcleral brachytherapy for UM was safe and effective, demonstrating Colleen M Cebulla1 no survival difference with enucleation. Today, brachytherapy is the most common form of radiotherapy for UM. We review the history of brachytherapy in the treatment of UM and the 1Havener Eye Institute, Department of Ophthalmology and Visual Science, evolution of the procedure to incorporate fine-needle-aspiration biopsy techniques with DNA- Ohio State University, 2Medical and RNA-based genetic prognostic testing. Student Research Program, The Ohio Keywords: brachytherapy, uveal melanoma, UM, fine-needle-aspiration biopsy, genetic State University College of Medicine, Columbus, OH, USA prognostic testing, molecular markers Introduction In the early 1900s, patients often presented with large, symptomatic uveal melanoma (UM), for which the primary course of treatment was enucleation. -

A Rare Case of Ciliary Body Melanoma Masquerading As Secondary Angle Closure Glaucoma
Jebmh.com Case Report A Rare Case of Ciliary Body Melanoma Masquerading as Secondary Angle Closure Glaucoma Farhad F. Mansuri1, Naitik Patel2, Somesh Aggarwal3 1Second Year Resident, Department of Ophthalmology, Western Regional Institute of Ophthalmology, Ahmedabad, Gujarat, India. 2Third Year Resident, Department of Ophthalmology, Western Regional Institute of Ophthalmology, Ahmedabad, Gujarat, India. 3Professor and HOD, Department of Ophthalmology, Western Regional Institute of Ophthalmology, Ahmedabad, Gujarat, India. INTRODUCTION Uveal melanoma is the most common primary malignancy of the eye in Caucasian Corresponding Author: adults, of which choroidal melanoma is the most common subtype.1 Ciliary body Dr. Somesh Aggarwal, melanoma is a rare tumour seen in 1 out of 10 cases of all intraocular melanomas Professor and HOD, Department of Ophthalmology, with an average age of 55 to 62 years.2, 3 Uveal melanoma arises from atypical Western Regional Institute of melanocytes present in iris, ciliary body and choroid, although each tumour has Ophthalmology, Ahmedabad, some particular characteristics depending on its location and structure. Because Gujarat, India. of the continuous contractions of the ciliary muscle and rich vascularization of the E-mail: [email protected] ciliary body, metastasis is faster in ciliary body melanoma.2 Vascular metastasis leads to impairment of other organs which is the main cause of death among ciliary DOI: 10.18410/jebmh/2020/430 body melanoma patients with 10 year mortality rate being 30-50%.2 Ciliary body melanoma has the worst prognosis of all intraocular tumours due to early How to Cite This Article: Mansuri FF, Patel N, Aggarwal S. A rare hematogenous metastasis which are frequently seen in the first year after case of ciliary body melanoma diagnosis.3 masquerading as secondary angle closure glaucoma. -

Ciliary Body Tumour Occuring in a Nigerian
Nigerian Journal of Ophthalmology 2008; 16(2): 60-63 Ciliary Body Tumour Occurring in a Nigerian - A case report ON Okonkwo MD, FRCSEd, DRCOphth; AO Hassan MD, FRCS, FRCOpth FWACS; O Oderinlo MD, FRCSEd, DRCOphth; F Oluyadi MD, FNMC, FWACS; AO Ogunro MD, FWACS; M Ulaikere MD, FWACS, FNMC; A Harriman MD, MRCOphth; S Oke MD, DWACS, MCEH Eye Foundation Retina Institute , Ijebu Imushin , Ogun State SUMMARY northern European descent. It is rarely seen among non white people. The incidence of ocular melanoma amongst Objective: To report the rare case of a 33-year-old female black peoples is extremely rare.3 Nigerian who presented to our retina clinic with a chronic total retinal detachment and visual acuity of no light CASE REPORT perception in her left eye. Re-attachment surgery in the eye was not attempted as prognosis for return of vision was poor. A 33-year old female Nigerian presented to the clinic with a She was later noted to harbor a progressively enlarging ciliary one-year history of poor vision and seeing of flashes of light body mass in the inferotemporal quadrant. in the left eye. The flashes of light predated the visual loss in Method: An observational case report was performed, with the left eye. She was referred to our clinic from another eye documentation of findings as patient was seen in the clinic. department after evaluation and investigation. The investigation included a B-scan ultrasonography, after which Conclusion: This is the first report of a ciliary body mass lesion she was diagnosed as a case of left eye posterior uveitis and in a Nigerian. -

Assessing Prognosis in Uveal Melanoma Uveal in Prognosis Assessing
cancercontroljournal.org Vol. 23, No. 2, April 2016 H. LEE MOFFITT CANCER CENTER & RESEARCH INSTITUTE, AN NCI COMPREHENSIVE CANCER CENTER Assessing Prognosis in Uveal Melanoma Zélia M. Corrêa, MD, PhD Therapeutic Options for Retinoblastoma Pia R. Mendoza, MD, and Hans E. Grossniklaus, MD Primary Vitreoretinal Lymphoma: Management of Isolated Ocular Disease Matthew T. Witmer, MD Management of Primary Acquired Melanosis, Nevus, and Conjunctival Melanoma Andrew Kao, MD, Armin Afshar, MD, Michele Bloomer, MD, et al Sebaceous Carcinoma of the Eyelid Carlos Prieto-Granada, MD, and Paul Rodriguez-Waitkus, MD, PhD Role of Vismodegib in the Management of Advanced Periocular Basal Cell Carcinoma Kyle F. Cox, MD, and Curtis E. Margo, MD Extranodal Marginal Zone B-cell Lymphoma of the Ocular Adnexa Jean Guffey Johnson, MD, Lauren A. Terpak, MS, Curtis E. Margo, MD, et al Ophthalmic Complications Related to Chemotherapy in Medically Complex Patients Lynn E. Harman, MD Cancer Control is included in Index Medicus/MEDLINE Permit No. 4390 No. Permit Jacksonville, FL FL Jacksonville, Tampa FL 33612-9416 FL Tampa P A I D I A P 12902 Magnolia Drive Magnolia 12902 U.S. POSTAGE U.S. & RESEARCH INSTITUTE INC INSTITUTE RESEARCH & NON-PROFIT ORG NON-PROFIT CENTER CANCER MOFFITT LEE H Editorial Board Members Editor: Richard D. Kim, MD Production Team: Associate Member Veronica Nemeth Lodovico Balducci, MD Gastrointestinal Oncology Senior Member Editorial Coordinator Bela Kis, MD, PhD Program Leader, Senior Adult Oncology Program Sherri Damlo Assistant Member Moffitt Cancer Center Medical Copy Editor Diagnostic Radiology Diane McEnaney Rami Komrokji, MD Deputy Editor: Graphic Design Consultant Associate Member Julio M.