A Structured Approach to Skin and Soft Tissue Infections (Sstis) in an Ambulatory Setting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abscess Prevention
ABSCESS PREVENTION ▪ Chest pains may occur if infection How do you soak/use Avoiding abscesses goes to heart or lungs compresses? • Wash your hands and the injection site. What should I do if I get ▪ Use warm/hot water (that doesn’t burn your skin) • Use alcohol pads and wipe an abscess? ▪ Soak in tub of plain hot water or hot back & forth (rub hard) over ▪ Treat at home with warm soaks water with Epsom salts injection site to remove dirt. only if: ▪ Use hot, wet, clean washcloth and - No red streaks hold on abscess, if abscess cannot • Then use another new alcohol - Skin not hot and puffy be soaked in tub pad for the final cleaning. ▪ Soak abscess 3 to 4 times a day for ▪ Go to a clinic if abscess: 10-15 minutes each time, if possible What is a skin abscess? - Not improving, especially ▪ Cover with a clean dry bandage after after 5-7 days soaking ▪ Pocket of pus - Gets bigger and/or very ▪ soaking/using compresses ▪ Often found at injection sites, but STOP painful when abscess starts draining can be found elsewhere - Is hot and puffy ▪ More likely with Red streaks start spreading skin-popping from the abscess-go ASAP! muscling What about missing a vein ▪ Go to emergency room if: ▪ May occur even after you stop Chest pain antibiotics? injecting High fever, chills ▪ Take all antibiotics, if Infection looks like it is How do you know it’s an spreading fast prescribed, even if you feel better abscess? ▪ Take antibiotics after you fix (if ▪ using heroin) ▪ Pink or reddish lump on skin ▪ Do not take antibiotics with ▪ Tender or painful Warning -

Toxic Shock Syndrome Contributors: Noah Craft MD, Phd, Lindy P
** no patient handout Toxic shock syndrome Contributors: Noah Craft MD, PhD, Lindy P. Fox MD, Lowell A. Goldsmith MD, MPH SynopsisToxic shock syndrome (TSS) is a severe exotoxin-mediated bacterial infection that is characterized by high fevers, headache, pharyngitis, vomiting, diarrhea, and hypotension. Two subtypes of TSS exist, based on the bacterial etiology: Staphylococcus aureus and group A streptococci. Significantly, the severity of TSS can range from mild disease to rapid progression to shock and end organ failure. The dermatologic manifestations of TSS include the following: • Erythema of the palms and soles that desquamates 1-3 weeks after the initial onset • Diffuse scarlatiniform exanthem that begins on the trunk and spreads toward the extremities • Erythema of the mucous membranes (strawberry tongue and conjunctival hyperemia) TSS was identified in and most commonly affected menstruating young white females using tampons in the 1980s. Current TSS cases are seen in post-surgical interventions in men, women, and children, as well as in other settings, in addition to cases of menstrual TSS, which have declined with increased public education on tampon usage and TSS. One study in Japanese patients found the highest TSS incidence to occur among children with burns, as Staphylococcus colonization is high in this subgroup and antibody titers are not yet sufficient to protect children from the exotoxins causing TSS. Staphylococcal TSS is caused by S. aureus strains that can produce the toxic shock syndrome toxin-1 (TSST-1). TSST-1 is believed to cause disease via direct effects on end organs, impairing clearance of gut flora derived endotoxins, with TSST-1 acting as a superantigen leading to massive nonspecific activation of T-cells and subsequent inflammation and vascular leakage. -

Gas Gangrene Infection of the Eyes and Orbits
Br J Ophthalmol: first published as 10.1136/bjo.69.2.143 on 1 February 1985. Downloaded from British Journal of Ophthalmology, 1985, 69, 143-148 Gas gangrene infection of the eyes and orbits GERARD W CROCK,' WILSON J HERIOT,' PATTABIRAMAN JANAKIRAMAN,' AND JOHN M WEINER2 From the 'Department of Ophthalmology, University ofMelbourne, and the2C H Greer Pathology Laboratory, the Royal Victorian Eye and Ear Hospital, East Melbourne, Australia SUMMARY The literature on Clostridium perfringens infections is reviewed up to 1983. An additional case is reported with bilateral clostridial infections of the eye and orbit. One eye followed the classical course of relentless panophthalmitis, amaurosis, and orbital cellulitis ending in enucleation. The second eye contained intracameral mud and gas bubbles that were removed by vitrectomy instrumentation. Subsequent removal of the toxic cataract resulted in a final aided visual acuity of 6/18, N8. This is the third report of a retained globe, and we believe the only known case where the patient was left with useful vision. Clostridium perfringens is a ubiquitous Gram- arms, chest, and abdomen. He was admitted to a positive bacillus found in soil and bowel flora. It is the general hospital, where he was examined under most common of four clostridia species identified in anaesthesia, and his injuries were attended to. copyright. cases of gas gangrene in man.' All species are obligate Ocular findings. The right cornea and anterior anaerobes and are usually saprophytic rather than chamber were intact. There was a scleral laceration pathogenic. Clostridium perfringens is a feared con- over the superonasal area of the pars plana with taminant of limb injuries and may result in death due vitreous prolapse. -

Investigation of Anthrax Associated with Intentional Exposure
October 19, 2001 / Vol. 50 / No. 41 889 Update: Investigation of Anthrax Associated with Intentional Exposure and Interim Public Health Guidelines, October 2001 893 Recognition of Illness Associated with the Intentional Release of a Biologic Agent 897 Weekly Update: West Nile Virus Activity — United States, October 10–16, 2001 Update: Investigation of Anthrax Associated with Intentional Exposure and Interim Public Health Guidelines, October 2001 On October 4, 2001, CDC and state and local public health authorities reported a case of inhalational anthrax in Florida (1 ). Additional cases of anthrax subsequently have been reported from Florida and New York City. This report updates the findings of these case investigations, which indicate that infections were caused by the intentional release of Bacillus anthracis. This report also includes interim guidelines for postexposure pro- phylaxis for prevention of inhalational anthrax and other information to assist epidemi- ologists, clinicians, and laboratorians responding to intentional anthrax exposures. For these investigations, a confirmed case of anthrax was defined as 1) a clinically compatible case of cutaneous, inhalational, or gastrointestinal illness* that is laboratory confirmed by isolation of B. anthracis from an affected tissue or site or 2) other labora- tory evidence of B. anthracis infection based on at least two supportive laboratory tests. A suspected case was defined as 1) a clinically compatible case of illness without isola- tion of B. anthracis and no alternative diagnosis, but with laboratory evidence of B. anthracis by one supportive laboratory test or 2) a clinically compatible case of an- thrax epidemiologically linked to a confirmed environmental exposure, but without cor- roborative laboratory evidence of B. -

Naeglaria and Brain Infections
Can bacteria shrink tumors? Cancer Therapy: The Microbial Approach n this age of advanced injected live Streptococcus medical science and into cancer patients but after I technology, we still the recipients unfortunately continue to hunt for died from subsequent innovative cancer therapies infections, Coley decided to that prove effective and safe. use heat killed bacteria. He Treatments that successfully made a mixture of two heat- eradicate tumors while at the killed bacterial species, By Alan Barajas same time cause as little Streptococcus pyogenes and damage as possible to normal Serratia marcescens. This Alani Barajas is a Research and tissue are the ultimate goal, concoction was termed Development Technician at Hardy but are also not easy to find. “Coley’s toxins.” Bacteria Diagnostics. She earned her bachelor's degree in Microbiology at were either injected into Cal Poly, San Luis Obispo. The use of microorganisms in tumors or into the cancer therapy is not a new bloodstream. During her studies at Cal Poly, much idea but it is currently a of her time was spent as part of the undergraduate research team for the buzzing topic in cancer Cal Poly Dairy Products Technology therapy research. Center studying spore-forming bacteria in dairy products. In the late 1800s, German Currently she is working on new physicians W. Busch and F. chromogenic media formulations for Fehleisen both individually Hardy Diagnostics, both in the observed that certain cancers prepared and powdered forms. began to regress when patients acquired accidental erysipelas (cellulitis) caused by Streptococcus pyogenes. William Coley was the first to use New York surgeon William bacterial injections to treat cancer www.HardyDiagnostics.com patients. -
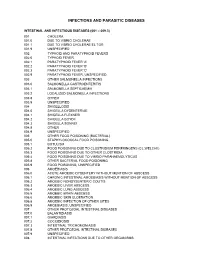
Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -
![Nonbacterial Pus-Forming Diseases of the Skin Robert Jackson,* M.D., F.R.C.P[C], Ottawa, Ont](https://docslib.b-cdn.net/cover/6901/nonbacterial-pus-forming-diseases-of-the-skin-robert-jackson-m-d-f-r-c-p-c-ottawa-ont-246901.webp)
Nonbacterial Pus-Forming Diseases of the Skin Robert Jackson,* M.D., F.R.C.P[C], Ottawa, Ont
Nonbacterial pus-forming diseases of the skin Robert Jackson,* m.d., f.r.c.p[c], Ottawa, Ont. Summary: The formation of pus as a Things are not always what they seem Fungus result of an inflammatory response Phaedrus to a bacterial infection is well known. North American blastomycosis, so- Not so well appreciated, however, The purpose of this article is to clarify called deep mycosis, can present with a is the fact that many other nonbacterial the clinical significance of the forma¬ verrucous proliferating and papilloma- agents such as certain fungi, viruses tion of pus in various skin diseases. tous plaque in which can be seen, par- and parasites may provoke pus Usually the presence of pus in or on formation in the skin. Also heat, the skin indicates a bacterial infection. Table I.Causes of nonbacterial topical applications, systemically However, by no means is this always pus-forming skin diseases administered drugs and some injected true. From a diagnostic and therapeutic Fungus materials can do likewise. Numerous point of view it is important that physi¬ skin diseases of unknown etiology cians be aware of the nonbacterial such as pustular acne vulgaris, causes of pus-forming skin diseases. North American blastomycosis pustular psoriasis and pustular A few definitions are required. Pus dermatitis herpetiformis can have is a yellowish [green]-white, opaque, lymphangitic sporotrichosis bacteriologically sterile pustules. The somewhat viscid matter (S.O.E.D.). Pus- cervicofacial actinomycosis importance of considering nonbacterial forming diseases are those in which Intermediate causes of pus-forming conditions of pus can be seen macroscopicaily. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Preoperative Skin Antisepsis with Chlorhexidine Gluconate Versus Povidone-Iodine: a Prospective Analysis of 6959 Consecutive Spinal Surgery Patients
CLINICAL ARTICLE J Neurosurg Spine 28:209–214, 2018 Preoperative skin antisepsis with chlorhexidine gluconate versus povidone-iodine: a prospective analysis of 6959 consecutive spinal surgery patients George M. Ghobrial, MD, Michael Y. Wang, MD, Barth A. Green, MD, Howard B. Levene, MD, PhD, Glen Manzano, MD, Steven Vanni, DO, DC, Robert M. Starke, MD, MSc, George Jimsheleishvili, MD, Kenneth M. Crandall, MD, Marina Dididze, MD, PhD, and Allan D. Levi, MD, PhD Department of Neurological Surgery and The Miami Project to Cure Paralysis, University of Miami Miller School of Medicine, Miami, Florida OBJECTIVE The aim of this study was to determine the efficacy of 2 common preoperative surgical skin antiseptic agents, ChloraPrep and Betadine, in the reduction of postoperative surgical site infection (SSI) in spinal surgery proce- dures. METHODS Two preoperative surgical skin antiseptic agents—ChloraPrep (2% chlorhexidine gluconate and 70% iso- propyl alcohol) and Betadine (7.5% povidone-iodine solution)—were prospectively compared across 2 consecutive time periods for all consecutive adult neurosurgical spine patients. The primary end point was the incidence of SSI. RESULTS A total of 6959 consecutive spinal surgery patients were identified from July 1, 2011, through August 31, 2015, with 4495 (64.6%) and 2464 (35.4%) patients treated at facilities 1 and 2, respectively. Sixty-nine (0.992%) SSIs were observed. There was no significant difference in the incidence of infection between patients prepared with Beta- dine (33 [1.036%] of 3185) and those prepared with ChloraPrep (36 [0.954%] of 3774; p = 0.728). Neither was there a significant difference in the incidence of infection in the patients treated at facility 1 (52 [1.157%] of 4495) versus facility 2 (17 [0.690%] of 2464; p = 0.06). -

Incision & Drainage Informed Consent
Jeri Shuster, M.D., P.A. and Women’s Center, Inc. JERI SHUSTER, M.D., PA & WOMEN’SJeri Shuster, CENTER, INC M.D.,. P.A. Jeri Shuster, M.D., Fellowand of the Women’s American CollegeCenter, Obstetricians Inc. and Gynecologists Kathryn Cervi, C.R.N.P., Women’s Health Care Nurse Practitioner Jeri Shuster, M.D., Fellow of the American College Obstetricians and Gynecologists INFORMED CONSENT: Kathryn INCISION Cervi, C.R.N.P., AND Women’s DRAINAGE Health (I Care & D) Nurse Practitioner I hereby request and authorize Dr. to Jeri Shuster perform upon me the procedure: incision and drainage of _________________________________________________________________________ _____________________________________________________________________________________________ This procedure involves making an incision, either with a scalpel or with an electrical device, in order to enable fluid to drain from an area of the body. The procedure is intended to drain a cyst(s), abscess(es), or infected tissue. Risks include: bleeding, infection, burn injury, pain, scarring, failure to diagnose or cure the underlying condition, persistence or recurrence of the condition. To reduce risk of infection, after the procedure keep area as clean and dry as possible. Wash three times each day with lukewarm water and mild soap. Dry by gently dabbing with a soft wel to or carefully use a blow dryer on the cool setting. Follow each wash/dry with antibacterial ointment (such as Neosporin or Bacitracin). If genital incision and drainage ou is performed, y may also place antibiotic ointment onto cotton balls (not cosmetic puffs) to cover the wounds during urination or bowel movements. Benefits may include achieving a diagnosis (by distinguishing between a cyst and an abscss) and alleviating symptoms such as pain. -

Sexually Transmitted Diseases
Sexually Transmitted Diseases by John H. Dirckx, M.D. significant proportion of the modern practice of adult using condoms and avoiding high-risk behaviors such as anal gynecology and urology is devoted to the prevention, intercourse—and by limiting the number of sex partners. Adiagnosis, and treatment of sexually transmitted dis- The overall incidence of sexually transmitted infections eases (STDs), because of both the high prevalence of these has increased substantially during the past generation, and diseases and their almost exclusive involvement of the repro- some diseases have shown a marked increase. Several factors ductive systems in both sexes. have contributed to these changing statistics. The discovery in A sexually transmitted disease is any infectious disease the 1940s that penicillin could cure syphilis and gonorrhea and that is transmitted from one person to another through sexual the development during the 1950s of safe and effective oral contact, taking that phrase in its broadest sense. Venereal dis- contraceptives paved the way for the sexual revolution of the ease (VD), a synonymous term, has now largely fallen out of 1960s. Against a background of civil unrest, widespread drug use, as has the euphemism social disease. It is worth empha- abuse, and radical feminism, that revolution led to social sizing that the only thing all STDs have in common is their acceptance of sexual promiscuity, popularization of oral and mode of transmission. In other respects they vary widely anal sex, and definition of overt homosexuality as normal among themselves. The common tendency to lump them all behavior. together yields a biologically invalid concept that invites con- Other factors favoring sexual promiscuity have been the fusion and misunderstanding. -

Abscesses Are a Serious Problem for People Who Shoot Drugs
Where to Get Your Abscess Seen Abscesses are a serious problem for people who shoot drugs. But what the hell are they and where can you go for care? What are abscesses? Abscesses are pockets of bacteria and pus underneath you skin and occasionally in your muscle. Your body creates a wall around the bacteria in order to keep the bacteria from infecting your whole body. Another name for an abscess is a “soft tissues infection”. What are bacteria? Bacteria are microscopic organisms. Bacteria are everywhere in our environment and a few kinds cause infections and disease. The main bacteria that cause abscesses are: staphylococcus (staff-lo-coc-us) aureus (or-e-us). How can you tell when you have an abscess? Because they are pockets of infection abscesses cause swollen lumps under the skin which are often red (or in darker skinned people darker than the surrounding skin) warm to the touch and painful (often VERY painful). What is the worst thing that can happen? The worst thing that can happen with abscesses is that they can burst under your skin and cause a general infection of your whole body or blood. An all over bacterial infection can kill you. Another super bad thing that can happen is a endocarditis, which is an infection of the lining of your heart, and “septic embolism”, which means that a lump of the contaminates in your abscess get loose in your body and lodge in your lungs or brain. Why do abscesses happen? Abscesses are caused when bad bacteria come in to contact with healthy flesh.