DM SEMINAR August 18, 2006
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Addressing Highly Hazardous Pesticides in Mozambique
República de Moçambique Ministério da Agricultura e Segurança Alimentar Direcção Nacional de Agricultura e Silvicultura Addressing Highly Hazardous Pesticides in Mozambique Addressing Highly Hazardous Pesticides in Mozambique Food and Agriculture Organization of the United Nations Rome, 2016 The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations (FAO) concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or products of manufacturers, whether or not these have been patented, does not imply that these have been endorsed or recommended by FAO in preference to others of a similar nature that are not mentioned. The views expressed in this information product are those of the author(s) and do not necessarily reflect the views or policies of FAO. ISBN 978-92-5-108519-6 © FAO, 2016 FAO encourages the use, reproduction and dissemination of material in this information product. Except where otherwise indicated, material may be copied, downloaded and printed for private study, research and teaching purposes, or for use in non-commercial products or services, provided that appropriate acknowledgement of FAO as the source and copyright holder is given and that FAO’s endorsement of users’ views, products or services is not implied in any way. All requests for translation and adaptation rights, and for resale and other commercial use rights should be made via www.fao.org/contact-us/licence-request or addressed to [email protected]. -

Recommended Classification of Pesticides by Hazard and Guidelines to Classification 2019 Theinternational Programme on Chemical Safety (IPCS) Was Established in 1980
The WHO Recommended Classi cation of Pesticides by Hazard and Guidelines to Classi cation 2019 cation Hazard of Pesticides by and Guidelines to Classi The WHO Recommended Classi The WHO Recommended Classi cation of Pesticides by Hazard and Guidelines to Classi cation 2019 The WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification 2019 TheInternational Programme on Chemical Safety (IPCS) was established in 1980. The overall objectives of the IPCS are to establish the scientific basis for assessment of the risk to human health and the environment from exposure to chemicals, through international peer review processes, as a prerequisite for the promotion of chemical safety, and to provide technical assistance in strengthening national capacities for the sound management of chemicals. This publication was developed in the IOMC context. The contents do not necessarily reflect the views or stated policies of individual IOMC Participating Organizations. The Inter-Organization Programme for the Sound Management of Chemicals (IOMC) was established in 1995 following recommendations made by the 1992 UN Conference on Environment and Development to strengthen cooperation and increase international coordination in the field of chemical safety. The Participating Organizations are: FAO, ILO, UNDP, UNEP, UNIDO, UNITAR, WHO, World Bank and OECD. The purpose of the IOMC is to promote coordination of the policies and activities pursued by the Participating Organizations, jointly or separately, to achieve the sound management of chemicals in relation to human health and the environment. WHO recommended classification of pesticides by hazard and guidelines to classification, 2019 edition ISBN 978-92-4-000566-2 (electronic version) ISBN 978-92-4-000567-9 (print version) ISSN 1684-1042 © World Health Organization 2020 Some rights reserved. -

A Review of Aluminium Phosphide Poisoning and a Flowchart to Treat It Arh Hig Rada Toksikol 2016;67:183-193 183
Hashemi-Domeneh, et al. A review of aluminium phosphide poisoning and a flowchart to treat it Arh Hig Rada Toksikol 2016;67:183-193 183 Review DOI: 10.1515/aiht-2016-67-2784 A review of aluminium phosphide poisoning and a flowchart to treat it Behrooz Hashemi-Domeneh1,2, Nasim Zamani1,2, Hossein Hassanian-Moghaddam1,2, Mitra Rahimi1,2, Shahin Shadnia1,2, Peyman Erfantalab1,2, and Ali Ostadi1,2 Toxicological Research Center, Department of Clinical Toxicology, Loghman-Hakim Hospital, Shahid Beheshti University of Medical Sciences1, Excellence Center of Clinical Toxicology, Iranian Ministry of Health2, Tehran, Iran [Received in February 2016; CrossChecked in February 2016; Accepted in September 2016] The use of pesticides such as aluminium phosphide (AlP) has increased in the recent years and improved the quantity and quality of agricultural products in a number of developing countries. The downside is that AlP causes severe chronic and acute health effects that have reached major proportions in countries such as India, Iran, Bangladesh, and Jordan. Nearly 300,000 people die due to pesticide poisoning in the world every year. Poisoning with AlP accounts for many of these deaths. Unfortunately, at the same time, there is no standard treatment for it. The aim of this article is to give a brief review of AlP poisoning and propose a treatment flowchart based on the knowledge gained so far. For this purpose we reviewed all articles on the management of AlP poisoning published from 2000 till now. Using a modified Delphi design, we have designed a handy flowchart that could be used as a guide for AlP poisoning management of patients in emergency centres. -
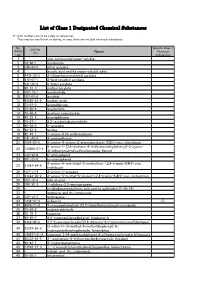
List of Class 1 Designated Chemical Substances
List of Class 1 Designated Chemical Substances *1:CAS numbers are to be solely as references. They may be insufficient or lacking, in case there are multiple chemical substances. No. Specific Class 1 CAS No. (PRTR Chemical (*1) Name Law) Substances 1 - zinc compounds(water-soluble) 2 79-06-1 acrylamide 3 140-88-5 ethyl acrylate 4 - acrylic acid and its water-soluble salts 5 2439-35-2 2-(dimethylamino)ethyl acrylate 6 818-61-1 2-hydroxyethyl acrylate 7 141-32-2 n-butyl acrylate 8 96-33-3 methyl acrylate 9 107-13-1 acrylonitrile 10 107-02-8 acrolein 11 26628-22-8 sodium azide 12 75-07-0 acetaldehyde 13 75-05-8 acetonitrile 14 75-86-5 acetone cyanohydrin 15 83-32-9 acenaphthene 16 78-67-1 2,2'-azobisisobutyronitrile 17 90-04-0 o-anisidine 18 62-53-3 aniline 19 82-45-1 1-amino-9,10-anthraquinone 20 141-43-5 2-aminoethanol 21 1698-60-8 5-amino-4-chloro-2-phenylpyridazin-3(2H)-one; chloridazon 5-amino-1-[2,6-dichloro-4-(trifluoromethyl)phenyl]-3-cyano- 22 120068-37-3 4[(trifluoromethyl)sulfinyl]pyrazole; fipronil 23 123-30-8 p-aminophenol 24 591-27-5 m-aminophenol 4-amino-6-tert-butyl-3-methylthio-1,2,4-triazin-5(4H)-one; 25 21087-64-9 metribuzin 26 107-11-9 3-amino-1-propene 27 41394-05-2 4-amino-3-methyl-6-phenyl-1,2,4-triazin-5(4H)-one; metamitron 28 107-18-6 allyl alcohol 29 106-92-3 1-allyloxy-2,3-epoxypropane 30 - n-alkylbenzenesulfonic acid and its salts(alkyl C=10-14) 31 - antimony and its compounds 32 120-12-7 anthracene 33 1332-21-4 asbestos ○ 34 4098-71-9 3-isocyanatomethyl-3,5,5-trimethylcyclohexyl isocyanate 35 78-84-2 isobutyraldehyde -

Hazardous Waste Classification
HAZARDOUS WASTE CLASSIFICATION: REVIEW OF WORST CASE TO LESS WORST CASE METAL SPECIES WITH A WORKED EXAMPLE FOR A CONTAMINATED SOIL Ian Bishop 1,* and Pierre Hennebert 2 1 One Touch Data Ltd, Suite 4, Third Floor, Nicholsons House, Nicholsons Walk, Maidenhead SL6 1LD, United Kingdom 2 INERIS (National Institute for Industrial Environment and Risks), BP 2, F-60550 Verneuil-en-Halatte, France Article Info: ABSTRACT Received: The classification of waste as either hazardous or non-hazardous, especially for mix- 28 October 2020 Revised: tures such as contaminated soils, ashes, filter cakes and sludges, is not straight for- 17 February 2021 ward. In particular, as the laboratories can only measure total metal concentrations, Accepted: both the European and the UK technical guidance state that if the classifier doesn’t 25 February 2021 know exactly which metal species is in their waste, then they should start from a Available online: worst case species and use lines of evidence to work towards a more reasonable 31 March 2021 (less hazardous) species. However, the guidance doesn’t define or list worst case Keywords: nor less worst case species. While some authors have documented worst case spe- Hazardous properties cies, this is only in relation to documenting the concentrations at which each hazard Worst case Metal species property is triggered for a given worst case species. This paper addresses this gap. It documents how to define both the worst case species and more importantly, lists less worst case species for 32 elements and 204 metal species; species based on those listed in the European legislation but also supplemented by species that hav- en’t (yet) been included in this legislation but are significant nevertheless. -

Chemical Names and CAS Numbers Final
Chemical Abstract Chemical Formula Chemical Name Service (CAS) Number C3H8O 1‐propanol C4H7BrO2 2‐bromobutyric acid 80‐58‐0 GeH3COOH 2‐germaacetic acid C4H10 2‐methylpropane 75‐28‐5 C3H8O 2‐propanol 67‐63‐0 C6H10O3 4‐acetylbutyric acid 448671 C4H7BrO2 4‐bromobutyric acid 2623‐87‐2 CH3CHO acetaldehyde CH3CONH2 acetamide C8H9NO2 acetaminophen 103‐90‐2 − C2H3O2 acetate ion − CH3COO acetate ion C2H4O2 acetic acid 64‐19‐7 CH3COOH acetic acid (CH3)2CO acetone CH3COCl acetyl chloride C2H2 acetylene 74‐86‐2 HCCH acetylene C9H8O4 acetylsalicylic acid 50‐78‐2 H2C(CH)CN acrylonitrile C3H7NO2 Ala C3H7NO2 alanine 56‐41‐7 NaAlSi3O3 albite AlSb aluminium antimonide 25152‐52‐7 AlAs aluminium arsenide 22831‐42‐1 AlBO2 aluminium borate 61279‐70‐7 AlBO aluminium boron oxide 12041‐48‐4 AlBr3 aluminium bromide 7727‐15‐3 AlBr3•6H2O aluminium bromide hexahydrate 2149397 AlCl4Cs aluminium caesium tetrachloride 17992‐03‐9 AlCl3 aluminium chloride (anhydrous) 7446‐70‐0 AlCl3•6H2O aluminium chloride hexahydrate 7784‐13‐6 AlClO aluminium chloride oxide 13596‐11‐7 AlB2 aluminium diboride 12041‐50‐8 AlF2 aluminium difluoride 13569‐23‐8 AlF2O aluminium difluoride oxide 38344‐66‐0 AlB12 aluminium dodecaboride 12041‐54‐2 Al2F6 aluminium fluoride 17949‐86‐9 AlF3 aluminium fluoride 7784‐18‐1 Al(CHO2)3 aluminium formate 7360‐53‐4 1 of 75 Chemical Abstract Chemical Formula Chemical Name Service (CAS) Number Al(OH)3 aluminium hydroxide 21645‐51‐2 Al2I6 aluminium iodide 18898‐35‐6 AlI3 aluminium iodide 7784‐23‐8 AlBr aluminium monobromide 22359‐97‐3 AlCl aluminium monochloride -

Proposing Boric Acid As an Antidote for Aluminium Phosphide Poisoning by Investigation of the Chemical Reaction Between Boric Acid and Phosphine
Journal of Medical Hypotheses and Ideas (2013) 7, 21–24 Available online at www.sciencedirect.com Journal of Medical Hypotheses and Ideas journal homepage: www.elsevier.com/locate/jmhi REGULAR ARTICLES Proposing boric acid as an antidote for aluminium phosphide poisoning by investigation of the chemical reaction between boric acid and phosphine Motahareh Soltani a, Seyed Farid Shetab-Boushehri b, Hamidreza Mohammadi c, Seyed Vahid Shetab-Boushehri d,* a Department of Toxicology, Ahar Branch, Islamic Azad University, Ahar, Iran b Novin Kavosh Mamatir, 20th Street, Kaveh Industrial Zone, Saveh, Iran c Department of Clinical Toxicology, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran d Department of Clinical Toxicology, School of Medicine and Razi Drug Research Center, Tehran University of Medical Sciences, P.O. Box: 14155-5983, Tehran, Iran Received 5 November 2012; revised 27 November 2012; accepted 28 November 2012 KEYWORDS Abstract Aluminium phosphide (AlP) is a storage fumigant pesticide, which is used to protect Aluminium phosphide stored grains especially from insects and rodents. It releases phosphine (PH3) gas, a highly toxic poisoning; mitochondrial poison, in contact with moisture, particularly if acidic. Although the exact mecha- Phosphine gas; nism of action is unknown so far, the major mechanism of PH3 toxicity seems to be the inhibition Trapping agent; of cytochrome-c oxidase and oxidative phosphorylation which eventually results in adenosine tri- Antidote; phosphate (ATP) depletion and cell death. Death due to AlP poisoning seems to be as a result Boric acid of myocardial damage. No efficient antidote has been found for AlP poisoning so far, and unfor- tunately, most of the poisoned human cases die. -

Disposal of Persistent Organic Pollutants and Obsolete Pesticides and Strengthening Sound Pesticide Management in Cameroon” Project Evaluation Series 01/2020
Project Evaluation Series 01/2020 Mid-term evaluation of the project “Disposal of persistent organic pollutants and obsolete pesticides and strengthening sound pesticide management in Cameroon” Project Evaluation Series 01/2020 Mid-term evaluation of the project “Disposal of persistent organic pollutants and obsolete pesticides and strengthening sound pesticide management in Cameroon” Project code: GCP/CMR/031/GFF GEF ID: 4641 FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Rome, 2020 Required citation: FAO. 2020. Mid-term evaluation of the project “Disposal of persistent organic pollutants and obsolete pesticides and strengthening sound pesticide management in Cameroon”. Project evaluation series, 01/2020. Rome. https://doi.org/10.4060/ca7489en. The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations (FAO) concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or products of manufacturers, whether or not these have been patented, does not imply that these have been endorsed or recommended by FAO in preference to others of a similar nature that are not mentioned. The views expressed in this information product are those of the author(s) and do not necessarily reflect the views or policies of FAO. © FAO, 2020 Some rights reserved. This work is made available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo/legalcode/legalcode). -

Recognition and Management of Pesticide Poisonings: Sixth Edition: 2013: Chapter 17 Fumigants
CHAPTER 17 HIGHLIGHTS Easily absorbed in lung, gut, skin Fumigants SIGNS & SYMPTOMS Packaging and formulation of fumigants are complex. Those that are gases at room Highly variable among temperature (methyl bromide, ethylene oxide, sulfur dioxide, sulfuryl fluoride) are agents provided in compressed gas cylinders. Liquids are marketed in cans or drums. Solids that sublime, such as naphthalene, must be packaged so as to prevent significant Many are irritants contact with air before they are used. Sodium cyanide is only available in an encap- Carbon disulfide, chloroform, sulated form so that when wild canids attack livestock their bite releases the poison. ethylene dichloride, Mixtures of fumigants are sometimes used. For instance, chloropicrin, which has hydrogen cyanide, methyl a strong odor and irritant effect, is often added as a “warning agent” to other liquid bromide may have serious fumigants. It is important to be aware of the possibility of such mixtures. CNS effects Liquid halocarbons and carbon disulfide evaporate into the air while naphtha- lene sublimes. Paraformaldehyde slowly depolymerizes to formaldehyde. Aluminum Methyl bromide, ethylene phosphide slowly reacts with water vapor in the air to liberate phosphine, an extremely dibromide, ethylene oxide, toxic gas. aluminum phosphide Fumigants have remarkable capacities for diffusion (a property essential to (phosphine gas) can cause their function). Some readily penetrate rubber and neoprene personal protective gear, pulmonary edema as well as human skin. They are rapidly absorbed across the pulmonary membranes, Chloroform, carbon gastrointestinal tract and skin. Special adsorbents are required in respirator canisters tetrachloride, ethylene to protect exposed workers from airborne fumigant gases. Even these may not provide dichloride, ethylene complete protection when air concentrations of fumigants are high. -

Aluminium Phosphide Releasing Phosphine Product-Type 20 (Control of Other Vertebrates) September 2013
Regulation (EU) n°528/2012 concerning the making available on the market and use of biocidal products Evaluation of active substances Assessment Report Aluminium phosphide releasing phosphine Product-type 20 (Control of other vertebrates) September 2013 Germany Aluminium phosphide releasing phosphine (PT 20) Assessment report Finalised in the Standing Committee on Biocidal Products at its meeting on 27 September 2013 CONTENTS 1. STATEMENT OF SUBJECT MATTER AND PURPOSE .................................. 4 1.1. Principle of evaluation .................................................................................... 4 1.2. Purpose of the assessment ............................................................................... 4 1.3. Procedure followed .......................................................................................... 5 2. OVERALL SUMMARY AND CONCLUSIONS ................................................... 7 2.1. Presentation of the Active Substance ............................................................. 7 2.1.1. Identity, Physico-Chemical Properties & Methods of Analysis ....... 7 2.1.2. Intended Uses and Efficacy ................................................................ 8 2.1.3. Classification and Labelling .............................................................. 9 2.2. Summary of the Risk Assessment ................................................................ 17 2.2.1. Human Health Risk Assessment ...................................................... 17 2.2.1.1. Effects assessment ............................................................................ -

Aluminium Phosphide-Induced Hepato-Nephrotoxicity and Oxidative Damage in Rats: the Protective Effect of Α-Lipoic Acid
Send Orders for Reprints to [email protected] 18 The Open Conference Proceedings Journal, 2015, 6, 18-23 Open Access Aluminium Phosphide-induced Hepato-nephrotoxicity and Oxidative Damage in Rats: The Protective Effect of -lipoic Acid Mokhtar I. Yousef, Naglaa F. Soliman*, Fatma M. El-Demerdash Department of Environmental Studies, Institute of Graduate Studies and Research, Alexandria University, Alexandria, Egypt Abstract: The present experiment was carried out to investigate the effectivness of -lipoic acid in allevating the toxicity of aluminium phosphide on biochemical parameters, free radicals and enzyme activities in plasma, liver and kidney of male rats. Animals were orally treated with aluminium phosphide, -lipoic acid and their combination for 30 consecutive days. Treatment with aluminium phosphide led to significant decrease in plasma total protein and glucose and increase in transaminases, phosphatases, urea, creatinine and bilirubin. Treatment with aluminium phosphide significantly decreased glutathione S-transferase (GST), catalase (CAT) and reduced glutathione (GSH) in plasma, liver and kidney. While, thiobarbituric acid reactive substances (TBARS; as an index of lipid peroxidation) and superoxide dismutase (SOD) were increased in plasma, liver and kidney of rats treated with aluminium phosphide. Administration of -lipoic acid in combination with aluminium phosphide minimized and alleviated its toxic effects on most of the measured parameters. In conclusion, lipoic acid has beneficial effects and could be able to attenuate aluminium phosphide toxicity. Keywords: Aluminium Phosphide, -Lipoic Acid, Antioxidants, Lipid peroxidation, Biochemical parameters, Rats. 1. INTRODUCTION catalase, peroxidase and glutathione [8, 9]. Oxidative stress is one of the main mechanisms of action of aluminium Aluminium phosphide is used as a pesticide and it is phosphide toxicity [10]. -

The APPPC Sub-Regional Training Workshop for the Dnas on the Rotterdam Convention Focusing On
REPORT APPPC SUB-REGIONAL TRAINING WORKSHOP FOR THE DESIGNATED NATIONAL AUTHORITIES ON THE ROTTERDAM CONVENTION FOCUSING ON INCREASING NOTIFICATIONS 13-17 MARCH 2017, SURABAYA, INDONESIA Executive Summary The APPPC Sub-regional Training Workshop for the DNAs on the Rotterdam Convention Focusing on Increasing Notifications was held from 13-17 March, 2017 in Surabaya, Indonesia and was attended by 33 participants from 9 countries. The main purpose of the workshop was to improve countries capacity in the implementation of the Convention, with the specific objective of strengthening DNAs in preparing notifications of FRA and SHPF, and also to increase the number of submission and improve the completeness of the information provided. The workshop provided training on the key elements of the Rotterdam Convention with special emphasis in strengthening and updating their knowledge on how to meet the obligation in submitting notification of FRA and SHPF. The status of import responses of the Annex III chemicals for each country was also discussed, and the participants were accordingly informed on the need to take action on pending responses. Participants became more knowledgeable on the provisions of the Rotterdam Convention and the latest status of its implementation through paper presentations during the workshop. During the exercise in the breakout groups, participants were also exposed to various forms and how to complete them in order to familiarize and facilitate them in making submission. Participants took part actively in the discussion during breakout and plenary sessions, and they exchanged knowledge, experiences and clarified issues and pointed to areas that need special attention. Among the issues discussed at length were on the need for an improved coordination and communication channel between DNAs and other relevant stakeholders at national level, so that all the requirements in meeting various obligations under the Convention are effectively decided.