Wound Healing and the Use of Medicinal Plants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Herbal Recipes for Preventing and Addressing Upper Respiratory
1 Herbal Recipes for Preventing and Addressing Upper Respiratory Infections by Rosalee de la Forêt 2 Text by Rosalee de la Forêt. Illustrations by Tatiana Rusakova ©2020 Rosalee de la Forêt, LLC. All rights reserved. No part of this publication may be reproduced in whole or in part, or stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without written permission of the author. The herbal and plant information in this ebook is for educational purposes only. The information within the ebook is not intended as a substitute for the advice provided by your physician or other medical professional. If you have or suspect that you have a serious health problem, promptly contact your health care provider. Always consult with a health care practitioner before using any herbal remedy or food, especially if pregnant, nursing, or have a medical condition. Published by Rosalee de la Forȇt, LLC, Methow Valley, WA First digital edition, March 2020. Published in the U.S.A 3 Astragalus Immune-Building Chai 4 Strong Elderberry Tea 5 Parsley & Garlic Gremolata 6 Garlic-Infused Honey 7 Kid’s Immune Support Tea 8 Elderflower and Yarrow Tea 9 Strong Chamomile Tea 10 Cayenne Tea 11 Healthy Lungs Tea 12 Looking for herbs? 13 About Rosalee 14 4 Astragalus Immune-Building Chai I drink a version of this throughout the winter months and attribute it to my good health. It’s spicy, sweet, delicious and is best when taken daily for an extended period of time. Ingredients 30 grams dried Astragalus root (A. -
Supplementstop for Immune Support
SUPPLEMENTSTOP FOR IMMUNE SUPPORT Three Generation’s of Truth in Nutrition Table of Contents 3 1 Maintaining healthy immune function 6 2 Sleep and mental health 9 3 The one-two punch for pain, inflammation 11 4 Four ways to provide a virus-season boost and maintaining a healthy gut microbiota 13 5 Essential vitamins and minerals for overall good health 2 1 Maintaining healthy immune function Poor immune systems causing record work losses According to a new study published in the September 2019 issue of the Journal of Occupational and Environmental Medicine, nearly one-fifth of working adults will experience a cold each year. The study estimated 20 million annual missed workdays might be just the tip of the iceberg, because the estimates include only colds that resulted in doctor’s visits or restricted activity days. There may be as many as 70 million lost workdays due to colds, when actual missed work time is combined with lost productivity. Past flu seasons likely cost employers nationwide millions of lost workdays and billions of dollars. Nearly 111 million workdays are lost due to the flu each year, There may be as many as according to Flu.gov, costing employers approximately $7 billion per year in sick days and lost productivity. 70 million lost workdays The study also found Americans spend nearly $3 billion annually on over- due to colds, when the-counter drugs that may not provide any symptom relief. actual missed work time Since the 1940s, studies have shown the use of botanicals and nutritional supplements may both prevent and reduce the effects of common colds and is combined with lost influenza and support immune cell function and promote respiratory health.* productivity. -

URAT1 for J Ethnopharmacol Figures2
O O O O O O O O coumarin 7-methoxycoumarin OH HO osthol O O O O HO O O 4-hydroxycoumarin 6-hydroxycoumarin umbelliferone HO O HO O O HO O O HO O O HO O O OH OH daphnetin esculetin fraxetin osthenol OH O O OH O O O O O bergaptol bergamottin geraniol Figure S1. Chemical structures of the compounds used as samples in this study. Original ABC F GED Original IH KJ L NM Figure S2. TLC pattern of the fractions collected from the hexane crude fraction. The hexane crude fraction (3.0 g) was applied to open silica gel chromatography eluted with hexane:acetone (8:2), and the fractions A–N were collected. Each fraction (3 µg) was spotted to TLC plate, spread out with hexane:acetone (8:2), and colored with anisaldehyde reagent. “Original” means the original hexane crude fraction. Large single spot in the fraction F is osthol. Table S1. The origin, distributer name, lot number of the sample, and the ratio yielded of crude drugs used. Latin name of crude drug Origin Distributera) Lot # Ratio yielded (%)b) Achyranthis Radix The dried root of Achyranthes bidentata Blume Tsumura 22026591 9.4 Akebiae Caulis The dried climbing stem of Akebia quinata Decaisne Tsumura 23006161 4.2 Alismatis Rhizoma The dried tuber of Alisma plantago-aquatica subsp. orientale (Sampaio) Sampaio Tsumura 22043631 6.8 Alpiniae Officinari Rhizoma The dried rhizome of Alpinia officinarum Hance Tsumura 23011641 9.0 Amomi Semen The dried seed mass of Amomum villosum var. xanthioides (Wall. ex Baker) T.L.Wu & S.J.Chen Tsumura 22042491 1.2 Anemarrhenae Rhizoma The dried rhizome of Anemarrhena asphodeloides Bunge Tsumura 23005341 16.8 Angelicae Dahuricae Radix The dried root of Angelica dahurica Benth. -

Medicinal Plants Used in the Treatment of Human Immunodeficiency Virus
International Journal of Molecular Sciences Review Medicinal Plants Used in the Treatment of Human Immunodeficiency Virus Bahare Salehi 1,2 ID , Nanjangud V. Anil Kumar 3 ID , Bilge ¸Sener 4, Mehdi Sharifi-Rad 5,*, Mehtap Kılıç 4, Gail B. Mahady 6, Sanja Vlaisavljevic 7, Marcello Iriti 8,* ID , Farzad Kobarfard 9,10, William N. Setzer 11,*, Seyed Abdulmajid Ayatollahi 9,12,13, Athar Ata 13 and Javad Sharifi-Rad 9,13,* ID 1 Medical Ethics and Law Research Center, Shahid Beheshti University of Medical Sciences, 88777539 Tehran, Iran; [email protected] 2 Student Research Committee, Shahid Beheshti University of Medical Sciences, 22439789 Tehran, Iran 3 Department of Chemistry, Manipal Institute of Technology, Manipal University, Manipal 576104, India; [email protected] 4 Department of Pharmacognosy, Gazi University, Faculty of Pharmacy, 06330 Ankara, Turkey; [email protected] (B.¸S.);[email protected] (M.K.) 5 Department of Medical Parasitology, Zabol University of Medical Sciences, 61663-335 Zabol, Iran 6 PAHO/WHO Collaborating Centre for Traditional Medicine, College of Pharmacy, University of Illinois, 833 S. Wood St., Chicago, IL 60612, USA; [email protected] 7 Department of Chemistry, Biochemistry and Environmental Protection, Faculty of Sciences, University of Novi Sad, Trg Dositeja Obradovica 3, 21000 Novi Sad, Serbia; [email protected] 8 Department of Agricultural and Environmental Sciences, Milan State University, 20133 Milan, Italy 9 Phytochemistry Research Center, Shahid Beheshti University of -

The Use of Chinese Yang/ Qi-Invigorating Tonic Botanical Drugs/ Herbal Formulations in Ameliorating Chronic Kidney Disease by Enhancing Mitochondrial Function
REVIEW published: 24 June 2021 doi: 10.3389/fphar.2021.622498 The Use of Chinese Yang/ Qi-Invigorating Tonic Botanical Drugs/ Herbal Formulations in Ameliorating Chronic Kidney Disease by Enhancing Mitochondrial Function Jiayi Tian 1,2†, Yuqi Huang 1,2†, Tong Wu 1,2, Hsien-Da Huang 2,3, Kam Ming Ko 4*, Bao Ting Zhu 1,2* and Jihang Chen 1,2* 1Shenzhen Key Laboratory of Steroid Drug Discovery and Development, School of Life and Health Sciences, The Chinese University of Hong Kong, Shenzhen, China, 2School of Life and Health Sciences, The Chinese University of Hong Kong, Edited by: Shenzhen, China, 3Warshel Institute for Computational Biology, The Chinese University of Hong Kong, Shenzhen, China, 4Division Uraiwan Panich, of Life Science, The Hong Kong University of Science & Technology, Hong Kong, China Mahidol University, Thailand Reviewed by: Mingjiang Yao, Background: Chronic kidney disease (CKD) is a leading cause of morbidity and mortality. Xiyuan Hospital, China Mitochondrial dysfunction has been implicated as a key factor in the development of CKD. Rodrigo Castaneda, According to traditional Chinese medicine (TCM) theory, many Chinese Yang/Qi- Universidad de San Carlos de Guatemala, Guatemala invigorating botanical drugs/herbal formulations have been shown to produce *Correspondence: promising outcomes in the clinical management of CKD. Experimental studies have Jihang Chen indicated that the health-promoting action of Yang/Qi invigoration in TCM is related to [email protected] Bao Ting Zhu the up-regulation of mitochondrial energy generation and antioxidant status. [email protected] Kam Ming Ko Objective: In this review, we aim to test whether Chinese Yang/Qi-invigorating tonic [email protected] botanical drugs/herbal formulations can provide medical benefits in CKD and its †These authors have contributed complications. -
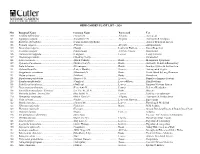
HERB GARDEN PLANT LIST – 2020 NO. Botanical Name Common
HERB GARDEN PLANT LIST – 2020 NO. Botanical Name Common Name Parts used Use 100 Achillea millefolium ……………………........………......(Yarrow) N ………………………......…......All parts …………….........Astringent 101 Aquilegia vulgaris………………………......…...............(Columbine) N ........…………...….............. All parts………..………....Astringent & Analgesic 102 Buddleia alternafolia....…………...…………...........…..(Fountain Butterfly Bush)………………..................................................Attracts Beneficial Insects 103 Primula vulgaris....………………...………...……..........(Primrose)………………………...…...........All parts………...………...Antispasmodic 104 Tanacetum vulgaris……………...……….............…..….(Tansy)……………….......………..…....…..Leaves & Flowers...............Insect Repellent 105 Aconitum vulgaris...……………...………………............(Monkshood)…………………......…….......All Parts Unsafe.........…....Ornamental 106 Pulmonaria longifolia..........……………...…...…..........(Lungwort)…………………......……….......Leaves.....…………...….....Lung Ailments 107 Dicentra spectabilis…….….…….…….…....…....…..….(Bleeding Heart)....……......…………………………….....…………….Ornamental 108 Actea racemose..…………….……………...…...........….(Black Cohosh)…….………...….............….Roots......…...…….………Menopausal Symptoms 109 Hydrastis Canadensis..............………......………..........(Golden Seal) N....………….......…..……….Roots………….…………..Antibiotic & Anti-inflammatory 110 Inula helenium......................…………………………….(Elecampane) .....…..........………………….Roots……………………..Immune System & Antibacteria 111 Alchemilla mollis....................…………………...………(Lady’s -

Herbal Advancements in the Treatment to Accelerate Wound Healing
ISSN 2226-3063 e-ISSN 2227-9555 Modern Phytomorphology 15: 76–8 1, 2021 REVIEW ARTICLE Herbal advancements in the treatment to accelerate wound healing Lovely School of Applied Medical Sciences Shyam Bass*, Sheetu, Asees Kaur School of Pharmaceutical Sciences, Lovely Professional University, Jalandhar, Punjab, India; * [email protected] Received: 11.05.2021 | Accepted: 15.06.2021 | Published: 23.06.2021 Abstract An injury or a wound is an anatomical and functional disturbance to the tissue. Wound healing is a complicated mechanism of tissue regeneration or remodelling that occurs in response to an injury. Plants and plant-derived constituents have long been used to heal and handle various forms of wounds. Currently, various forms of biopolymers are being studied in order to create a cost-effective, long-lasting, durable, and reliable delivery mechanism for the treatment of wounds. Wound treatment providers have revisited ancient healing practices by using conventional and complementary medicine in wound recovery due to the rise of multi-resistant pathogens and a decline in modern antibiotics. People’s attitudes toward alternative medicine have shifted as well, which is very positive. The idea of moist wound healing has gained a lot of attraction, and conventional medicine has begun to use it to speed up the healing process. In wound care treatment, several experiments using herbal and conventional medicine from various continents have been published. Keywords: Alternative medicine, complementary medicine, traditional medicine, wound -

On the Metabolism and Transport of Anticancer Drugs
Effects of Complementary and Alternative Medicines (CAM) on the Metabolism and Transport of Anticancer Drugs KIM MOOIMAN Cover design: Kim Mooiman Lay-out & printing: Optima Grafische Communicatie, Rotterdam, The Netherlands Mooiman, K.D. Effects of Complementary and Alternative Medicines (CAM) on the Metabolism and Transport of Anticancer Drugs ISBN/EAN: 978-94-6169-457-7 © 2013 Kim Mooiman Effects of Complementary and Alternative Medicines (CAM) on the Metabolism and Transport of Anticancer Drugs Effecten van complementaire en alternatieve geneesmiddelen op het metabolisme en transport van oncolytica (met een samenvatting in het Nederlands) PROEFSCHRIFT ter verkrijging van de graad van doctor aan de Universiteit Utrecht op gezag van de rector magnificus, prof. dr. G.J. van der Zwaan, ingevolge het besluit van het college voor promoties in het openbaar te verdedigen op woensdag 18 december 2013 des middags te 2.30 uur door Kim Delia Mooiman geboren op 22 mei 1986 te Woerden Promotoren: Prof. dr. J.H.M. Schellens Prof. dr. J.H. Beijnen Co-promotor: Dr. ir. I. Meijerman The research described in this thesis was performed at the Department of Pharmaceuti- cal Sciences, Division of Pharmacoepidemiology & Clinical Pharmacology of the Utrecht University in Utrecht, The Netherlands. Furthermore, part of the research was performed at the Department of Clinical Pharmacology of the Netherlands Cancer Institute in Amsterdam, and at the Department of Pharmacy and Pharmacology of the Slotervaart Hospital in Amsterdam, The Netherlands. Financial support by the Utrecht Institute for Pharmaceutical Sciences (UIPS), The Neth- erlands Laboratory for Anticancer Drug Formulation (NLADF), Shimadzu Benelux B.V. and the Dutch Cancer Society for the publication of this thesis is gratefully acknowledged. -

Research on Plants with Medicinal Properties in Suriname Dennis R.A
Clinical and Medical Investigations Review Article ISSN: 2398-5763 “Nature, green in leaf and stem”. Research on plants with medicinal properties in Suriname Dennis R.A. Mans* Department of Pharmacology, Faculty of Medical Sciences, Anton de Kom University of Suriname, USA Abstract The widely held layman’s perception of nature as a collection of animals operating against a static green background of plants is a serious misunderstanding of the complexity and dynamics of the plant biodiversity. Plants fulfill all functions that superficially only seem reserved for animals including movement, communication, and defense. For the latter purposes, plants have developed intricate and highly sophisticated chemical warning signals and defense systems to alarm friends and ward off foes. Many of these plant substances possess meaningful pharmacological properties, and some were found useful against human diseases. This paper briefly describes several aspects of plant communication and defense; gives a few examples of plant-derived therapeutics; and focuses on the potential contribution of Suriname (South America) to this scientific area. Background organs of the plant and transport seeds away from the parent plant, enabling its propagation and the colonization of new niches, receiving The view of the plant kingdom as a green and static background valuable sources of food in return [7]. for moving animals - particularly (higher) vertebrates - is far from the reality. Paraphrasing Alfred, Lord Tennyson’s (1809-1892) words “Tho’ Other means of plant communication are so-called semiochemicals, nature, red in tooth and claw” in his poem ‘In Memoriam A.H.H.’, plant substances involved in the transfer of information between plants the American author, physician, producer, director, and screenwriter and other organisms [8]. -

Supplementary Appendix for the Origin and Early Evolution of The
Supplementary Appendix for The Origin and Early Evolution of the Legumes are a Complex Paleopolyploid Phylogenomic Tangle closely associated with the Cretaceous-Paleogene (K-Pg) Boundary Authors: Erik J.M. Koenen1*, Dario I. Ojeda2,3, Royce Steeves4,5, Jérémy Migliore2, Freek Bakker6, Jan J. Wieringa7, Catherine Kidner8,9, Olivier Hardy2, R. Toby Pennington8,10, Patrick S. Herendeen11, Anne Bruneau4 and Colin E. Hughes1 1 Department of Systematic and Evolutionary Botany, University of Zurich, Zollikerstrasse 107, CH-8008, Zurich, Switzerland 2 Service Évolution Biologique et Écologie, Faculté des Sciences, Université Libre de Bruxelles, Avenue Franklin Roosevelt 50, 1050, Brussels, Belgium 3 Norwegian Institute of Bioeconomy Research, Høgskoleveien 8, 1433 Ås, Norway 4 Institut de Recherche en Biologie Végétale and Département de Sciences Biologiques, Université de Montréal, 4101 Sherbrooke St E, Montreal, QC H1X 2B2, Canada 5 Fisheries & Oceans Canada, Gulf Fisheries Center, 343 Université Ave, Moncton, NB E1C 5K4, Canada 6 Biosystematics Group, Wageningen University, Droevendaalsesteeg 1, 6708 PB, Wageningen, The Netherlands 7 Naturalis Biodiversity Center, Leiden, Darwinweg 2, 2333 CR, Leiden, The Netherlands 8 Royal Botanic Gardens, 20a Inverleith Row, Edinburgh EH3 5LR, U.K. 9School of Biological Sciences, University of Edinburgh, King’s Buildings, Mayfield Rd, Edinburgh, UK 10 Geography, University of Exeter, Amory Building, Rennes Drive, Exeter, EX4 4RJ, U.K. 11 Chicago Botanic Garden, 1000 Lake Cook Rd, Glencoe, IL 60022, U.S.A. * Correspondence to be sent to: Zollikerstrasse 107, CH-8008, Zurich, Switzerland; phone: +41 (0)44 634 84 16; email: [email protected]. Methods S1. Discussion on fossils used for calibrating divergence time analyses. -

Asia Is the Mine of Natural Antiviral Products for Public Health
58 The Open Complementary Medicine Journal, 2009, 1, 58-68 Open Access Asia is the Mine of Natural Antiviral Products for Public Health R.R. Hafidh1, A.S. Abdulamir1, F. Jahanshiri2, F. Abas1,3, F. Abu Bakar1,3,* and Z. Sekawi4 1Institue of Bioscience; 2Department of Microbiology, Faculty of Biotechnology and Biomolecular Sciences; 3Department of Food Science, Faculty of Food Science and Technology and 4Department of Medical Microbiology and Parasitology, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, 43400 UPM Serdang, Selangor Darul Ehsan, Malaysia Abstract: This review highlights a wide range of research on antiviral natural products in Asia in the period from 2000 to 2008. It focuses on the most important findings in this field specifically on the plants' components with potential antiviral activity against wide range of pathogenic DNA and RNA viruses. In addition, the difference between Asians and other populations regarding their habits of using natural products containing antiviral activity instead of allopathic medicine has been reviewed briefly. In conclusion, Asian continent serves as the most important source for providing the candidate natural products for the future antiviral drugs which could save the lives of millions in the world. Key Words: Antiviral, alternative medicine, polyphenols, flavonoids, tannin, anti-RNA virus, anti-DNA virus and Asia. INTRODUCTION [10]. Interestingly, most of the plant species have shown strong positive ethnopharmacological correlation with the There is a long history of medicinal use of plants in traditional knowledge [6]. The ethnopharmacology knowl- Asian countries, some of which have proved useful to hu- mans as pharmaceuticals. Asia seems to be the most promis- edge serve as an innovative and powerful discovery engine for newer, safer and affordable medicines [11]. -

Flavonoids from Astragalus Propinquus
Available online www.jocpr.com Journal of Chemical and Pharmaceutical Research, 2013, 5(1):261-265 ISSN : 0975-7384 Research Article CODEN(USA) : JCPRC5 Flavonoids from Astragalus propinquus Venkata Sai Prakash Chaturvedula* and Indra Prakash Organic Chemistry Department, The Coca-Cola Company, Global Research and Development, One Coca-Cola Plaza, Atlanta, GA 30313, USA _____________________________________________________________________________________________ ABSTRACT Systematic phytochemical studies of the dichloromethane (CH 2Cl 2) fraction of the aqueous extract of Astragalus propinquus on a C-18 column using a Biotage Flash Chromatography system yielded three flavonoids namely 5- hydroxy-4´, 6, 7 trimethoxyflavone (salvigenin), 4´, 5, 7-trihydroxyflavone (apigenin), and 3´,4´, 5, 7- tetrhydroxyflavone (luteolin). The structures of the isolated compounds salvigenin, apigenin, and luteolin were characterized on the basis of extensive spectral studies and literature search. Further, the complete 1H and 13 C NMR spectral assignments of the three isolated compounds are reported on the basis of 1D ( 1H and 13 C) and 2D (COSY, HSQC, and HMBC) NMR spectral data. Keywords: Astragalus propinquus , Fabaceae, Flavonoids, NMR, MS, Structure elucidation _____________________________________________________________________________________________ INTRODUCTION Astragalus root is a staple of Traditional Chinese Medicine (TCM), where it is also known as Huang Qi . It is considered a sweet, warming herb with many medicinal propreties. Traditionally it is used in the treatment of fatigue, decreased appetite, general debility (particularly in the elderly), susceptibility to viral infections, non- healing wounds, fever, sweating, uterine prolapse, uterine bleeding, edema (nephritis), numbness, muscle pain, diabetes mellitus, and uterine, ovarian or colon cancer [1]. Astragalus is a component of numerous traditional medicine tonics and is often combined with ginseng, angelica, licorice and other herbs.