Plasminogen Activators (Activity of Variant Tissue Plasminogen Activators/Domains of Tissue Plasminogen Activator/Effectors of Fibrinolysis) SHOKO URANO, ALAN R
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Clinical Protocol
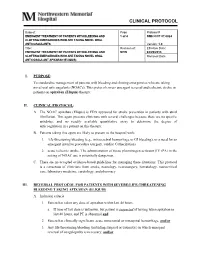
CLINICAL PROTOCOL Subject: Page Protocol # EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND 1 of 4 NMH CCP 07.0024 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL ANTICOAGULANTS Version: 1.0 Title: Revision of: Effective Date: EMERGENT TREATMENT OF PATIENTS WITH BLEEDING AND NEW 04/29/2013 CLOTTING EMERGENCIES WHO ARE TAKING NOVEL ORAL Removal Date: ANTICOAGULANT APIXABAN (ELIQUIS) I. PURPOSE: To standardize management of patients with bleeding and clotting emergencies who are taking novel oral anticoagulants (NOACs). This protocol covers emergent reversal and ischemic stroke in patients on apixaban (Eliquis) therapy. II. CLINICAL PROTOCOL: A. The NOAC apixaban (Eliquis) is FDA approved for stroke prevention in patients with atrial fibrillation. This agent presents clinicians with several challenges because there are no specific antidotes, and no readily available quantitative assay to determine the degree of anticoagulation in a patient on this therapy. B. Patients taking this agent are likely to present to the hospital with; 1. life-threatening bleeding (e.g., intracerebral hemorrhage or GI bleeding), or a need for an emergent invasive procedure (surgery, cardiac Catherization) 2. acute ischemic stroke. The administration of tissue plasminogen activator (IV tPA) in the setting of NOAC use is potentially dangerous. C. There are no accepted evidence-based guidelines for managing these situations. This protocol is a consensus of clinicians from stroke, neurology, neurosurgery, hematology, neurocritical care, laboratory medicine, cardiology, and pharmacy. III. REVERSAL PROTOCOL FOR PATIENTS WITH SEVERE/LIFE-THREATENING BLEEDING TAKING APIXABAN (ELIQUIS) A. Inclusion criteria: 1. Patient has taken any dose of apixaban within last 48 hours. a. If time of last dose is unknown, but patient is suspected of having taken apixaban in last 48 hours, and PT is abnormal and 2. -

The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’S Perspective
International Journal of Molecular Sciences Review The Central Role of Fibrinolytic Response in COVID-19—A Hematologist’s Perspective Hau C. Kwaan 1,* and Paul F. Lindholm 2 1 Division of Hematology/Oncology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA 2 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; [email protected] * Correspondence: [email protected] Abstract: The novel coronavirus disease (COVID-19) has many characteristics common to those in two other coronavirus acute respiratory diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). They are all highly contagious and have severe pulmonary complications. Clinically, patients with COVID-19 run a rapidly progressive course of an acute respiratory tract infection with fever, sore throat, cough, headache and fatigue, complicated by severe pneumonia often leading to acute respiratory distress syndrome (ARDS). The infection also involves other organs throughout the body. In all three viral illnesses, the fibrinolytic system plays an active role in each phase of the pathogenesis. During transmission, the renin-aldosterone- angiotensin-system (RAAS) is involved with the spike protein of SARS-CoV-2, attaching to its natural receptor angiotensin-converting enzyme 2 (ACE 2) in host cells. Both tissue plasminogen activator (tPA) and plasminogen activator inhibitor 1 (PAI-1) are closely linked to the RAAS. In lesions in the lung, kidney and other organs, the two plasminogen activators urokinase-type plasminogen activator (uPA) and tissue plasminogen activator (tPA), along with their inhibitor, plasminogen activator 1 (PAI-1), are involved. The altered fibrinolytic balance enables the development of a hypercoagulable Citation: Kwaan, H.C.; Lindholm, state. -

Assembly of an Integrated Human Lung Cell Atlas Reveals That
medRxiv preprint doi: https://doi.org/10.1101/2020.06.02.20120634; this version posted June 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Assembly of an integrated human lung cell atlas reveals that SARS-CoV-2 receptor is co-expressed with key elements of the kinin-kallikrein, renin-angiotensin and coagulation systems in alveolar cells Davi Sidarta-Oliveira1,2, Carlos Poblete Jara1,3, Adriano J. Ferruzzi4, Munir S. Skaf4, William H. Velander5, Eliana P. Araujo1,3, Licio A. Velloso1 1Laboratory of Cell Signaling, Obesity and Comorbidities Research Center, University of Campinas, Brazil 2 Physician-Scientist Graduate Program, School of Medical Sciences, University of Campinas, Brazil 3Nursing School, University of Campinas, Brazil 4Institute of Chemistry and Center for Computing in Engineering and Sciences University of Campinas, Brazil 5Department of Chemical and Biomolecular Engineering, University of Nebraska, Lincoln, USA Correspondence: Licio A. Velloso Laboratory of Cell Signaling, Obesity and Comorbidities Research Center, University of Campinas, Campinas, Brazil Address: Rua Carl Von Lineaus s/n, Instituto de Biologia - Bloco Z. Campus Universitário Zeferino Vaz - Barão Geraldo, Campinas - SP, 13083-864 Phone: +55 19 3521-0025 E-mail: [email protected] Abstract SARS-CoV-2, the pathogenic agent of COVID-19, employs angiotensin converting enzyme-2 (ACE2) as its cell entry receptor. Clinical data reveal that in severe COVID- 19, SARS-CoV-2 infects the lung, leading to a frequently lethal triad of respiratory insufficiency, acute cardiovascular failure, and coagulopathy. -

The Plasmin–Antiplasmin System: Structural and Functional Aspects
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Bern Open Repository and Information System (BORIS) Cell. Mol. Life Sci. (2011) 68:785–801 DOI 10.1007/s00018-010-0566-5 Cellular and Molecular Life Sciences REVIEW The plasmin–antiplasmin system: structural and functional aspects Johann Schaller • Simon S. Gerber Received: 13 April 2010 / Revised: 3 September 2010 / Accepted: 12 October 2010 / Published online: 7 December 2010 Ó Springer Basel AG 2010 Abstract The plasmin–antiplasmin system plays a key Plasminogen activator inhibitors Á a2-Macroglobulin Á role in blood coagulation and fibrinolysis. Plasmin and Multidomain serine proteases a2-antiplasmin are primarily responsible for a controlled and regulated dissolution of the fibrin polymers into solu- Abbreviations ble fragments. However, besides plasmin(ogen) and A2PI a2-Antiplasmin, a2-Plasmin inhibitor a2-antiplasmin the system contains a series of specific CHO Carbohydrate activators and inhibitors. The main physiological activators EGF-like Epidermal growth factor-like of plasminogen are tissue-type plasminogen activator, FN1 Fibronectin type I which is mainly involved in the dissolution of the fibrin K Kringle polymers by plasmin, and urokinase-type plasminogen LBS Lysine binding site activator, which is primarily responsible for the generation LMW Low molecular weight of plasmin activity in the intercellular space. Both activa- a2M a2-Macroglobulin tors are multidomain serine proteases. Besides the main NTP N-terminal peptide of Pgn physiological inhibitor a2-antiplasmin, the plasmin–anti- PAI-1, -2 Plasminogen activator inhibitor 1, 2 plasmin system is also regulated by the general protease Pgn Plasminogen inhibitor a2-macroglobulin, a member of the protease Plm Plasmin inhibitor I39 family. -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death -

Plasmin (Human) 1.00 Mg
Plasmin (Human) 1.00 mg Ref#: HPLAS Lot#: xxxxxx Exp. Date: xxxx-xx Store at -10°C to -20°C For Research Use Only Not for Use in Diagnostic Procedures For in vitro use only Description: Plasmin Format: Frozen in 50mM Hepes/ 50 mM sodium acetate/ 50% glycerol/ pH 8.5 Host: Human Storage: Store between -10°C and -20°C Volume: 1 vial containing 0.962 mL Total Protein: 1.00 mg 1% Concentration: 1.04 mg/mL by Absorbance; Extinction Coefficient E 280 = 17.0 Activity: 228.00 nkat/mg Molecular weight: 83000 daltons Plasminogen is synthesized in the liver and circulates in plasma at a concentration of ~200 μg/mL (~2.3 μM). Plasminogen is a single-chain glycoprotein of ~88 kDa that consists of a catalytic domain followed by five kringle structures. Within these kringle structures are four low-affinity lysine binding sites and one high-affinity lysine binding site. It is through these lysine binding sites that plasminogen binds to fibrin and to α2-Antiplasmin. Native Plasminogen (Glu-Plasminogen) exists in two variants that differ in their extent of glycosylation, and each variant has up to six isoelectric forms with respect to sialic acid content, for a total of 12 molecular forms. Activation of Glu-Plasminogen by the Plasminogen activators Urokinase (UPA), or tissue Plasminogen Activator (tPA) occurs by cleavage after residue Arg560 to produce the two-chain active serine protease Plasmin. In a positive feedback reaction, the Plasmin generated cleaves an ~8 kDa peptide from Glu-Plasminogen, producing lys77- Plasminogen which has a higher affinity for Fibrin and when bound is a preferred substrate for Plasminogen activators such as Urokinase. -

A First in Class Treatment for Thrombosis Prevention. a Phase I
Journal of Cardiology and Vascular Medicine Research Open Access A First in Class Treatment for Thrombosis Prevention. A Phase I study with CS1, a New Controlled Release Formulation of Sodium Valproate 1,2* 2 3 2 1,2 Niklas Bergh , Jan-Peter Idström , Henri Hansson , Jonas Faijerson-Säljö , Björn Dahlöf 1Department of Molecular and Clinical Medicine, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden 2 Cereno Scientific AB, Gothenburg, Sweden 3 Galenica AB, Malmö, Sweden *Corresponding author: Niklas Bergh, The Wallenberg Laboratory for Cardiovascular Research Sahlgrenska University Hospi- tal Bruna Stråket 16, 413 45 Göteborg, Tel: +46 31 3421000; E-Mail: [email protected] Received Date: June 11, 2019 Accepted Date: July 25, 2019 Published Date: July 27, 2019 Citation: Niklas Bergh (2019) A First in Class Treatment for Thrombosis Prevention? A Phase I Study With Cs1, a New Con- trolled Release Formulation of Sodium Valproate. J Cardio Vasc Med 5: 1-12. Abstract Several lines of evidence indicate that improving fibrinolysis by valproic acid may be a fruitful strategy for throm- bosis prevention. This study investigated the safety, pharmacokinetics, and effect on biomarkers for thrombosis of CS1, a new advanced controlled release formulation of sodium valproate designed to produce optimum valproic acid concen- trations during the early morning hours, when concentrations of plasminogen activator inhibitor (PAI)-1 and the risk of thrombotic events is highest. Healthy volunteers (n=17) aged 40-65 years were randomized to receive single doses of one of three formulations of CS1 (FI, FII, and FIII). The CS1 FII formulation showed the most favorable pharmacokinetics and was chosen for multiple dosing. -

6. Interaction Between the Coagulation and Complement System
6. Interaction Between the Coagulation and Complement System Umme Amara1, Daniel Rittirsch 1, Michael Flierl 1, Uwe Bruckner 2, Andreas Klos 3, Florian Gebhard1, John D. Lambris4, and Markus Huber-Lang1,* 1Department of Traumatology, Hand-, Plastic-, and Reconstructive Surgery, University Hospital of Ulm, Ulm, Germany, [email protected] 2Division of Experimental Surgery, University Hospital of Ulm, Ulm, Germany, [email protected] 3Department of Medical Microbiology, Medical School Hannover, Hannover, Germany, [email protected] 4Department of Pathology, University of Pennsylvania, 401 Stellar Chance, Philadelphia, PA 19104, USA, [email protected]. Abstract. The complement system as a main column of innate immunity and the coagulation system as a main column in hemostasis undergo massive activation early after injury. Interactions between the two cascades have often been proposed but the precise molecular pathways of this interplay are still in the dark. To elucidate the mechanisms involved, the effects of various coagulation factors on complement activation and generation of anaphylatoxins were investigated and summarized in the light of the latest literature. Own in vitro findings suggest, that the coagulation factors FXa, FXIa and plasmin may cleave both C5 and C3, and robustly generate C5a and C3a (as detected by immunoblotting and ELISA). The produced anaphylatoxins were found to be biologically active as shown by a dose- dependent chemotactic response of neutrophils and HMC-1 cells, respectively. Thrombin did not only cleave C5 (Huber-Lang et al. 2006) but also in vitro-generated C3a when incubated with native C3. The plasmin-induced cleavage activity could be dose-dependently blocked by the serine protease inhibitor aprotinin and leupeptine. -

Activation of the Plasma Kallikrein-Kinin System in Respiratory Distress Syndrome
003 I-3998/92/3204-043 l$03.00/0 PEDIATRIC RESEARCH Vol. 32. No. 4. 1992 Copyright O 1992 International Pediatric Research Foundation. Inc. Printed in U.S.A. Activation of the Plasma Kallikrein-Kinin System in Respiratory Distress Syndrome OLA D. SAUGSTAD, LAILA BUP, HARALD T. JOHANSEN, OLAV RPISE, AND ANSGAR 0. AASEN Department of Pediatrics and Pediatric Research [O.D.S.].Institute for Surgical Research. University of Oslo [L.B.. A.O.A.], Rikshospitalet, N-0027 Oslo 1, Department of Surgery [O.R.],Oslo City Hospital Ullev~il University Hospital, N-0407 Oslo 4. Department of Pharmacology [H. T.J.],Institute of Pharmacy, University of Oslo. N-0316 Oslo 3, Norway ABSTRAm. Components of the plasma kallikrein-kinin proteins that interact in a complicated way. When activated, the and fibrinolytic systems together with antithrombin 111 contact factors plasma prekallikrein, FXII, and factor XI are were measured the first days postpartum in 13 premature converted to serine proteases that are capable of activating the babies with severe respiratory distress syndrome (RDS). complement, fibrinolytic, coagulation, and kallikrein-kinin sys- Seven of the patients received a single dose of porcine tems (7-9). Inhibitors regulate and control the activation of the surfactant (Curosurf) as rescue treatment. Nine premature cascades. C1-inhibitor is the most important inhibitor of the babies without lung disease or any other complicating contact system (10). It exerts its regulatory role by inhibiting disease served as controls. There were no differences in activated FXII, FXII fragment, and plasma kallikrein (10). In prekallikrein values between surfactant treated and non- addition, az-macroglobulin and a,-protease inhibitor inhibit treated RDS babies during the first 4 d postpartum. -

Original Article Endogenous Risk Factors for Deep-Vein Thrombosis in Patients with Acute Spinal Cord Injuries
Spinal Cord (2007) 45, 627–631 & 2007 International Spinal Cord Society All rights reserved 1362-4393/07 $30.00 www.nature.com/sc Original Article Endogenous risk factors for deep-vein thrombosis in patients with acute spinal cord injuries S Aito*,1, R Abbate2, R Marcucci2 and E Cominelli1 1Spinal Unit, Careggi University Hospital, Florence, Italy; 2Medical division, coagulation disease, Careggi University Hospital, Florence, Italy Study design: Case–control study. Aim of the study: Investigate the presence of additional endogenous risk factors of deep-vein thrombosis (DVT). Setting: Regional Spinal Unit of Florence, Italy. Methods: A total of 43 patients with spinal lesion and a history of DVT during the acute stage of their neurological impairment (Group A) were comprehensively evaluated and the blood concentrations of the following risk factors, that are presumably associated with DVT, were determined: antithrombin III (ATIII), protein C (PC), protein S (PS), factor V Leiden, gene 200210A polymorphism, homocysteine (Hcy), inhibitor of plasminogen activator-1 (PAI-1) and lipoprotein A (LpA). The control group (Group B) consisted of 46 patients matched to Group A for sex, age, neurological status and prophylactic treatment during the acute stage, with no history of DVT. Statistical analysis was performed using the Mann–Whitney and Fisher’s exact tests. Results: Of the individuals in GroupA, 14% had no risk factor and 86% had at least one; however, in GroupB 54% had no endogenous risk factors and 46% had at least one. None of the individuals in either grouphad a deficit in their coagulation inhibitors (ATIII, PC and PS), and the LpA level was equivalent in the two groups. -

Assessing Plasmin Generation in Health and Disease
International Journal of Molecular Sciences Review Assessing Plasmin Generation in Health and Disease Adam Miszta 1,* , Dana Huskens 1, Demy Donkervoort 1, Molly J. M. Roberts 1, Alisa S. Wolberg 2 and Bas de Laat 1 1 Synapse Research Institute, 6217 KD Maastricht, The Netherlands; [email protected] (D.H.); [email protected] (D.D.); [email protected] (M.J.M.R.); [email protected] (B.d.L.) 2 Department of Pathology and Laboratory Medicine and UNC Blood Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +31-(0)-433030693 Abstract: Fibrinolysis is an important process in hemostasis responsible for dissolving the clot during wound healing. Plasmin is a central enzyme in this process via its capacity to cleave fibrin. The ki- netics of plasmin generation (PG) and inhibition during fibrinolysis have been poorly understood until the recent development of assays to quantify these metrics. The assessment of plasmin kinetics allows for the identification of fibrinolytic dysfunction and better understanding of the relationships between abnormal fibrin dissolution and disease pathogenesis. Additionally, direct measurement of the inhibition of PG by antifibrinolytic medications, such as tranexamic acid, can be a useful tool to assess the risks and effectiveness of antifibrinolytic therapy in hemorrhagic diseases. This review provides an overview of available PG assays to directly measure the kinetics of plasmin formation and inhibition in human and mouse plasmas and focuses on their applications in defining the role of plasmin in diseases, including angioedema, hemophilia, rare bleeding disorders, COVID- 19, or diet-induced obesity. -

Therapeutic Fibrinolysis How Efficacy and Safety Can Be Improved
JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY VOL.68,NO.19,2016 ª 2016 PUBLISHED BY ELSEVIER ON BEHALF OF THE ISSN 0735-1097/$36.00 AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION http://dx.doi.org/10.1016/j.jacc.2016.07.780 THE PRESENT AND FUTURE REVIEW TOPIC OF THE WEEK Therapeutic Fibrinolysis How Efficacy and Safety Can Be Improved Victor Gurewich, MD ABSTRACT Therapeutic fibrinolysis has been dominated by the experience with tissue-type plasminogen activator (t-PA), which proved little better than streptokinase in acute myocardial infarction. In contrast, endogenous fibrinolysis, using one-thousandth of the t-PA concentration, is regularly lysing fibrin and induced Thrombolysis In Myocardial Infarction flow grade 3 patency in 15% of patients with acute myocardial infarction. This efficacy is due to the effects of t-PA and urokinase plasminogen activator (uPA). They are complementary in fibrinolysis so that in combination, their effect is synergistic. Lysis of intact fibrin is initiated by t-PA, and uPA activates the remaining plasminogens. Knockout of the uPA gene, but not the t-PA gene, inhibited fibrinolysis. In the clinic, a minibolus of t-PA followed by an infusion of uPA was administered to 101 patients with acute myocardial infarction; superior infarct artery patency, no reocclusions, and 1% mortality resulted. Endogenous fibrinolysis may provide a paradigm that is relevant for therapeutic fibrinolysis. (J Am Coll Cardiol 2016;68:2099–106) © 2016 Published by Elsevier on behalf of the American College of Cardiology Foundation. n occlusive intravascular thrombus triggers fibrinolysis, as shown by it frequently not being A the cardiovascular diseases that are the lead- identified specifically in publications on clinical ing causes of death and disability worldwide.