Eye Health Needs Assessment 2014
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chester Road, Stonnall Guide Price £269,950
178 Chester Road, Stonnall Guide Price £269,950 A spacious, well presented, extended, traditional style semi detached family residence situated in this popular semi rural location yet remaining within easy reach of local amenities. * Open Aspect to Front * Nature Reserve to Rear * Recessed Porch * Reception Hall * Guest Cloakroom * Through Lounge/Dining Room * Extended Fitted Kitchen * Three Bedrooms * Bathroom * Garage & Extensive Off Road Parking * Attractive Gardens * Gas Central Heating System * PVCu Double Glazing * Post code: WS9 9DF Directions: A-Z Page 22. Ref 2D. 178 Chester Road, Stonnall Reception Hall Through Lounge/Dining Room Through Lounge/Dining Room 178 Chester Road, Stonnall Extended Fitted Kitchen Bedroom One Bedroom Two 178 Chester Road, Stonnall Bedroom Three Bathroom Attractive Rear Garden Attractive Rear Garden 178 Chester Road, Stonnall Attractive Rear Garden Deep Fore Garden Deep Fore Garden 178 Chester Road, Stonnall An internal inspection is highly recommended to begin to fully appreciate this spacious, well presented and extended traditional style semi detached family residence enjoying an excellent semi rural position in this popular residential location with open aspect to the front and nature reserve to the rear yet remaining within easy reach of local amenities. The area is extremely accessible to all main centres of the West Midlands conurbation with the A5 Trunk and M6 Toll Roads within 4 miles at Brownhills and Shenstone, leading to the M6, M5, M42 and M54. Main centre shopping is available at Lichfield and Walsall and children of all ages have a wide range of good schools provided including St Francis of Assisi Catholic Technology College at Aldridge, the highly regarded Queen Mary’s Grammar school for boys and High school for girls at Walsall and Friary High School and King Edwards in Lichfield. -

The List of Pharmacies Registered to Sell Ppcs on Our Behalf Is Sorted Alphabetically in Postcode Order
The list of pharmacies registered to sell PPCs on our behalf is sorted alphabetically in postcode order. 0 NAME PREMISES ADDRESS 1 PREMISES ADDRESS 2 PREMISES ADDRESS 3 PREMISES ADDRESS 4 LLOYDS PHARMACY SAINSBURYS, EVERARD CLOSE ST ALBANS HERTFORDSHIRE AL1 2QU BOOTS UK LIMITED 9 ST PETERS STREET ST.ALBANS HERTFORDSHIRE AL1 3DH FREEMAN GRIEVES LTD 111-113 ST PETERS STREET ST.ALBANS HERTFORDSHIRE AL1 3ET LLOYDS PHARMACY PARKBURY HOUSE ST PETER ST ALBANS HERTFORDSHIRE AL1 3HD IMED PHARMACY 67 HATFIELD ROAD ST ALBANS HERTFORDSHIRE AL1 4JE LLOYDS PHARMACY SAINSBURYS, BARNET ROAD LONDON COLNEY ST ALBANS HERTFORDSHIRE AL2 1AB LLOYDS PHARMACY 17 RUSSELL AVENUE ST ALBANS HERTFORDSHIRE AL3 5ES CROWN PHAMRACY 65 HIGH STREET REDBOURN ST ALBANS HERTFORDSHIRE AL3 7LW MANOR PHARMACY (WHEATHAMPSTEAD) LTD 2 HIGH STREET WHEATHAMPSTEAD HERTFORDSHIRE AL4 8AA BOOTS UK LIMITED 23-25 HIGH STREET HARPENDEN HERTFORDSHIRE AL5 2RU LLOYDS PHARMACY 40 HIGH STREET WELWYN GARDEN CITY HERTFORDSHIRE AL6 9EQ LLOYDS PHARMACY 84 HALDENS WELWYN GARDEN CITY HERTFORDSHIRE AL7 1DD BOOTS UK LIMITED 65 MOORS WALK WELWYN GARDEN CITY HERTFORDSHIRE AL7 2BQ BOOTS UK LIMITED 31 COLE GREEN LANE WELWYN GARDEN CITY HERTFORDSHIRE AL7 3PP PEARTREE PHARMACY 110 PEARTREE LANE WELWYN GARDEN CITY HERTFORDSHIRE AL7 3UJ BOOTS UK LIMITED 126 PEARTREE LANE WELWYN GARDEN CITY HERTFORDSHIRE AL7 3XY BOOTS UK LIMITED 31 THE HOWARD CENTRE WELWYN GARDEN CITY HERTFORDSHIRE AL8 6HA LLOYDS PHARMACY SAINSBURYS, CHURCH ROAD WELWYN GARDEN CITY HERTFORDSHIRE AL8 6SA LLOYDS PHARMACY 9 SHOPLANDS WELWYN GARDEN -

Public Health Area Profiles December 2012
Walsall Area Partnership Public Health Profile: Aldridge/Pheasey/Streetly/Walsall Wood Public Health Area Profiles December 2012 VERSION 2 Darlaston/ Bentley Area 2: Aldridge/Pheasey/ Aldridge/Pheasey/Streetly/WalsallStreetly/Walsall Wood Wood Page of 34 Walsall Area Partnership Public Health Profile: Aldridge/Pheasey/Streetly/Walsall Wood Executive Summary The Area Partnership has 5 communities within it’s bound- ary (Approx 48,000 population): Aldridge (12,700) Aldridge North (4,100) Pheasey (8,800) Streetly (13,500) & Walsall Wood (8,900) The population is on the whole older than the Walsall av- erage, with much higher %’s of both men and women aged 65 and over The area has a relatively small number of residents from BME communities—around 3-4% Compared to the majority of Walsall, residents in the Area Partnership are relatively well-off economically. Most live in small areas in the least deprived half of the country. Geographically, the area partnership shares borders with South Staffordshire and Birmingham East and North PCT’s. Residents are likely to access some primary and secondary care health services outside of Walsall Health Priorities: Generally, health outcomes are better in communities in this Area Partnership than Walsall averages. Indicators of child health are good in the area with relatively low Infant Mortality rates and lower levels of childhood obesity. Sex- ual health is also generally good in the area (low teenage pregnancies and Chlamydia infection levels). Life expectan- cy, as defined by current average age at death is a number of years higher than the rest of Walsall for both men and women. -

Staffordshire. Stowe by Ch.Artley
DIRECTORY.) STAFFORDSHIRE. STOWE BY CH.ARTLEY. 34:7 division of Lichfield and Brownbills, Lichfield union and dispatched at 6.20 p.m. (week days only). Postal orders county court district, rural deanery of Lichfield, arch are issued here, but not paid. The nearest money order deaconry of Stafford and diocese of Lichfield. The district & telegraph office is at Walsall Wood church of St. Peter, standing on an eminence between WALL LETTER Box, Lynn, cleared at 6 p.m Upper and Lower Stonnall, was erected in 1822 at a cost of National School (mixed), Stonnall, built with master's £1,100, and is a building of local red stone, consisting of house, in 1874, at a cost of £ x,40], raised by subscription ; chancel (added in 1843), nave and a small western tower the school will accommodate about 200 children; average containing one bell: the chancel was built at the sole expenRe attendance, 120 ; .Albert Edward Bussell, master; Mrs. of William Leigh esq. late of Little Aston Hall, who also Bussell, mistress gave the interior fittings, originally intended for a church at Adelaide, Australia: the east window is stained and there Little As ton is 21 miles south. Little Aston Hall is a are several others: the church was restored in 1895 at a fine mansion, much enlarged by the present proprietor, the cost of about £sso, and affords 400 sittings. The earliest Hon. Edward Swynfen Parker-Jervis. This place was date in the register is March 1 l, 1823. The living is a formed into an ecclesiastical pa.r;sh Oct. -

Wolverhampton City Council OPEN EXECUTIVE DECISION ITEM (AMBER)
Agenda Item: 5 Wolverhampton City Council OPEN EXECUTIVE DECISION ITEM (AMBER) SPECIAL ADVISORY GROUP Date: 28 October 2011 Portfolio(s) ALL Originating Service Group(s) DELIVERY Contact Officer(s)/ SUSAN KEMBREY KEY DECISION: YES Telephone Number(s) 4300 IN FORWARD PLAN: YES Title BOUNDARY COMMISSION REVIEW OF PARLIAMENTARY CONSTITUENCIES – WEST MIDLANDS REGION CONSULTATION ON INITIAL PROPOSALS Recommendation (a) That the initial proposals of the Boundary Commission for England for the review of Parliamentary Constituencies in the West Midland region England as detailed in Sections 2 and 3 of the report be noted (b) That the Special Advisory Group recommend Cabinet to invite the three political groups to formulate their individual views on the proposals set out in the consultation paper for submission to the Boundary Commission direct. 1 1.0 PURPOSE 1.1 To advise of the consultation exercise on the initial proposals of the Boundary Commission for the review of Parliamentary Constituencies in the West Midland region and the date to respond to the consultation. 2.0 BACKGROUND 2.1 The Boundary Commission for England (BCE) is an independent and impartial non- departmental public body which is responsible for reviewing Parliamentary constituency boundaries in England. The BCE conduct a review of all the constituencies in England every five years. Their role is to make recommendations to Parliament for new constituency boundaries. The BCE is currently conducting a review of all Parliamentary constituency boundaries in England based on new rules laid down by Parliament. These rules involve a reduction in the number of constituencies in England (from 533 to 502) and stipulate that every constituency, apart from two specific exemptions, must have an electorate no smaller than 72,810 and no larger than 80,473. -
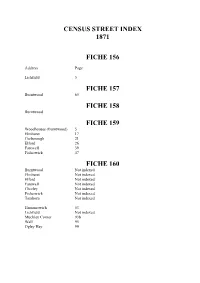
Census Street Index 1871
CENSUS STREET INDEX 1871 FICHE 156 Address Page Lichfield 5 FICHE 157 Burntwood 65 FICHE 158 Burntwood FICHE 159 Woodhouses (Burntwood) 5 Elmhurst 17 Curborough 21 Elford 26 Farewell 39 Fisherwick 47 FICHE 160 Burntwood Not indexed Elmhurst Not indexed Elford Not indexed Farewell Not indexed Chorley Not indexed Fisherwick Not indexed Tamhorn Not indexed Hammerwich 53 Lichfield Not indexed Muckley Corner 93b Wall 95 Ogley Hay 99 FICHE 160 OGLEY HAY Address Page Address Page Ogley Hay 88-127 New Road 104 Bells Row 99 Brick Hill Farm, Chester Rd 104 Church Hill 99 Chester Road 104-117 Shoulder of Mutton Inn 99 Wheatsheaf 113 Hope Cottage 100 Miners Arms 114 School House 103 The Square 117 Vicarage 103 Burntwood Road 121 Wolverhampton Road 122-127 FICHE 162 Address Page Ogley Hay 4-17 Address Page Walsall Road 4 Spring Hill 11 Watling Street Road 4 Walsall Road 11 Ogley Road 4-6 Barrack Lane 11 Fox Row 6 Warren House Farm 12A Walsall Road 7-9 Lock House 12 Hilton Lane 9 Weeford 16 Rowleys Cottage 10 Thickbroom 22 Rowleys Farm 10 Packington 23 Cranbrook Farm 10 Swinfen 25 Walsall Road 10 Shenstone 30-49,59-68 Spring Hill Farm 11 FICHE 163 Address Page Address Page Wood End 50 Friezeland Lane 65 Footheley 53-59 The Anchor Inn, Chester Rd. 68 Cranebrook 59 Catshill 68 Pouk Lane 59 Chester Road 68 Whiteacres Lane 59 Shire Oak Cottages 68 Cartersfield Lane 59 The Royal Oak 68 Sandhills 60 Hodgkins Row 71 Shire Oak 62 Robinson’s Row 72 Gilpin’s Houses 62 Clark’s Row 73 Friezeland 64 Ogley Lane 73 Williams Row 73 FICHE 164 OGLEY HAY (cont) Address -

Retail Unit to Let
RETAIL UNIT TO LET Unit 5 - 6 Neighbourhood Shopping Centre, sw.co.uk Slaters Road, Walsall Wood, West Midlands. WS9 9JD Location Walsall Wood is a largely residential suburb on the northern edge of the West Midlands conurbation between Aldridge and Brownhills. Neighbourhood Shopping Centre is a local shopping centre, made up of several retail units with flats above is prominently sited at the busy Streets Corner junction where the A461 Walsall to Lichfield Road crosses the B1452 Slaters’ Road. Opposite is the Oak Park Leisure Centre, KFC, a doctors’ surgery, a pharmacy and a recently developed Co-op Local store. To the rear is Better Gym. The property can be found by using the postcode WS9 9JD Description Unit 5 - 6 consists of two rectangular retail units, which have been joined to create a larger unit, with storage, offices and staff facilities on the first floor above. The unit benefits from rear access for loading by a shared service corridor. Internally the unit extends to the following approximate Net Internal Areas: SQ M SQ FT Retail 644.24 6,935 • Double retail unit, with first floor First floor 157.35 1,694 storage/ office. Total 901.59 8,628 • Rear access for loading. • Local neighbourhood parade. Consideration will be given to letting the unit in two parts, each with ground floor retail space and first floor rooms. • Flexible lease terms available. A split of the unit, would create two retail areas of approximately 3,255 sq ft and 3,680 sq ft. • Rental of £60,000 per annum. Rent £60,000 per annum, exclusive VAT The property is elected for VAT, which is charged at the prevailing rate. -

5454 the LONDON GAZETTE, 21 JULY, 1922. Streets in Which, It Is Proposed That Electrio Lines Walsall Wood.—(High Street, Queen
5454 THE LONDON GAZETTE, 21 JULY, 1922. streets in which, it is proposed that electrio lines Walsall Wood.—(High Street, Queen. shall be laid down within a period tci bei speci- Street, Boatman's Lane, dayhanger Road, fied by the Older are as follows/: — Camden Street, Pier Street. This following, streets in, whole or part: — High Street, Btrownhills. Chasetoum.—High Street, Queen Street, (B) Railways— Hill Street, Union Street, New Street, High- (1) The followingi level crossings over the fields, Triangle. London and North Western Railway: — Chase Terrace.—Cannook Road, Rugeley -Alt, Highbridge, Norton: Canes. Rioad, Princessi Street, Iromstonei Road, High (2) Over the Cannock. Chase and Wolver- .Street. hampton Railway:—> Boney Hay.—Spinney Lane, Oak L'ane. At Canno'ok Road, High Street, and Rail- Norton Canes.—Hednesford Road, Can- way Lane (Cha'se Terrace), Burntwood, and nods Road, Norton East Road, Burntwood Anglesey, Sidings and Anglesey Wharf, Road. Hammeirwioh. BroumhiUs.—'High Street, Lichfield Road, Ogley Hay Lane, Coppice Lane, Church (3) The following level crossings over the- Street, Pelsall Road, Vicarage Road, Midland Railway: — Brickiln Street. At Norton East Road, Norton Canes. 3. The streets and parts of streets not repair- 4. Td authorise the: Undertakers to exercise able by the local .authority .(including roadways within the area of supply all powers usually over bridges and the approaches thereto) and conferred upon distributors of electrical' railways (including level crossings) which the energy. Undertakers propose to take powers to break 5. To authorise* the Undertakers to take, up are:—' collect and recover rates, rente and charges for (A) Streets— the supply of electricity and the sale and use- Chase Terrace.—'Water Street, 'Chapel of any machine, lamps, meters, fittings or Street, Thorpe Street, School .Lane, Holly apparatus connected therewith, and to pre- Grove1 Lane, Hill Lane. -

'10 Lichfield to Wednesbury' (Pdf, 512KB)
L CHF ELD STAFFORDSH RE West Midlands Key Route Network WALSALL LichfieldWOLVERHAMPTON to Wednesbury WEST BROMW CH DUDLEY BRMNGHAM WARW CKSH RE WORCESTERSH RE SOL HULL COVENTRY Figure 1 12 A5 A38, A38(M), A47, A435, A441, A4400, A4540, A5127, B4138, M6 L CHF ELD Birmingham West Midlands Cross City B4144, B4145, B4148, B4154 11a Birmingham Outer Circle A4030, A4040, B4145, B4146 Key Route Network A5 11 Birmingham to Stafford A34 Black Country Route A454(W), A463, A4444 3 2 1 M6 Toll BROWNH LLS Black Country to Birmingham A41 M54 A5 10a Coventry to Birmingham A45, A4114(N), B4106 A4124 A452 East of Coventry A428, A4082, A4600, B4082 STAFFORDSH RE East of Walsall A454(E), B4151, B4152 OXLEY A449 M6 A461 Kingswinford to Halesowen A459, A4101 A38 WEDNESF ELD A34 Lichfield to Wednesbury A461, A4148 A41 A460 North and South Coventry A429, A444, A4053, A4114(S), B4098, B4110, B4113 A4124 A462 A454 Northfield to Wolverhampton A4123, B4121 10 WALSALL A454 A454 Pensnett to Oldbury A461, A4034, A4100, B4179 WOLVERHAMPTON Sedgley to Birmingham A457, A4030, A4033, A4034, A4092, A4182, A4252, B4125, B4135 SUTTON T3 Solihull to Birmingham A34(S), A41, A4167, B4145 A4038 A4148 COLDF ELD PENN B LSTON 9 A449 Stourbridge to Wednesbury A461, A4036, A4037, A4098 A4123 M6 Stourbridge to A449, A460, A491 A463 8 7 WEDNESBURY M6 Toll North of Wolverhampton A4041 A452 A5127 UK Central to Brownhills A452 WEST M42 A4031 9 A4037 BROMW CH K NGSTAND NG West Bromwich Route A4031, A4041 A34 GREAT BARR M6 SEDGLEY West of Birmingham A456, A458, B4124 A459 M5 A38 A461 -

Walsall Local History Centre Aldridge Historytrail
• istor ra1 1-1 --- ~ • ~· :. ), - ;\~ ~ ,< Walsall Local History Centre Aldridge HistoryTrail by Betty Fox William Yates' map of the County of Stafford 1769 Reproduced by kind p ermission of Stafford sh ire County Record Office The author is grateful to Mervyn Rowley for permission to use his drawing of The Moot- House on the front cover. · (c) Copyright Walsall Local History Centre l 990 ISBN 0946652 20 I ,Walsall PubI ished by Walsall Metropolitan Borough Council '~ Walsall Leisure Services, Library and lnforma t ion Services THE EARLY HISTORY OF ALDRIDGE The earliest sign of habitation in the area is indicated by t he Mesolithic or middle stone age flints which have been found at Bourne Pool in association with ancient earthworks. At Castlefort there is a small hill-fort, believed to be iron age, and a bronze age hoard was found in 1824 at Greensborough Farm just over the parish boundary in Shenstone. This consisted of swords, spearheads, celts or battle axes, axes, palstaves and ot her objects dating from approximately 900 BC. Fragments of Roman glass and tiles have been found at Castlefort but no other direct evidence of Roman occupation has come to light i n spite of the proximity of Ryknield Street which runs through Sut t on Park and continues northward quite close to the parish boundary. The name given to Aldridge in the Domesday Book - Alrewic - is Anglo-Saxon and it is probable that the community was established during this period. Neighbour ing Little Aston and Barr were the subjects of a grant of land by a charter dated 957. -

54 Cartersfield Lane, Stonnall £950 PCM
54 Cartersfield Lane, Stonnall £950 PCM A superbly appointed and recently refurbished three bedroom Detached Cottage occupying a superb Rural position enjoying stunning open views. * Reception Hall * Guest Cloak Room * Lounge/Dining Room * Luxury Fitted Breakfast Kitchen * Three Bedrooms * Luxury Bathroom * Off Road Parking * Rear Garden * Solar Panels * Electric Central Heating System * PVCu Double Glazing * 6/12 Months Tenancy * NO DSS * NO PETS * NO SMOKERS * NO SHARERS * Post code: WS9 9EQ Directions: A-Z Page 23 Ref: 1F 54 Cartersfield Lane, Stonnall Lounge/Dining Room Lounge/Dining Room Luxury Fitted Breakfast Kitchen 54 Cartersfield Lane, Stonnall Bedroom One Bedroom Two Bedroom Three 54 Cartersfield Lane, Stonnall Bathroom Rear Garden Open Views 54 Cartersfield Lane, Stonnall A superbly appointed three bedroom Detached Cottage that has recently been refurbished to a high standard and occupies a superb Rural position enjoying stunning open views. The area is extremely accessible to all main centres of the West Midlands conurbation with the A5 Trunk and M6 Toll Roads within 4 miles at Brownhills and Shenstone, leading to the M6, M5, M42 and M54. Main centre shopping is available at Lichfield and Walsall and children of all ages have a wide range of good schools provided including St Francis of Assisi Catholic Technology College at Aldridge, the highly regarded Queen Mary’s Grammar school for boys and High school for girls at Walsall and Friary High School and King Edwards in Lichfield. The area is well served for leisure facilities with Oak Park Leisure Centre in Walsall Wood and cricket, hockey and squash clubs behind the church at The Green, Aldridge and Druids Heath Golf Club off Stonnall Road while Stonnall village enjoys a range of community activities. -

1964 the Former Walsall Wood Colliery Is Abandoned. 1966 Effluent Disposal Limited, a Subsidiary of Leigh Interests Limited
1964 The former Walsall Wood colliery is abandoned. 1966 Effluent Disposal Limited, a subsidiary of Leigh Interests Limited open facility for the subterranean disposal of liquid wastes and sludges, under licence from The National Coal board. This facility saw the reception of liquid wastes including inorganic acids, organic acids, heavy metal containing solutions, phenolic liquids, oily wastes, dairy wastes, scrubber liquors, lagoon liquors, treated cyanide wastes and many others. At its peak it was receiving around 35,000,000 gallons of liquid waste per annum. A 1971 Birmingham post article claimed that the company admitted to pumping 77.25 million gallons of liquids and sludge into such sites, with about 80% of it into the 12+ miles of void in the Walsall Wood colliery. 1972 The Deposit of Poisonous Wastes Act imposes some stricter conditions on waste operators and producers after a nationwide cyanide dumping scare- particularly focusing on The West Midlands. 1974 The Control of Pollution Act requires sites to be licensed with conditions. This regulation in The West Midlands is overseen by The West Midlands County Council who would consider licences on a case by case basis. 1976 Early in the year, access to the Walsall Wood shaft becomes blocked by falling brickwork from a deteriorating shaft at Lindon Road Brownhills. Another site- The Mitco lagoon tip off Coppice Lane, Aldridge was used instead to supposedly “treat” the waste. The Birmingham Daily Post article of June 6th 1976 sets the scene. Effluent Disposal seek planning permission to drill exploratory borehole into the workings known as “the mitco borehole”.