DJO Oculodigital Phenomenon Leading to Advanced Keratoconus in Retinopathy of Prematurity – a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Congenital Cataract
3801 W. 15th St., Bldg. A, Ste. 110 Plano, TX 75075 Phone: (972) 758-0625 Fax: (972) 964-5725 Email: [email protected] Website: www.drstagerjr.com Congenital Cataract Your eye works a lot like a camera. Light rays focus through the lens on the retina, a layer of light-sensitive cells at the back of the eye. Similar to photographic film, the retina allows the image to be “seen” by the brain. Over time, the lens of our eye can become cloudy, preventing light rays from passing clearly through the lens. The loss of transparency may be so mild that vision is barely affected, or it can be so severe that no shapes or movements are seen—only light and dark. When the lens becomes cloudy enough to obstruct vision to any significant degree, it is called a cataract. Eyeglasses or contact lenses can usually correct slight refractive errors caused by early cataracts, but they cannot sharpen your vision if a severe cataract is present. The most common cause of cataract is aging. Occasionally, babies are born with cataracts or develop them very early in life. This condition is called congenital cataract. There are many causes of congenital cataract. Certain diseases can cause the condition, and sometimes it can be inherited. However, in most cases, there is no identifiable cause. Treatment for cataract in infants varies depending on the nature of each patient’s condition. Surgery is usually recommended very early in life, but many factors affect this decision, including the infant’s health and whether there is a cataract in one or both eyes. -

Multipurpose Conical Orbital Implant in Evisceration
Ophthalmic Plastic and Reconstructive Surgery Vol. 21, No. 5, pp 376–378 ©2005 The American Society of Ophthalmic Plastic and Reconstructive Surgery, Inc. Multipurpose Conical Orbital Implant in Evisceration Harry Marshak, M.D., and Steven C. Dresner, M.D. Doheny Eye Institute, Keck School of Medicine, University of Southern California, Los Angeles, California, U.S.A. Purpose: To evaluate the safety and efficacy of the porous polyethylene multipurpose conical orbital implant for use in evisceration. Methods: A retrospective review of 31 eyes that underwent evisceration and received the multipurpose conical orbital implant. The orbits were evaluated at 1 week, 1 month, and 6 months after final prosthetic fitting for implant exposure, superior sulcus deformity, and prosthetic motility. Results: There were no cases of extrusion, migration, or infection. All patients had a good cosmetic result after final prosthetic fitting. Prosthetic motility was good in all patients. Exposure developed in one eye (3%) and a superior sulcus deformity developed in one eye (3%). Conclusions: Placement of an multipurpose conical orbital implant in conjunction with evisceration is a safe and effective treatment for blind painful eye that achieves good motility and a good cosmetic result. visceration has proved to be effective for the treat- forms anteriorly to the sclera to be closed over it, without Ement of blind painful eye from phthisis bulbi or crowding the fornices, and extends posteriorly through endophthalmitis. By retaining the sclera in its anatomic the posterior sclerotomies, providing needed volume to natural position, evisceration has the advantage of allow- the posterior orbit. ing the insertions of the extraocular muscles to remain intact, promoting better motility. -

Vision Screening Training
Vision Screening Training Child Health and Disability Prevention (CHDP) Program State of California CMS/CHDP Department of Health Care Services Revised 7/8/2013 Acknowledgements Vision Screening Training Workgroup – comprising Health Educators, Public Health Nurses, and CHDP Medical Consultants Dr. Selim Koseoglu, Pediatric Ophthalmologist Local CHDP Staff 2 Objectives By the end of the training, participants will be able to: Understand the basic anatomy of the eye and the pathway of vision Understand the importance of vision screening Recognize common vision disorders in children Identify the steps of vision screening Describe and implement the CHDP guidelines for referral and follow-up Properly document on the PM 160 vision screening results, referrals and follow-up 3 IMPORTANCE OF VISION SCREENING 4 Why Screen for Vision? Early diagnosis of: ◦ Refractive Errors (Nearsightedness, Farsightedness) ◦ Amblyopia (“lazy eye”) ◦ Strabismus (“crossed eyes”) Early intervention is the key to successful treatment 5 Why Screen for Vision? Vision problems often go undetected because: Young children may not realize they cannot see properly Many eye problems do not cause pain, therefore a child may not complain of discomfort Many eye problems may not be obvious, especially among young children The screening procedure may have been improperly performed 6 Screening vs. Diagnosis Screening Diagnosis 1. Identifies children at 1. Identifies the child’s risk for certain eye eye condition conditions or in need 2. Allows the eye of a professional -

Treatment of Congenital Ptosis
13 Review Article Page 1 of 13 Treatment of congenital ptosis Vladimir Kratky1,2^ 1Department of Ophthalmology, Queen’s University, Kingston, Canada; 21st Medical Faculty, Charles University, Prague, Czech Republic Correspondence to: Vladimir Kratky, BSc, MD, FRCSC, DABO. Associate Professor of Ophthalmology, Director of Ophthalmic Plastic and Orbital Surgery, Oculoplastics Fellowship Director, Queen’s University, Kingston, Canada; 1st Medical Faculty, Charles University, Prague, Czech Republic. Email: [email protected]. Abstract: Congenital ptosis is an abnormally low position of the upper eyelid, with respect to the visual axis in the primary gaze. It can be present at birth or manifest itself during the first year of life and can be bilateral or unilateral. Additionally, it may be an isolated finding or part of a constellation of signs of a specific syndrome or systemic associations. Depending on how much it interferes with the visual axis, it may be considered as a functional or a cosmetic condition. In childhood, functional ptosis can lead to deprivation amblyopia and astigmatism and needs to be treated. However, even mild ptosis with normal vision can lead to psychosocial problems and correction is also advised, albeit on a less urgent basis. Although, patching and glasses can be prescribed to treat the amblyopia, the mainstay of management is surgical. There are several types of surgical procedure available depending on the severity and etiology of the droopy eyelid. The first part of this paper will review the different categories of congenital ptosis, including more common associated syndromes. The latter part will briefly cover the different surgical approaches, with emphasis on how to choose the correct condition. -
Iol Calculations for Patients with Keratoconus
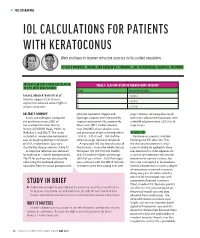
s THE LITERATURE IOL CALCULATIONS FOR PATIENTS WITH KERATOCONUS Work continues to improve refractive accuracy in this patient population. BY ALICE ROTHWELL, MBCHB, AND ANDREW M.J. TURNBULL, BM, PGCERTMEDED, PGDIPCRS, FRCOPHTH INTRAOCULAR LENS POWER CALCULATION TABLE 1. CLASSIFICATION OF KERATOCONUS SEVERITY IN EYES WITH KERATOCONUS Stage Keratometry Reading Savini G, Abbate R, Hoffer KJ, et al1 1 ≤ 48.00 D Industry support: K.J.H. licenses 2 > 48.00 D registered trademark name Hoffer to various companies 3 > 53.00 D ABSTRACT SUMMARY spherical equivalent. Myopic and stage 1 disease. Accuracy decreased Savini and colleagues compared hyperopic surprises were indicated by with more advanced keratoconus, with the prediction errors (PEs) of negative and positive PEs, respectively. a MedAE of greater than 2.50 D in all five standard formulas: Barrett Mean error (ME), median absolute stage 3 eyes. Universal II (BUII), Haigis, Hoffer Q, error (MedAE), mean absolute error, Holladay 1, and SRK/T. The study and percentage of eyes achieving within DISCUSSION included 41 consecutive keratoconic ±0.50 D, ±0.75 D, and ±1.00 D of the Keratoconus presents multiple eyes undergoing phacoemulsification refractive target were also calculated. challenges to IOL selection. First, and IOL implantation. Eyes were A hyperopic ME was found across all the standard keratometric index classified by disease severity (Table 1). five formulas. Across the whole dataset, cannot reliably be applied to these A subjective refraction was obtained the lowest ME (0.91 D) and MedAE eyes because this index depends on for each eye at 1 month postoperatively. (0.62 D) and the highest percentage a normal ratio between the anterior The PE for each eye was calculated by (36%) of eyes within ±0.50 D of target and posterior corneal surfaces, but subtracting the predicted spherical were achieved with the SRK/T formula. -

Analysis of Human Corneal Igg by Isoelectric Focusing
Investigative Ophthalmology & Visual Science, Vol. 29, No. 10, October 1988 Copyright © Association for Research in Vision and Ophthalmology Analysis of Human Corneal IgG by Isoelectric Focusing J. Clifford Woldrep,* Robin L. Noe,f and R. Doyle Stulringf Parameters which regulate the localization and retention of IgG within the corneal stroma are complex and poorly understood. Although multiple factors are involved, electrostatic interactions between IgG and anionic corneal tissue components, ie, proteoglycans (PG) and glycosaminoglycans (GAG) may regulate the distribution of antibodies within the corneal stroma. Isoelectric focusing (IEF) and blotting analysis of IgG revealed a restricted pi profile for both central and peripheral regions of the normal cornea. Similar analysis of pathological corneas from keratoplasty specimens in Fuchs' dys- trophy and keratoconus reveal a variable IEF profile. In the majority of keratoplasty specimens from patients with corneal edema or graft rejection, there was generally little or no IgG detectable. These results suggest that in edematous corneas where there is altered PG/GAG in the stroma and modified fluid dynamics, there is a concomitant loss of IgG. These findings may have implications for immuno- logic surveillance and protection of the avascular cornea. Invest Ophthalmol Vis Sci 29:1538-1543, 1988 The humoral immune system plays an important the soluble plasma proteins through ionic interac- role in mediating immunologic surveillance and pro- tions. The PGs and GAGs have long been known to -
Management Modalities for Keratoconus an Overview of Noninterventional and Interventional Treatments
REFRACTIVE SURGERY FEATURE STORY EXCLUSIVE ONLINE CONTENT AVAILABLE Management Modalities for Keratoconus An overview of noninterventional and interventional treatments. BY MAZEN M. SINJAB, MD, PHD anagement of keratoconus has advanced TAKE-HOME MESSAGE during the past few years, and surgeons can • When evaluating patients with keratoconus, ask now choose among numerous traditional and them to stop using RGP contact lenses at least 2 modern treatments. Traditional modalities weeks before evaluation to achieve correct Msuch as spectacle correction, contact lenses, penetrating measurement of the corneal shape. keratoplasty (PKP), and conductive keratoplasty (CK) • Interventional management modalities include CK, are still effective; however, demand for the last two has PKP, DALK, ICRSs, CXL, phakic IOLs, or some decreased with the advent of modern alternatives, specifi- combination of these treatments. cally intrastromal corneal ring segments (ICRSs) and cor- • Making the right management decision depends neal collagen crosslinking (CXL). Caution should be used on the patient’s corneal transparency and stress when considering these newer treatment modalities, and lines, age, progression, contact lens tolerance, surgeons should be aware of their indications, contraindi- refractive error, UCVA and BCVA, K-max, corneal cations, conditions, and complications before proceeding thickness, and sex. with treatment. Keratoconus treatments can be divided into two cate- Some patients achieve good vision correction and comfort gories, interventional and noninterventional. In this article, with this strategy. particular attention is given to ICRSs and CXL, as they are Advances in lens designs and materials have increased the the most popular emerging interventional management proportion of keratoconus patients who can be fitted with modalities for keratoconus. -

Updates on Myopia
Updates on Myopia A Clinical Perspective Marcus Ang Tien Y. Wong Editors Updates on Myopia Marcus Ang • Tien Y. Wong Editors Updates on Myopia A Clinical Perspective Editors Marcus Ang Tien Y. Wong Singapore National Eye Center Singapore National Eye Center Duke-NUS Medical School Duke-NUS Medical School National University of Singapore National University of Singapore Singapore Singapore This book is an open access publication. ISBN 978-981-13-8490-5 ISBN 978-981-13-8491-2 (eBook) https://doi.org/10.1007/978-981-13-8491-2 © The Editor(s) (if applicable) and The Author(s) 2020, corrected publication 2020 Open Access This book is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made. The images or other third party material in this book are included in the book's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the book's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specifc statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -

Prominent and Regressive Brain Developmental Disorders Associated with Nance-Horan Syndrome
brain sciences Article Prominent and Regressive Brain Developmental Disorders Associated with Nance-Horan Syndrome Celeste Casto 1,†, Valeria Dipasquale 1,†, Ida Ceravolo 2, Antonella Gambadauro 1, Emanuela Aliberto 3, Karol Galletta 4, Francesca Granata 4, Giorgia Ceravolo 1, Emanuela Falzia 5, Antonella Riva 6 , Gianluca Piccolo 6, Maria Concetta Cutrupi 1, Pasquale Striano 6,7 , Andrea Accogli 7,8, Federico Zara 7,8, Gabriella Di Rosa 9, Eloisa Gitto 10, Elisa Calì 11, Stephanie Efthymiou 11 , Vincenzo Salpietro 6,7,11,*, Henry Houlden 11 and Roberto Chimenz 12 1 Department of Human Pathology in Adult and Developmental Age “Gaetano Barresi”, Unit of Emergency Pediatric, University of Messina, Via Consolare Valeria 1, 98125 Messina, Italy; [email protected] (C.C.); [email protected] (V.D.); [email protected] (A.G.); [email protected] (G.C.); [email protected] (M.C.C.) 2 Unit of Ophthalmology, Department of Clinical and Experimental Medicine, University of Messina, Via Consolare Valeria 1, 98125 Messina, Italy; [email protected] 3 Casa di Cura la Madonnina, Via Quadronno 29, 20122 Milano, Italy; [email protected] 4 Department of Biomedical, Dental Science and Morphological and Functional Images, Neuroradiology Unit, University of Messina, Via Consolare Valeria 1, 98125 Messina, Italy; [email protected] (K.G.); [email protected] (F.G.) 5 Azienza Ospedaliera di Cosenza, Via San Martino, 87100 Cosenza, Italy; [email protected] 6 Pediatric Neurology and Muscular Diseases Unit, -

Expanding the Phenotypic Spectrum of PAX6 Mutations: from Congenital Cataracts to Nystagmus
G C A T T A C G G C A T genes Article Expanding the Phenotypic Spectrum of PAX6 Mutations: From Congenital Cataracts to Nystagmus Maria Nieves-Moreno 1,* , Susana Noval 1 , Jesus Peralta 1, María Palomares-Bralo 2 , Angela del Pozo 3 , Sixto Garcia-Miñaur 4, Fernando Santos-Simarro 4 and Elena Vallespin 5 1 Department of Ophthalmology, Hospital Universitario La Paz, 28046 Madrid, Spain; [email protected] (S.N.); [email protected] (J.P.) 2 Department of Molecular Developmental Disorders, Medical and Molecular Genetics Institue (INGEMM) IdiPaz, CIBERER, Hospital Universitario La Paz, 28046 Madrid, Spain; [email protected] 3 Department of Bioinformatics, Medical and Molecular Genetics Institue (INGEMM) IdiPaz, CIBERER, Hospital Universitario La Paz, 28046 Madrid, Spain; [email protected] 4 Department of Clinical Genetics, Medical and Molecular Genetics Institue (INGEMM) IdiPaz, CIBERER, Hospital Universitario La Paz, 28046 Madrid, Spain; [email protected] (S.G.-M.); [email protected] (F.S.-S.) 5 Department of Molecular Ophthalmology, Medical and Molecular Genetics Institue (INGEMM) IdiPaz, CIBERER, Hospital Universitario La Paz, 28046 Madrid, Spain; [email protected] * Correspondence: [email protected] Abstract: Background: Congenital aniridia is a complex ocular disorder, usually associated with severe visual impairment, generally caused by mutations on the PAX6 gene. The clinical phenotype of PAX6 mutations is highly variable, making the genotype–phenotype correlations difficult to establish. Methods: we describe the phenotype of eight patients from seven unrelated families Citation: Nieves-Moreno, M.; Noval, with confirmed mutations in PAX6, and very different clinical manifestations. -

Scleral Lenses and Eye Health
Scleral Lenses and Eye Health Anatomy and Function of the Human Eye How Scleral Lenses Interact with the Ocular Surface Just as the skin protects the human body, the ocular surface protects the human Scleral lenses are large-diameter lenses designed to vault the cornea and rest on the conjunctival tissue sitting on eye. The ocular surface is made up of the cornea, the conjunctiva, the tear film, top of the sclera. The space between the back surface of the lens and the cornea acts as a fluid reservoir. Scleral and the glands that produce tears, oils, and mucus in the tear film. lenses can range in size from 13mm to 19mm, although larger diameter lenses may be designed for patients with more severe eye conditions. Due to their size, scleral lenses consist SCLERA: The sclera is the white outer wall of the eye. It is SCLERAL LENS made of collagen fibers that are arranged for strength rather of at least two zones: than transmission of light. OPTIC ZONE The optic zone vaults over the cornea CORNEA: The cornea is the front center portion of the outer Cross section of FLUID RESERVOIR wall of the eye. It is made of collagen fibers that are arranged in the eye shows The haptic zone rests on the conjunctiva such a way so that the cornea is clear. The cornea bends light the cornea, overlying the sclera as it enters the eye so that the light is focused on the retina. conjunctiva, and sclera as CORNEA The cornea has a protective surface layer called the epithelium. -

Care of the Patient with Accommodative and Vergence Dysfunction
OPTOMETRIC CLINICAL PRACTICE GUIDELINE Care of the Patient with Accommodative and Vergence Dysfunction OPTOMETRY: THE PRIMARY EYE CARE PROFESSION Doctors of optometry are independent primary health care providers who examine, diagnose, treat, and manage diseases and disorders of the visual system, the eye, and associated structures as well as diagnose related systemic conditions. Optometrists provide more than two-thirds of the primary eye care services in the United States. They are more widely distributed geographically than other eye care providers and are readily accessible for the delivery of eye and vision care services. There are approximately 36,000 full-time-equivalent doctors of optometry currently in practice in the United States. Optometrists practice in more than 6,500 communities across the United States, serving as the sole primary eye care providers in more than 3,500 communities. The mission of the profession of optometry is to fulfill the vision and eye care needs of the public through clinical care, research, and education, all of which enhance the quality of life. OPTOMETRIC CLINICAL PRACTICE GUIDELINE CARE OF THE PATIENT WITH ACCOMMODATIVE AND VERGENCE DYSFUNCTION Reference Guide for Clinicians Prepared by the American Optometric Association Consensus Panel on Care of the Patient with Accommodative and Vergence Dysfunction: Jeffrey S. Cooper, M.S., O.D., Principal Author Carole R. Burns, O.D. Susan A. Cotter, O.D. Kent M. Daum, O.D., Ph.D. John R. Griffin, M.S., O.D. Mitchell M. Scheiman, O.D. Revised by: Jeffrey S. Cooper, M.S., O.D. December 2010 Reviewed by the AOA Clinical Guidelines Coordinating Committee: David A.