Differentiation of Restrictive Cardiomyopathy from Pericardial Constriction: Assessment of Diastolic Function by Radionuclide Angiography
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diagnosis and Treatment of Myocarditides
DIAGNOSIS AND TREATMENT OF MYOCARDITIDES Clinical guidelines Task force for preparing the text of recommendations Chairperson: Professor S.N. Tereshchenko (Moscow), Task force members: I.V. Zhirov (MD, Moscow), Professor V.P. Masenko (MD, Moscow), O.Yu. Narusov (Ph.D., Moscow), S.N. Nasonova (Ph.D., Moscow), Professor A.N. Samko (MD, Moscow), O.V. Stukalova (Ph.D., Moscow) and M.A. Shariya (MD, Moscow) Expert Committee: Professor Arutyunov G.P. (Moscow), Professor Moiseev S.V. (Moscow), Professor Vasyuk Yu.A. (Moscow), Professor Garganeeva A.A. (Tomsk), Professor Glezer M.G. (Moscow region), Professor Tkacheva O.N. (Moscow) Professor Shevchenko A.O. (Moscow), Professor Govorin A.V. (Chita), Professor Azizov V.A. (Azerbaijan), Professor Mirrahimov E.M. (Kyrgyzstan), Professor Abdullaev T.A. (Uzbekistan), Ph.D. Panfale E.M. (Moldova), MD Sudzhaeva O.A. (Belarus) Moscow, 2019 TABLE OF CONTENTS Page INTRODUCTION ............................................................................................................. 4 Evidence Base for Diagnosis and Treatment of Myocarditides…………….……6 I. MYOCARDITIDES CLASSIFICATION ................................................................... 5 1. Fulminant myocarditis. .................................................................................................... 6 2. Acute myocarditis. ........................................................................................................... 6 3. Chronic active myocarditis. ............................................................................................ -

Diagnostic Yield and Safety Profile of Endomyocardial Biopsy in the Non
REC Interv Cardiol. 2019;1(2):99-107 Original article Diagnostic yield and safety profile of endomyocardial biopsy in the non-transplant setting at a Spanish referral center Eusebio García-Izquierdo Jaén,a Juan Francisco Oteo Domínguez,a,* Marta Jiménez Blanco,a Cristina Aguilera Agudo,a Fernando Domínguez,a Jorge Toquero Ramos,a Javier Segovia Cubero,a Clara Salas Antón,b Arturo García-Touchard,a José Antonio Fernández-Díaz,a Rodrigo Estévez-Loureiro,a Francisco Javier Goicolea Ruigómez,a and Luis Alonso-Pulpóna a Servicio de Cardiología, Hospital Universitario Puerta de Hierro, Majadahonda, Madrid, Spain b Servicio de Anatomía Patológica, Hospital Universitario Puerta de Hierro, Majadahonda, Madrid, Spain ABSTRACT Introduction and objectives: Endomyocardial biopsy (EMB) is an established diagnostic tool in myocardial disease. However, this technique may carry major complications. We present the diagnostic and safety results of our experience in EMB in the non-trans- plant setting. We also present the results after the implementation of a technical and safety protocol developed at our center. Methods: We retrospectively analyzed the data of all EMBs conducted in non-transplant patients from September 2004 through July 2018. We compared the diagnostic yield and rate of major complications of EMB in two different periods: before and after implementing the protocol. Results: We included 204 EMBs performed in 190 patients. The most frequent indications were the evaluation of ventricular dys- function or suspected myocarditis (51.5%) and the evaluation of restrictive cardiomyopathy or suspected infiltrative disease (44.6%). One hundred and seventy-two EMBs were performed in the right cardiac chambers (84.3%) and 30 EMBs in the left cardiac chambers (14.7%). -

Intractable Chest Pain in Cardiomyopathy: Treatment by a Novel Technique of Cardiac Cryodenervation with Quantitative Immunohistochemical Assessment of Success
574 Br HeartJ 1993;69:574-577 TECHNIQUE Br Heart J: first published as 10.1136/hrt.70.6.574 on 1 December 1993. Downloaded from Intractable chest pain in cardiomyopathy: treatment by a novel technique of cardiac cryodenervation with quantitative immunohistochemical assessment of success J AR Gaer, L Gordon, J Wharton, J M Polak, K M Taylor, W McKenna, D J Parker Abstract she described episodes of chest pain, usually A novel method of cardiac denervation on exertion but also at rest and at night. The by cryoablation has been developed ex- pain occurred up to 10 times daily and her perimentally. The technique uses liquid exercise tolerance had deteriorated from four nitrogen delivered under pressure to miles to 200 yards. Although she denied ablate the principal sources of cardiac paroxysmal nocturnal dyspnoea, she slept innervation-namely, the adventitia sur- with three pillows. Her medication at this rounding the aorta, pulmonary arteries, time consisted of sotalol (80 mg twice daily) and veins. The technique has been veri- and verapamil (240 mg twice daily). She had fied experimentally both in vivo by four children (aged 6, 8, 10, and 11 years) all physiological means and in vitro by of whom were healthy. She was unaware of a quantitative immunohistochemistry and family history of hypertrophic cardiomyopa- the measurement of myocardial nor- thy, although two members of her family had adrenaline concentrations. A 35 year old died suddenly in middle age. On admission a woman presented with intractable pre- soft pansystolic murmur and considerable cordial pain, normal epicardial coronary obesity were noted. -
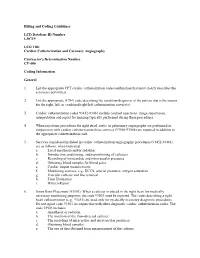
Billing and Coding Guidelines Cardiac Catheterization and Coronary Angiography CV-006
Billing and Coding Guidelines LCD Database ID Number L30719 LCD Title Cardiac Catheterization and Coronary Angiography Contractor's Determination Number CV-006 Coding Information General 1. List the appropriate CPT cardiac catheterization code/combination that most clearly describes the service(s) performed. 2. List the appropriate ICD-9 code describing the condition/diagnosis of the patient that is the reason for the right, left, or combined right/left catheterization service(s). 3. Cardiac catheterization codes 93452-93461 include contrast injections, image supervision, interpretation and report for imaging typically performed during these procedures. 4. When injections procedures for right atrial, aortic or pulmonary angiography are performed in conjunction with cardiac catheterization these services (93566-93568) are reported in addition to the appropriate catheterization code. 5. Services considered included in cardiac catheterization/angiography procedures (93452-93461) are as follows, when indicated: a. Local anesthesia and/or sedation b. Introduction, positioning, and repositioning of catheters c. Recording of intracardiac and intravascular pressures d. Obtaining blood samples for blood gases e. Cardiac output measurements f. Monitoring services, e.g., ECCS, arterial pressures, oxygen saturation g. Vascular catheter and line removal h. Final Evaluation i. Written Report 6. Swan Ganz Placement (93503). When a catheter is placed in the right heart for medically necessary monitoring purposes, the code 93503 must be reported. The codes describing a right heart catheterization (e.g., 93451) are used only for medically necessary diagnostic procedures. Do not report code 93503 in conjunction with other diagnostic cardiac catheterization codes. The code 93503 includes: a. Anesthesia or sedation. b. The insertion of the flow-directed catheter. -

Consensus Statement on Endomyocardial Biopsy
Cardiovascular Pathology 21 (2012) 245–274 Original Article 2011 Consensus statement on endomyocardial biopsy from the Association for European Cardiovascular Pathology and the Society for Cardiovascular Pathology ⁎ ⁎ Ornella Leone a, , John P. Veinot b, , Annalisa Angelini c, Ulrik T. Baandrup d, Cristina Basso c, Gerald Berry e, Patrick Bruneval f, Margaret Burke g, Jagdish Butany h, Fiorella Calabrese c, Giulia d'Amati i, William D. Edwards j, John T. Fallon k, Michael C. Fishbein l, Patrick J. Gallagher m, Marc K. Halushka n, Bruce McManus o, Angela Pucci p, E. René Rodriguez q, Jeffrey E. Saffitz r, Mary N. Sheppard g, Charles Steenbergen n, James R. Stone r, Carmela Tan q, Gaetano Thiene c, Allard C. van der Wal s, Gayle L. Winters r aBologna, Italy bOttawa, Ontario, Canada cPadua, Italy dHjoerring, Denmark eStanford, CA, USA fParis, France gLondon, UK hToronto, Ontario, Canada iRome, Italy jRochester, MN, USA kNew York, NY, USA lLos Angeles, CA, USA mSouthampton, UK nBaltimore, MD, USA oVancouver, BC, Canada pPisa, Italy qCleveland, OH, USA rBoston, MA, USA sAmsterdam, The Netherlands Received 3 August 2011; received in revised form 28 September 2011; accepted 7 October 2011 Abstract The Association for European Cardiovascular Pathology and the Society for Cardiovascular Pathology have produced this position paper concerning the current role of endomyocardial biopsy (EMB) for the diagnosis of cardiac diseases and its contribution to patient management, focusing on pathological issues, with these aims: • Determining appropriate EMB use in the context of current diagnostic strategies for cardiac diseases and providing recommendations for its rational utilization ⁎ Corresponding authors. O. Leone is to be contacted at U.O. -

Complications of Endomyocardial Biopsy in Heart Transplant Patients: a Retrospective Study of 2117 Consecutive Procedures
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Repositório Institucional dos Hospitais da Universidade de Coimbra Complications of Endomyocardial Biopsy in Heart Transplant Patients: A Retrospective Study of 2117 Consecutive Procedures F. Saraiva, V. Matos, L. Gonçalves, M. Antunes, and L.A. Providência ABSTRACT Background. Endomyocardial biopsy (EMB) remains the gold standard for the diagno- sis of graft rejection after heart transplantation (HT). Our purpose was to evaluate the rate of complications of this invasive procedure. Methods. This was a retrospective study of 175 patients, who were transplanted between November 2003 and October 2010 and survived more than 1 month after surgery. We evaluated the number of inconclusive EMB and described the incidence, nature, and subsequent management of several complications associated with this procedure. Results. Over a period of approximately 7 years, we performed 2217 EMB yielding 4972 specimens, namely, an average of 2.3 fragments per procedure. The majority of EMBs (95.3%) were performed by the femoral approach. Only 12 EMB (0.57%) were inconclu- sive. The overall complication rate was 0.71%. During puncture, one patient experienced a vasovagal reaction and another one, a femoral artery false aneurysm. During the biopsy, there was one case of cardiac perforation with tamponade, two cases of supraventricular tachycardia, and three atrioventricular conduction abnormalities. In 19 patients, histolog- ical analysis revealed chordal tissue, but only two patients developed mild tricuspid regurgitation. We observed five cases of coronary artery fistulae. The clinical outcomes were favorable in all cases. Conclusion. EMB proved to be a suitable, safe method to monitor rejection after HT. -

Outcomes of Mechanical Circulatory Support for Giant Cell Myocarditis: a Systematic Review
Journal of Clinical Medicine Article Outcomes of Mechanical Circulatory Support for Giant Cell Myocarditis: A Systematic Review Preeyal M. Patel 1, Abhiraj Saxena 1, Chelsey T. Wood 1, Thomas J. O’Malley 2 , Elizabeth J. Maynes 2, John W. C. Entwistle 2, H. Todd Massey 2, Preethi R. Pirlamarla 3, René J. Alvarez 3, Leslie T. Cooper 4 , J. Eduardo Rame 2 and Vakhtang Tchantchaleishvili 2,* 1 Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, PA 19107, USA; [email protected] (P.M.P.); [email protected] (A.S.); [email protected] (C.T.W.) 2 Division of Cardiac Surgery, Department of Surgery, Thomas Jefferson University, Philadelphia, PA 19107, USA; [email protected] (T.J.O.); [email protected] (E.J.M.); john.entwistle@jefferson.edu (J.W.C.E.); howard.massey@jefferson.edu (H.T.M.); eduardo.rame@jefferson.edu (J.E.R.) 3 Division of Cardiology, Department of Medicine, Thomas Jefferson University, Philadelphia, PA 19107, USA; preethi.pirlamarla@jefferson.edu (P.R.P.); rene.alvarez@jefferson.edu (R.J.A.) 4 Department of Cardiovascular Medicine, Mayo Clinic, Jacksonville, FL 32224, USA; [email protected] * Correspondence: vakhtang.tchantchaleishvili@jefferson.edu; Tel.: +1-215-955-6996; Fax: +1-215-955-6010 Received: 20 October 2020; Accepted: 23 November 2020; Published: 1 December 2020 Abstract: Treatment of giant cell myocarditis (GCM) can require bridging to orthotopic heart transplantation (OHT) or recovery with mechanical circulatory support (MCS). Since the roles of MCS and immunotherapy are not well-defined in GCM, we sought to analyze outcomes of patients with GCM who required MCS. -

Technique of Endomyocardial Biopsy-Including a Description of a New Form of Endomyocardial Bioptome P
Postgrad Med J: first published as 10.1136/pgmj.51.595.282 on 1 May 1975. Downloaded from Postgraduate Medical Journal (May 1975) 51, 282-285. Technique of endomyocardial biopsy-including a description of a new form of endomyocardial bioptome P. J. RICHARDSON M.R.C.P. Department of Cardiology, King's College Hospital, Denmark Hill, London SE5 9RS THE technique of endomyocardial biopsy which was the routine manner to the right atrium. The Konno developed by Konno and Sakakibara, 1963, and was catheter is rather rigid and, because of this, one has further reported by Sekiguchi and Konno, 1969; to produce a bend in the catheter before the instru- Konno, Sekiguchi and Sakakibara, 1971, and ment is introduced, otherwise difficulties may be Somers et al., 1971, has meant that it is now possible experienced in manipulating the catheter tip through to study the myocardium of patients suspected of the tricuspid valve. having intrinsic abnormality of the muscle structure We have found that manipulation in the right by histological, histochemical and electron micro- atrium on occasions may produce a series of atrial scopic examination. This is particularly applicable dysrhythmias, including atrial fibrillation, nodal to the cardiomyopathies, and it is in this context rhythm and supraventricular tachycardia, as the that the majority of biopsies which we have per- catheter impinges against the atrial wall. formed have been done (Table 1). The advantage of When it is thought that the catheter is positioned in a suitable place in the right ventricle to obtain a copyright. TABLE 1. Suspected clinical diagnoses myocardial sample, it is essential to check the site of the catheter tip. -

Canadian Consensus on Paediatric and Adult Congenital Heart Transplantation 2004
Canadian Consensus on Paediatric and Adult Congenital Heart Transplantation 2004 Primary Panel: Anne Dipchand (Chair), Renzo Cecere, Diego Delgado, Annie Dore, Nadia Giannetti, Haissam Haddad, Jonathan Howlett, Marie-Helene LeBlanc, Line Leduc, Ariane Marelli, Jean Perron, Nancy Poirier, Heather Ross Secondary Panel: Upton Allen, Myriam Brassard, James Y. Coe, Jean-Marc Cote, Derek Human, Luc Jutras, Miriam Kaufman, Sureya Shah, Christo Tchervenkov, Lori West Address for correspondence: Anne I. Dipchand, MD Clinical Head, Heart Transplant Program Hospital for Sick Children 555 University Avenue Toronto, Ontario, Canada M5G 1X8 Phone: 416-813-6674 Fax: 416-813-7547 [email protected] TABLE OF CONTENTS INTRODUCTION……………………………………………………………………………4 The Need for Paediatric and Adult Congenital Guidelines……………………………4 INDICATIONS AND CONTRAINDICATIONS…………………………………………..7 Indications – General Considerations………………………………………………….7 Contraindications – General Considerations…………………………………………..9 Functional Class………………………………………………………………………10 Cardiopulmonary Testing……………………………………………………………..12 Pulmonary Hypertension……………………………………………………………...13 Neonatal Advantage…………………………………………………………………..15 ABO-Incompatible (ABO-I) Transplantation………………………………………...16 Anatomically Normal Heart in the Paediatric Population…………………………….19 Congenital Heart Disease in the Paediatric Population……………………………….20 Univentricular circulation……………………………………………………..20 Other forms of CHD in the paediatric population…………………………….22 1 Adult Congenital Heart Disease………………………………………………………22 -

Acute Pacing-Induced Cardiomyopathy
Case Rep Int 2016;5:48–53. Alzahrani et al. 48 www.casereportsinternational.com CASE REPORT PEER REVIEWED | OPEN ACCESS Acute pacing-induced cardiomyopathy Talal Alzahrani, Sripooja Satya, Marco Mercader ABSTRACT with pacing-induced cardiomyopathy because other causes of cardiomyopathy were ruled Introduction: Pacing-induced cardiomyopathy out. Thus, his cardiac pacemaker device (PICM) is defined as a 10% reduction in the was upgraded to Biventricular pacing device left ventricular ejection fraction over several with implantable cardioverter defibrillator. months to a year after pacemaker implantation, Conclusion: This report describes a patient resulting in an ejection fraction of less than 50%. with a severe acute form of pacing-induced Nonetheless, other causes of cardiomyopathy cardiomyopathy and discusses the prevention should be excluded to diagnose patients with and therapy of this condition. this condition. Case Report: A 59-year-old male presented with a third-degree heart Keywords: Cardiomyopathy, Pacing, Pacemaker block and underwent pacemaker implantation with right ventricular pacing. Subsequently, How to cite this article he manifested with an acute heart failure exacerbation and a reduced ejection fraction Alzahrani T, Satya S, Mercader M. Acute pacing- within two months of pacemaker implantation. induced cardiomyopathy. Case Rep Int 2016;5:48–53. Consequently, he underwent further workup to exclude causes of dilated cardiomyopathy such as acute coronary syndrome, sarcoidosis, Article ID: 100031CRINTTA2016 hemochromatosis, granulomatosis with polyangiitis, and eosinophilic myocarditis. His left heart catheterization showed worsening ********* in his ejection fraction without any significant coronary stenosis. He had an endomyocardial doi:10.5348/crint-2016-31-CR-12 biopsy, which showed fibroblast proliferation and fibrosis with no evidence of any infiltrative cardiomyopathy. -

ASNC INFORMATION STATEMENT the Role and Clinical Effectiveness of Multimodality Imaging in the Management of Cardiac Complicatio
ASNC INFORMATION STATEMENT The role and clinical effectiveness of multimodality imaging in the management of cardiac complications of cancer and cancer therapy Raymond R. Russell, MD, PhD, FASNC,a Jonathan Alexander, MD,b Diwakar Jain, MD,c Indu G. Poornima, MD,d Ajay V. Srivastava, MD,e Eugene Storozynsky, MD, PhD,f and Ronald G. Schwartz, MD, MSf,g a Rhode Island Cardiovascular Institute, Rhode Island Hospital, The Warren Alpert Medical School of Brown University, Providence, RI b Cardiology Division, Western Connecticut Medical Center at Danbury Hospital, Danbury, CT c Section of Cardiovascular Medicine, New York Medical College and Westchester Medical Center, Valhalla, NY d Division of Cardiology, Allegheny Health Network, Pittsburgh, PA e Division of Cardiovascular Medicine, Scripps Clinic, La Jolla, CA f Cardiology Division, Department of Medicine, University of Rochester Medical Center, Rochester, NY g Nuclear Medicine Division, Department of Imaging Sciences, University of Rochester Medical Center, Rochester, NY Received Apr 13, 2016; accepted Apr 13, 2016 doi:10.1007/s12350-016-0538-8 With the increasing number of individuals living with a current or prior diagnosis of cancer, it is important for the cardiovascular specialist to recognize the various complications of cancer and its therapy on the cardiovascular system. This is true not only for established cancer therapies, such as anthracyclines, that have well established cardiovascular toxicities, but also for the new targeted therapies that can have ‘‘off target’’ effects in the heart and vessels. The purpose of this informational statement is to provide cardiologists, cardiac imaging specialists, cardio-oncologists, and oncologists an understanding of how multimodality imaging may be used in the diagnosis and management of the cardiovascular complications of cancer therapy. -

Cardiotoxicity of Epirubicin and Doxorubicin: Assessment by Endomyocardial Biopsy1
[CANCER RESEARCH 46, 3722-3727, July 1986] Cardiotoxicity of Epirubicin and Doxorubicin: Assessment by Endomyocardial Biopsy1 Frank M. Torti,2 Michael M. Bristow, Bert L. Lum, Stephen K. Carter, Anthony E. Howes, Diana A. Aston, Byron W. Brown, Jr., John F. Hannigan, Jr., Frederick J. Meyers, Edith P. Mitchell, and Margaret E. Billingham Northern California Oncology Group, Palo Alto, California [B. L. L., S. K. C., D. A. A., B. W. B., J. F. H.J; Divisions of Medical Oncology [F. M. T.], Radiation Therapy [A. E. H.I, Cardiology [M. M. B.], and Cardiac Pathology [M. E. B.¡,Stanford University Medical Center, Stanford, California 94305; V. A. Medical Center, Palo Alto, California 94304 [F. M. T., B. L. L.]; Department of Clinical Pharmacy, University of the Pacific, Stockton, California 9521J [B. L. L.]; Travis Air Force Base Medical Center, Travis, California 94535 [E. P. M.]; and the University of California, Davis Medical Center, Sacramento, California 95819 [F. J. M.] ABSTRACT at doses which produced equal antitumor effect (21). To assess the character and degree of epirubicin cardiotoxicity in humans, Forty-two évaluableendomyocardial biopsies were obtained from 29 patients treated with epirubicin, the 4'-epimer of doxorubicin in cumu a study at the Northern California Oncology Group used elec lative doses ranging from 147 mjj/nr to 888 mg/m2. In this study of the tron microscopy to evaluate tissue obtained from right heart biopsy for epirubicin-induced cardiac damage. Northern California Oncology Group, myofibrillar loss and sarcoplasmic vacuolization were identified and shown to be identical to those previously described for doxorubicin.