Cardiotoxicity of Epirubicin and Doxorubicin: Assessment by Endomyocardial Biopsy1
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Diagnosis and Treatment of Myocarditides
DIAGNOSIS AND TREATMENT OF MYOCARDITIDES Clinical guidelines Task force for preparing the text of recommendations Chairperson: Professor S.N. Tereshchenko (Moscow), Task force members: I.V. Zhirov (MD, Moscow), Professor V.P. Masenko (MD, Moscow), O.Yu. Narusov (Ph.D., Moscow), S.N. Nasonova (Ph.D., Moscow), Professor A.N. Samko (MD, Moscow), O.V. Stukalova (Ph.D., Moscow) and M.A. Shariya (MD, Moscow) Expert Committee: Professor Arutyunov G.P. (Moscow), Professor Moiseev S.V. (Moscow), Professor Vasyuk Yu.A. (Moscow), Professor Garganeeva A.A. (Tomsk), Professor Glezer M.G. (Moscow region), Professor Tkacheva O.N. (Moscow) Professor Shevchenko A.O. (Moscow), Professor Govorin A.V. (Chita), Professor Azizov V.A. (Azerbaijan), Professor Mirrahimov E.M. (Kyrgyzstan), Professor Abdullaev T.A. (Uzbekistan), Ph.D. Panfale E.M. (Moldova), MD Sudzhaeva O.A. (Belarus) Moscow, 2019 TABLE OF CONTENTS Page INTRODUCTION ............................................................................................................. 4 Evidence Base for Diagnosis and Treatment of Myocarditides…………….……6 I. MYOCARDITIDES CLASSIFICATION ................................................................... 5 1. Fulminant myocarditis. .................................................................................................... 6 2. Acute myocarditis. ........................................................................................................... 6 3. Chronic active myocarditis. ............................................................................................ -

Chemotherapy Protocol
Chemotherapy Protocol BREAST CANCER CYCLOPHOSPHAMIDE-EPIRUBICIN-PACLITAXEL (7 day) Regimen • Breast Cancer – Cyclophosphamide-Epirubicin-Paclitaxel (7 day) Indication • Neoadjuvant / adjuvant therapy of early breast cancer • WHO Performance status 0, 1 Toxicity Drug Adverse Effect Cyclophosphamide Dysuria, haemorrhagic cystitis, taste disturbances Epirubicin Cardio-toxicity, urinary discolouration (red) Hypersensitivity, hypotension, bradycardia, peripheral Paclitaxel neuropathy, myalgia and back pain on administration The adverse effects listed are not exhaustive. Please refer to the relevant Summary of Product Characteristics for full details. Monitoring Regimen • FBC, U&Es and LFTs prior to each cycle. • Ensure adequate cardiac function before starting treatment with epirubicin. Baseline LVEF should be measured, particularly in patients with a history of cardiac problems or in the elderly. Dose Modifications The dose modifications listed are for haematological, liver and renal function only. Dose adjustments may be necessary for other toxicities as well. In principle all dose reductions due to adverse drug reactions should not be re- escalated in subsequent cycles without consultant approval. It is also a general rule for chemotherapy that if a third dose reduction is necessary treatment should be stopped. Please discuss all dose reductions / delays with the relevant consultant before prescribing if appropriate. The approach may be different depending on the clinical circumstances. The following is a general guide only. Version 1.2 (November 2020) Page 1 of 7 Breast – Cyclophosphamide-Epirubicin-Paclitaxel (7 day) Haematological Prior to prescribing the following treatment criteria must be met on day one of treatment. Criteria Eligible Level Neutrophils equal to or more than 1x10 9/L Platelets equal to or more than 100x10 9/L Consider blood transfusion if patient symptomatic of anaemia or has a haemoglobin of less than 8g/dL If counts on day one are below these criteria for neutrophils and platelets then delay treatment for seven days. -

Diagnostic Yield and Safety Profile of Endomyocardial Biopsy in the Non
REC Interv Cardiol. 2019;1(2):99-107 Original article Diagnostic yield and safety profile of endomyocardial biopsy in the non-transplant setting at a Spanish referral center Eusebio García-Izquierdo Jaén,a Juan Francisco Oteo Domínguez,a,* Marta Jiménez Blanco,a Cristina Aguilera Agudo,a Fernando Domínguez,a Jorge Toquero Ramos,a Javier Segovia Cubero,a Clara Salas Antón,b Arturo García-Touchard,a José Antonio Fernández-Díaz,a Rodrigo Estévez-Loureiro,a Francisco Javier Goicolea Ruigómez,a and Luis Alonso-Pulpóna a Servicio de Cardiología, Hospital Universitario Puerta de Hierro, Majadahonda, Madrid, Spain b Servicio de Anatomía Patológica, Hospital Universitario Puerta de Hierro, Majadahonda, Madrid, Spain ABSTRACT Introduction and objectives: Endomyocardial biopsy (EMB) is an established diagnostic tool in myocardial disease. However, this technique may carry major complications. We present the diagnostic and safety results of our experience in EMB in the non-trans- plant setting. We also present the results after the implementation of a technical and safety protocol developed at our center. Methods: We retrospectively analyzed the data of all EMBs conducted in non-transplant patients from September 2004 through July 2018. We compared the diagnostic yield and rate of major complications of EMB in two different periods: before and after implementing the protocol. Results: We included 204 EMBs performed in 190 patients. The most frequent indications were the evaluation of ventricular dys- function or suspected myocarditis (51.5%) and the evaluation of restrictive cardiomyopathy or suspected infiltrative disease (44.6%). One hundred and seventy-two EMBs were performed in the right cardiac chambers (84.3%) and 30 EMBs in the left cardiac chambers (14.7%). -

Intractable Chest Pain in Cardiomyopathy: Treatment by a Novel Technique of Cardiac Cryodenervation with Quantitative Immunohistochemical Assessment of Success
574 Br HeartJ 1993;69:574-577 TECHNIQUE Br Heart J: first published as 10.1136/hrt.70.6.574 on 1 December 1993. Downloaded from Intractable chest pain in cardiomyopathy: treatment by a novel technique of cardiac cryodenervation with quantitative immunohistochemical assessment of success J AR Gaer, L Gordon, J Wharton, J M Polak, K M Taylor, W McKenna, D J Parker Abstract she described episodes of chest pain, usually A novel method of cardiac denervation on exertion but also at rest and at night. The by cryoablation has been developed ex- pain occurred up to 10 times daily and her perimentally. The technique uses liquid exercise tolerance had deteriorated from four nitrogen delivered under pressure to miles to 200 yards. Although she denied ablate the principal sources of cardiac paroxysmal nocturnal dyspnoea, she slept innervation-namely, the adventitia sur- with three pillows. Her medication at this rounding the aorta, pulmonary arteries, time consisted of sotalol (80 mg twice daily) and veins. The technique has been veri- and verapamil (240 mg twice daily). She had fied experimentally both in vivo by four children (aged 6, 8, 10, and 11 years) all physiological means and in vitro by of whom were healthy. She was unaware of a quantitative immunohistochemistry and family history of hypertrophic cardiomyopa- the measurement of myocardial nor- thy, although two members of her family had adrenaline concentrations. A 35 year old died suddenly in middle age. On admission a woman presented with intractable pre- soft pansystolic murmur and considerable cordial pain, normal epicardial coronary obesity were noted. -

BC Cancer Protocol Summary for Neoadjuvant Or Adjuvant Therapy for Breast Cancer Using Fluorouracil, Epirubicin, Cyclophosphamide and Docetaxel
BC Cancer Protocol Summary for Neoadjuvant or Adjuvant Therapy for Breast Cancer Using Fluorouracil, Epirubicin, Cyclophosphamide and DOCEtaxel Protocol Code BRAJFECD Tumour Group Breast Contact Physician Dr. Stephen Chia ELIGIBILITY: . Node positive (any T, N1-3) or high risk, node negative early stage breast cancer . Less than or equal to 65 years of age or fit patients greater than 65 years deemed appropriate by supervising physician . ECOG 0-1 . HER-2 negative . Adequate renal and hepatic function . Adequate cardiac function EXCLUSIONS: . ECOG 2-4 . Significant hepatic dysfunction . Congestive heart failure (LVEF less than 45%) or other significant heart disease . Greater than or equal to grade 2 sensory or motor neuropathy . Pregnancy or lactation . Unsuitable for aggressive adjuvant chemotherapy TESTS: . Baseline: CBC & diff, platelets, creatinine, bilirubin, ALT, Alk Phos, LDH, GGT . Before each treatment (Day 1): CBC & diff, platelets. Prior to Cycle #4: CBC & diff, platelets, bilirubin, ALT, Alk Phos (see Precaution #5 for guidelines regarding hepatic dysfunction and DOCEtaxel). If clinically indicated: bilirubin, ALT, Alk Phos, creatinine, protein level, albumin, GGT, LDH, urea, MUGA scan or echocardiogram PREMEDICATIONS: . For the 3 cycles of epirubicin, fluorouracil and cyclophosphamide, antiemetic protocol for highly emetogenic chemotherapy (see protocol SCNAUSEA) . For the 3 cycles of DOCEtaxel: Dexamethasone 8 mg PO bid for 3 days, starting one day prior to each DOCEtaxel administration. Patient must receive minimum of 3 doses pre-treatment. Additional antiemetics not usually required. DOCEtaxel-induced onycholysis and cutaneous toxicity of the hands may be prevented by wearing frozen gloves starting 15 minutes before DOCEtaxel infusion until 15 minutes after end of DOCEtaxel infusion; gloves should be changed after 45 minutes of wearing to ensure they remain cold during the entire DOCEtaxel infusion. -

In Advanced Upper Tract Urothelial Carcinoma
ANTICANCER RESEARCH 37 : 1875-1883 (2017) doi:10.21873/anticanres.11525 Comparison of Efficacy of Adjuvant MEC (Methotrexate, Epirubicin and Cisplatin) and GC (Gemcitabine and Cisplatin) in Advanced Upper Tract Urothelial Carcinoma SHENG-CHUN HUNG 1, SHIAN-SHIANG WANG 1,2,3 , CHUN-KUANG YANG 1, JIAN-RI LI 1, CHEN-LI CHENG 1, YEN-CHUAN OU 1, HAO-CHUNG HO 1, KUN-YUAN CHIU 1 and CHUAN-SHU CHEN 1 1Division of Urology, Department of Surgery, Taichung Veterans General Hospital, Taichung, Taiwan, R.O.C.; 2School of Medicine, Chung Shan Medical University, Taichung, Taiwan, R.O.C.; 3Department of Applied Chemistry, National Chi Nan University, Puli, Taiwan, R.O.C. Abstract. Aim: To evaluate the efficacy of methotrexate, (3). Its behavior appears multi-focal and in 17% of cases, epirubicin and cisplatin (MEC) or gemcitabine and cisplatin concurrent bladder cancer is present (4). Furthermore, an (GC) as adjuvant chemotherapy in advanced upper tract estimated 22-47% of patients with UTUC may suffer from urothelium carcinoma (UTUC). Patients and Methods: From bladder recurrence (5) and 2-6% of patients suffer from 2002 January to 2008 December, a total of 70 patients with contralateral recurrence (6). advanced UTUC received radical nephroureterctomy at our A radical nephroureterectomy and bladder cuff excision is Institute with MEC and GC as adjuvant chemotherapy. Disease- standard treatment for UTUC, while offering the benefits of free survival (DFS), cancer-specific survival (CSS) and overall preventing tumor spreading and an entire urinary tract resection survival (OS) among the two groups were evaluated. Results: (7). However, after definite and en bloc surgical removal of the The MEC (n=30) and GC group (n=40) were compared and kidney, it still appears to be a poor prognosis for advanced showed no significant differences in DFS (p=0.859), CSS disease, with a <50% 5-year cancer-specific survival rate in (p=0.722) and OS (p=0.691). -

Natural Products. a History of Success and Continuing Promise for Drug Discovery and Development
Natural Products. A History of Success and Continuing Promise for Drug Discovery and Development Gordon M. Cragg NIH Special Volunteer [email protected] David J. Newman Natural Products Branch Developmental Therapeutics Program National Cancer Institute EARLY DOCUMENTATION OF USE OF MEDICINAL PLANTS http://www.nlm.nih.gov/hmd/collections/archives/index.html • Mesopotamian ~2,600 B. C. E. • Egyptian ~ 1,800 B. C. E. • Chinese – ~1,100 B. C. E. and continuing • Indian ~ 1,000 B. C. E. and continuing • Greek ~ 500 B. C. E. Greco-Roman expertise preserved and coordinated with other traditions by Islamic cultures during the Dark Ages ~ 400-1,100 CE Avicenna. Persian pharmacist, physician, poet, philosopher author: canon medicinae – “final codification of Greco-Roman medicine” Great Moments in Pharmacy Collection APhA Traditional Medicine and Drug Discovery • 80% of the world population resides in developing countries • 80% of people in developing countries utilize plants to meet their primary health care needs • Global pop. ca. 7 billion ca. 4.5 billion people utilize plants to meet their primary health care needs Farnsworth NR, et al. Medicinal Plants in Therapy. Bull. W.H.O. 63:965-981 (1985) Fabricant and Farnsworth, EnViron. Health Perspect. 109, 69-75 (2001) Cordell and Clovard, J. Nat. Prod., 75, 514-525 (2012) Norman Farnsworth 1800s. Discovery of some active principles of major herbal preparations Newman and Cragg. Natural Product Chemistry for Drug Discovery, eds. Buss and Butler, M. S., Royal Soc. Chem., Cambridge, 2010, pp. 3-27 European chemists (apothecaries) revolutionized drug discovery and development. 1817. Sertϋrner reports isolation of morphine from Papaver somniferum. -

Breast Pathway Group – FEC75 (Fluorouracil / Epirubicin / Cyclophosphamide) in Advanced Breast Cancer
Breast Pathway Group – FEC75 (Fluorouracil / Epirubicin / Cyclophosphamide) in Advanced Breast Cancer Indication: First line palliative therapy in selected patients with advanced breast cancer Regimen details: Fluorouracil 600mg/m2 IV Day 1 Epirubicin *75mg/m2 IV Day 1 Cyclophosphamide 600mg/m2 IV Day 1 * Consider using FEC60 regimen in patients > 60 years Administration: Epirubicin IV bolus injection via a fast-running Sodium Chloride 0.9% infusion Fluorouracil IV bolus injection via a fast-running Sodium Chloride 0.9% infusion Cyclophosphamide may be administered as IV bolus injection via a fast-running Sodium Chloride 0.9% infusion or as a short infusion e.g. in 100-250ml Sodium Chloride 0.9% over 30 minutes Frequency: Day 1, every 21 days, for 6 cycles Pre-medication: Not routinely required Anti- emetics: Highly Emetogenic Follow local anti-emetic policy. Supportive medication: Mouthcare as per local policy. Extravasation: Fluorouracil: Irritant Epirubicin: Vesicant Cyclophosphamide: Non-vesicant Epirubicin should be administered with appropriate precautions to prevent extravasation. If there is any possibility that extravasation Version: 1.0 Supersedes: all other versions Approved by LCA Breast Pathway Chemotherapy Lead: Mark Harries November 2014 Reason for Update: LCA Protocol Approved by LCA Joint Delivery Subgroup Co-Chairs: Pauline McCalla & Rebecca Johl Development Prepared by: Anabel Rodriguez Marina Approved by LCA Medicines & Chemotherapy Steering Group Chair: Jamie Ferguson Second check by: Lisa Yuen Date prepared: November 2014 Review Date: November 2016 Disclaimer: The Joint Delivery Chemotherapy Nurse/Oncology Pharmacist Group is a sub-group of the Medicines & Chemotherapy Steering Group (MCSG) working within the London Cancer Alliance Integrated Cancer System (LCA). -
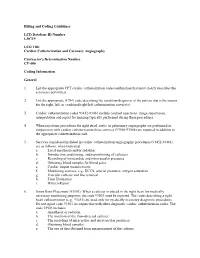
Billing and Coding Guidelines Cardiac Catheterization and Coronary Angiography CV-006
Billing and Coding Guidelines LCD Database ID Number L30719 LCD Title Cardiac Catheterization and Coronary Angiography Contractor's Determination Number CV-006 Coding Information General 1. List the appropriate CPT cardiac catheterization code/combination that most clearly describes the service(s) performed. 2. List the appropriate ICD-9 code describing the condition/diagnosis of the patient that is the reason for the right, left, or combined right/left catheterization service(s). 3. Cardiac catheterization codes 93452-93461 include contrast injections, image supervision, interpretation and report for imaging typically performed during these procedures. 4. When injections procedures for right atrial, aortic or pulmonary angiography are performed in conjunction with cardiac catheterization these services (93566-93568) are reported in addition to the appropriate catheterization code. 5. Services considered included in cardiac catheterization/angiography procedures (93452-93461) are as follows, when indicated: a. Local anesthesia and/or sedation b. Introduction, positioning, and repositioning of catheters c. Recording of intracardiac and intravascular pressures d. Obtaining blood samples for blood gases e. Cardiac output measurements f. Monitoring services, e.g., ECCS, arterial pressures, oxygen saturation g. Vascular catheter and line removal h. Final Evaluation i. Written Report 6. Swan Ganz Placement (93503). When a catheter is placed in the right heart for medically necessary monitoring purposes, the code 93503 must be reported. The codes describing a right heart catheterization (e.g., 93451) are used only for medically necessary diagnostic procedures. Do not report code 93503 in conjunction with other diagnostic cardiac catheterization codes. The code 93503 includes: a. Anesthesia or sedation. b. The insertion of the flow-directed catheter. -

Consensus Statement on Endomyocardial Biopsy
Cardiovascular Pathology 21 (2012) 245–274 Original Article 2011 Consensus statement on endomyocardial biopsy from the Association for European Cardiovascular Pathology and the Society for Cardiovascular Pathology ⁎ ⁎ Ornella Leone a, , John P. Veinot b, , Annalisa Angelini c, Ulrik T. Baandrup d, Cristina Basso c, Gerald Berry e, Patrick Bruneval f, Margaret Burke g, Jagdish Butany h, Fiorella Calabrese c, Giulia d'Amati i, William D. Edwards j, John T. Fallon k, Michael C. Fishbein l, Patrick J. Gallagher m, Marc K. Halushka n, Bruce McManus o, Angela Pucci p, E. René Rodriguez q, Jeffrey E. Saffitz r, Mary N. Sheppard g, Charles Steenbergen n, James R. Stone r, Carmela Tan q, Gaetano Thiene c, Allard C. van der Wal s, Gayle L. Winters r aBologna, Italy bOttawa, Ontario, Canada cPadua, Italy dHjoerring, Denmark eStanford, CA, USA fParis, France gLondon, UK hToronto, Ontario, Canada iRome, Italy jRochester, MN, USA kNew York, NY, USA lLos Angeles, CA, USA mSouthampton, UK nBaltimore, MD, USA oVancouver, BC, Canada pPisa, Italy qCleveland, OH, USA rBoston, MA, USA sAmsterdam, The Netherlands Received 3 August 2011; received in revised form 28 September 2011; accepted 7 October 2011 Abstract The Association for European Cardiovascular Pathology and the Society for Cardiovascular Pathology have produced this position paper concerning the current role of endomyocardial biopsy (EMB) for the diagnosis of cardiac diseases and its contribution to patient management, focusing on pathological issues, with these aims: • Determining appropriate EMB use in the context of current diagnostic strategies for cardiac diseases and providing recommendations for its rational utilization ⁎ Corresponding authors. O. Leone is to be contacted at U.O. -

Epirubicin Ebewe Solution for Injection 2 Mg/Ml 2
NEW ZEALAND DATA SHEET EPIRUBICIN EBEWE (EPIRUBICIN HYDROCHLORIDE) 1. PRODUCT NAME Epirubicin Ebewe solution for injection 2 mg/mL 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Active: Epirubicin hydrochloride Each vial contains 2 mg/mL of epirubicin hydrochloride Epirubicin hydrochloride is a red-orange, almost odourless, hygroscopic powder, sparingly soluble in water and dilute alcohol. List of excipients with known effect: Sodium chloride For the full list of excipients, see Section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Solution for injection (clear red solution, vials). 4. CLINICAL PARTICULARS 4.1. THERAPEUTIC INDICATIONS Epirubicin hydrochloride has produced responses in a wide spectrum of neoplastic diseases, and is indicated for the treatment of breast cancer, gastric cancer, ovarian cancer, small cell lung cancer, lymphoma (non-Hodgkin's lymphoma), advanced/ metastatic soft tissue sarcoma, and superficial bladder cancer (Tis, Ta). In bladder cancer, epirubicin hydrochloride is also indicated in the prophylaxis of recurrence after transurethral resection of stage T1 papillary cancers and stage Ta multifocal papillary cancers (grade 2 and 3). 4.2. DOSE AND METHOD OF ADMINISTRATION Dosage The safety and efficacy of epirubicin in children has not been established. Care in the intravenous administration of epirubicin hydrochloride will reduce the chance of perivenous infiltration. It may also decrease the chance of local reactions, such as urticaria and erythematous streaking (see Section 4.4 Special warnings and precautions for use). Note. The recommended lifetime cumulative dose limit of epirubicin is 900 mg/m2 body surface area. Under conditions of normal recovery from drug induced toxicity (particularly bone marrow depression and stomatitis), the recommended dosage schedule in adults, as described below, is as a single intravenous injection administered at 21 day intervals. -

Complications of Endomyocardial Biopsy in Heart Transplant Patients: a Retrospective Study of 2117 Consecutive Procedures
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Repositório Institucional dos Hospitais da Universidade de Coimbra Complications of Endomyocardial Biopsy in Heart Transplant Patients: A Retrospective Study of 2117 Consecutive Procedures F. Saraiva, V. Matos, L. Gonçalves, M. Antunes, and L.A. Providência ABSTRACT Background. Endomyocardial biopsy (EMB) remains the gold standard for the diagno- sis of graft rejection after heart transplantation (HT). Our purpose was to evaluate the rate of complications of this invasive procedure. Methods. This was a retrospective study of 175 patients, who were transplanted between November 2003 and October 2010 and survived more than 1 month after surgery. We evaluated the number of inconclusive EMB and described the incidence, nature, and subsequent management of several complications associated with this procedure. Results. Over a period of approximately 7 years, we performed 2217 EMB yielding 4972 specimens, namely, an average of 2.3 fragments per procedure. The majority of EMBs (95.3%) were performed by the femoral approach. Only 12 EMB (0.57%) were inconclu- sive. The overall complication rate was 0.71%. During puncture, one patient experienced a vasovagal reaction and another one, a femoral artery false aneurysm. During the biopsy, there was one case of cardiac perforation with tamponade, two cases of supraventricular tachycardia, and three atrioventricular conduction abnormalities. In 19 patients, histolog- ical analysis revealed chordal tissue, but only two patients developed mild tricuspid regurgitation. We observed five cases of coronary artery fistulae. The clinical outcomes were favorable in all cases. Conclusion. EMB proved to be a suitable, safe method to monitor rejection after HT.