Non-Aortic Vascular Findings on Chest CT Angiogram: Including Arch Vessels and Bronchial Arteries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ipsilateral Subclavian Steal in Association with Aberrant Origin of the Left Vertebral Artery from the Aortic Arch
411 Ipsilateral Subclavian Steal in Association with Aberrant Origin of the Left Vertebral Artery from the Aortic Arch John Holder1 Five cases are reported of left subclavian steal syndrome associated with anomalous Eugene F. Binet2 origin of the left vertebral artery from the aortic arch. In all five instances blood flow at Bernard Thompson3 the origin of the left vertebral artery was in an antegrade direction contrary to that usually reported in this condition. The distal subclavian artery was supplied via an extensive collateral network of vessels connecting the vertebral artery to the thyro cervical trunk. If a significant stenosis or occlusion is present within the left subc lavi an artery proximal to the origin of the left vertebral artery, the direction of the bl ood fl ow within the vertebral artery will reverse toward the parent vessel (retrograde flow). This phenomenon occurs when a negative pressure gradient of 20-40 torr exists between the vertebral-basilar artery junction and th e vertebral-subc lavian artery junction [1-3]. We describe five cases of subclavian steal confirmed by angiography where a significant stenosis or occlusion of the left subclavian artery was demonstrated in association with anomalous origin of th e left vertebral artery directly from the aortic arch. In all five cases blood flow at the origin of the left vertebral artery was in an antegrade direction contrary to that more commonly reported in the subclavian steal syndrome. Materials and Methods The five patients were all 44- 58-year-old men. Three sought medical attention for symptoms specificall y related to th e left arm . -

Vessels and Circulation
CARDIOVASCULAR SYSTEM OUTLINE 23.1 Anatomy of Blood Vessels 684 23.1a Blood Vessel Tunics 684 23.1b Arteries 685 23.1c Capillaries 688 23 23.1d Veins 689 23.2 Blood Pressure 691 23.3 Systemic Circulation 692 Vessels and 23.3a General Arterial Flow Out of the Heart 693 23.3b General Venous Return to the Heart 693 23.3c Blood Flow Through the Head and Neck 693 23.3d Blood Flow Through the Thoracic and Abdominal Walls 697 23.3e Blood Flow Through the Thoracic Organs 700 Circulation 23.3f Blood Flow Through the Gastrointestinal Tract 701 23.3g Blood Flow Through the Posterior Abdominal Organs, Pelvis, and Perineum 705 23.3h Blood Flow Through the Upper Limb 705 23.3i Blood Flow Through the Lower Limb 709 23.4 Pulmonary Circulation 712 23.5 Review of Heart, Systemic, and Pulmonary Circulation 714 23.6 Aging and the Cardiovascular System 715 23.7 Blood Vessel Development 716 23.7a Artery Development 716 23.7b Vein Development 717 23.7c Comparison of Fetal and Postnatal Circulation 718 MODULE 9: CARDIOVASCULAR SYSTEM mck78097_ch23_683-723.indd 683 2/14/11 4:31 PM 684 Chapter Twenty-Three Vessels and Circulation lood vessels are analogous to highways—they are an efficient larger as they merge and come closer to the heart. The site where B mode of transport for oxygen, carbon dioxide, nutrients, hor- two or more arteries (or two or more veins) converge to supply the mones, and waste products to and from body tissues. The heart is same body region is called an anastomosis (ă-nas ′tō -mō′ sis; pl., the mechanical pump that propels the blood through the vessels. -

The Variations of the Subclavian Artery and Its Branches Ahmet H
Okajimas Folia Anat. Jpn., 76(5): 255-262, December, 1999 The Variations of the Subclavian Artery and Its Branches By Ahmet H. YUCEL, Emine KIZILKANAT and CengizO. OZDEMIR Department of Anatomy, Faculty of Medicine, Cukurova University, 01330 Balcali, Adana Turkey -Received for Publication, June 19,1999- Key Words: Subclavian artery, Vertebral artery, Arterial variation Summary: This study reports important variations in branches of the subclavian artery in a singular cadaver. The origin of the left vertebral artery was from the aortic arch. On the right side, no thyrocervical trunk was found. The two branches which normally originate from the thyrocervical trunk had a different origin. The transverse cervical artery arose directly from the subclavian artery and suprascapular artery originated from the internal thoracic artery. This variation provides a short route for posterior scapular anastomoses. An awareness of this rare variation is important because this area is used for diagnostic and surgical procedures. The subclavian artery, the main artery of the The variations of the subclavian artery and its upper extremity, also gives off the branches which branches have a great importance both in blood supply the neck region. The right subclavian arises vessels surgery and in angiographic investigations. from the brachiocephalic trunk, the left from the aortic arch. Because of this, the first part of the right and left subclavian arteries differs both in the Subjects origin and length. The branches of the subclavian artery are vertebral artery, internal thoracic artery, This work is based on a dissection carried out in thyrocervical trunk, costocervical trunk and dorsal the Department of Anatomy in the Faculty of scapular artery. -
The Vertebral Artery in the Vascular Lab: What Does It Mean?
The Vertebral Artery in the Vascular Lab: What Does It Mean? Caron Rockman MD Frances and Joseph Ritroto Professor of Surgery Program Director, Vascular Surgery New York University Langone Medical Center Disclosures •None Division of Vascular and Endovascular Surgery Subclavian Steal Occlusion of proximal Subclavian Art Vertebral artery supplies retrograde flow Posterior brain receives decreased flow 55 years + Men > Women more than 2:1 LSA affected 3x more than RSA Division of Vascular and Endovascular Surgery Subclavian Steal Causes: - Arteriosclerosis of subclavian artery (>95% cases) - Embolism - Takayasu’s Arteritis -Dissecting Aneurysm Risk Factors: (similar to CAD) -Smoking -Hypertension -Hyperlipidemia -Hypertension Division of Vascular and Endovascular Surgery Symptoms of Subclavian Steal Vertebrobasilar Insufficiency (posterior circulation symptoms) Light headedness or dizziness Ataxia or Vertigo Visual Disturbance Headache Syncope Confusion Division of Vascular and Endovascular Surgery Symptoms of Subclavian Steal Subclavian Insufficiency Arm weakness, coldness Numbness or “tingling” Arm Claudication with exercise Symptoms can be exacerbated with: Vigorous exercise Sudden turning of head to affected side Division of Vascular and Endovascular Surgery Signs of Subclavian Steal Diminished pulses (radial/ulnar) Discrepant blood pressures in upper extremities (>20mmHg) (Pitfall with bilateral disease) Subclavian Bruit 7 Division of Vascular and Endovascular Surgery Subclavian steal on Duplex Exam Incomplete steal •Striking deceleration of velocity in mid or late systole •High grade stenosis of subclavian rather than occlusion Complete Steal •Complete reversal of flow within the vertebral artery Division of Vascular and Endovascular Surgery Vertebral Retrograde Flow • Reversal of flow in the vertebral artery is a common finding identified on cerebrovascular duplex ultrasound. • The clinical significance and natural history of patients presenting with this finding, however, is poorly understood. -
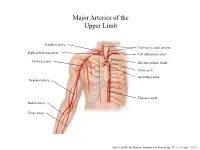
Major Arteries of the Upper Limb
Major Arteries of the Upper Limb Vertebral artery Common carotid arteries Right subclavian artery Left subclavian artery Axillary artery Brachiocephalic trunk Aortic arch Ascending aorta Brachial artery Thoracic aorta Radial artery Ulnar artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.23 Major Arteries of the Abdominal Region Renal artery Celiac trunk Abdominal aorta Superior mesenteric artery Gonadal artery Inferior mesenteric artery Common iliac artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.24 Common iliac artery Internal iliac artery Major Arteries of the External iliac artery Lower Limb Femoral artery Popliteal artery Anterior tibial artery Fibular artery Posterior tibial artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.25 Major Veins of the Upper Limb Internal jugular vein (left) Subclavian vein (right) External jugular vein (left) Axillary vein Brachiocephalic veins Cephalic vein Superior vena cava Brachial vein Basilic vein Median cubital vein Inferior vena cava Radial vein Ulnar vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.28 Major Veins of the Abdominal Cavity – Part 1 Hepatic veins Inferior vena cava Renal vein (left) Gonadal vein (left) Gonadal vein (right) Common iliac vein (left) Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Major Veins of the Abdominal Cavity – Part 2 (Hepatic portal circulation) Hepatic portal vein Splenic vein Inferior mesenteric vein Superior mesenteric vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Common iliac vein (left) Internal iliac vein Major Veins of the External iliac vein Lower Limb Great saphenous vein Femoral vein Popliteal vein Fibular vein Small saphenous vein Anterior tibial Posterior tibial vein vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.30 . -

An Unusual Origin and Course of the Thyroidea Ima Artery, with Absence of Inferior Thyroid Artery Bilaterally
Surgical and Radiologic Anatomy (2019) 41:235–237 https://doi.org/10.1007/s00276-018-2122-1 ANATOMIC VARIATIONS An unusual origin and course of the thyroidea ima artery, with absence of inferior thyroid artery bilaterally Doris George Yohannan1 · Rajeev Rajan1 · Akhil Bhuvanendran Chandran1 · Renuka Krishnapillai1 Received: 31 May 2018 / Accepted: 21 October 2018 / Published online: 25 October 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract We report an unusual origin and course of the thyroidea ima artery in a male cadaver. The ima artery originated from the right subclavian artery very close to origin of the right vertebral artery. The artery coursed anteriorly between the common carotid artery medially and internal jugular vein laterally. It then coursed obliquely, from below upwards, from lateral to medial superficial to common carotid artery, to reach the inferior pole of the right lobe of thyroid and branched repeatedly to supply the anteroinferior and posteroinferior aspects of both the thyroid lobes and isthmus. The superior thyroid arteries were normal. Both the inferior thyroid arteries were absent. The unusual feature of this thyroidea ima artery is its origin from the subclavian artery close to vertebral artery origin, the location being remarkably far-off from the usual near midline position, and the oblique and relatively superficial course. This report is a caveat to neck surgeons to consider such a superficially running vessel to be a thyroidea ima artery. Keywords Thyroid vascular anatomy · Thyroidea ima artery · Artery of Neubauer · Blood supply of thyroid · Variations Introduction (1.1%), transverse scapular (1.1%), or pericardiophrenic or thyrocervical trunk [8, 10]. -

The Dorsal Scapular Artery - a Proposed Term for the Artery to the Rhomboid Muscles
The Dorsal Scapular Artery - A Proposed Term for the Artery to the Rhomboid Muscles DONALD F. HUELKE Department of Anatomy, The University of Michigan, Medical School, Ann Arbor, Michigan The terminology of the arterial supply from the thyrocervical trunk in 77.5% of to the rhomboid and trapezius muscles is sides). (2) That the artery which sup- quite confusing in that each artery has plies the rhomboid muscles take the name been given two different names; names of the nerve along with which it passes, which are related to the variations in the and be designated the dorsal scapular ar- origin of these vessels. According to the tery. This artery arises from the second recent Paris Revision of the terminology or third part of the subclavian artery, sepa- (’55) one of these is the transverse cer- rate from the transverse cervical artery, vical artery, of the thyrocervical trunk, in approximately 70% of the sides. Thus, which gives rise to a superficial and a only one term is used for each artery. deep branch to the trapezius and rhom- If this modification in terminology is to boid muscles respectively. When these be accepted internationally, there must be branches arise separately, the trapezial an agreement among anatomists as to its branch is called the “superficial cervical “usual” site of origin. Only by comparing artery” and that to the rhomboids, the data on the origins of these arteries from “descending scapular artery.” Thus, each various countries can this end be achieved. vessel has two different names. Generally, Therefore, it is the purpose of this report an artery is named by the area of supply, to compare the data on these vessels of irrespective of its origin or variations. -

Arterial Variations Within the Lateral Cervical Region: a Multidetector CT Angiography Study
Int. J. Morphol., 37(3):991-996, 2019. Arterial Variations Within the Lateral Cervical Region: A Multidetector CT Angiography Study Variaciones Arteriales en la Región Cervical Lateral: Estudio Angiográfico por Tomografía Computarizada Multidetector Erdogan Bulbul1; Bahar Yanik1; Emrah Akay1; Vildan Koksal2 & Gulen Demirpolat1 BULBUL, E.; YANIK, B.; AKAY, E.; KOKSAL, V. & DEMIRPOLAT, G. Arterial variations within the lateral cervical region: A multidetector CT angiography study. Int. J. Morphol., 37(3):991-996, 2019. SUMMARY: It is important to know the arterial anatomy within the lateral cervical region before the flap-planning. We evaluated the arterial anatomy in this area using multidetector computed tomography (CT) angiography and our aim was to establish the arterial variations. Both sides of individuals in a total number of 155 carotid CT angiographies are reviewed by using 64-detector CT, retrospectively. The variations of suprascapular artery, superficial cervical artery, dorsal scapular artery that are inclusive of the lateral cervical region were assessed. Three arteries originated individually in 67 (23.8 %) sides. They arose by trunk formation in 214 (76.2 %) sides. The most common type of trunk formation was cervicodorsal trunk (107; 38 %). The others were cervicoscapular trunk, cervicodorsoscapular trunk, dorsoscapular trunk and detected in 66 (23.4 %), 40 (14.3 %), 1 (0.3 %) sides, respectively. The origins of arteries within the lateral cervical region may show variations and they may originate from subclavian artery or its branches individually or by trunk formations. It may be beneficial to know these variations before the reconstructive surgical procedures in head and neck. CT angiography is a non-invasive method that enables to evaluate the arterial anatomy and variations in this area. -

Case Report: Absence of Thyrocervical Trunk
May 2015, Volume 12, Number 2 Case Report: Absence of Thyrocervical Trunk Hassan Hassani Bafrani 1, Homayun Naderian 2, Mohammad Ali Atlasi 2, Abolfazl Azami-Tameh 2* 1. Gametogenesis Research Center, Kashan University of Medical Sciences, Kashan, Iran. 2. Anatomical Sciences Research Center, Kashan University of Medical Sciences, Kashan, Iran. Has been an Assistant Professor in the Department of Anatomy at Kashan University of Medical Sciences since 2011. His postdoctoral research was conducted in the field of neurodegeneration at Neuroanatomy Institute of RWTH Aachen Uni- versity in Germany. His special interest is the study glutamate receptors and transporters in neural survival. Article info: A B S T R A C T Received: 10 Dec. 2014 Accepted: 18 Mar. 2015 The thyrocervical trunk most commonly arises from the upper portion of the first segment of the subclavian artery, close to the medial edge of the scalenus anterior muscle and after short distance is divided to the inferior thyroid, transverse cervical, and suprascapular artery. This study reports important variations in branches of the thyrocervical trunk in Key Words: a singular female cadaver. On the right side, no thyrocervical trunk was found. The two branches which normally originate from the thyrocervical trunk had a different origin. The Subclavian artery, superficial cervical, suprascapular and internal thoracic arteries arose from the common Thyrocervical trunk, Variation trunk artery. An awareness of this rare variation is important because this area is used for complex, Neck posterior diagnostic and surgical procedures. triangle 1. Introduction In some cases, the superficial cervical artery is called the superficial branch of the transverse cervical artery einvestigation of the configuration of the because its course is superficial to the levator-rhomboid human thyrocervical trunk revealed, that muscle group. -

Blood Cell Models
BLOOD CELL MODELS Erythrocyte Platelet BLOOD CELL MODELS Neutrophil Eosinophil BLOOD CELL MODELS Basophil Monocyte BLOOD CELL MODELS Lymphocyte BLOOD CELL MODELS BLOOD CELL MODELS BLOOD CELL MODELS BLOOD CELL MODELS BLOOD SMEAR SLIDES Erythrocyt es Platelets Neutrophi l Eosinophil Lymphocyt e Monocyt e Basophil BLOOD SMEAR SLIDES HEART MODEL Brachiocephalic Artery Left Common Carotid Artery ANTERIOR VIEW LEFT VIEW Left Subclavian Superior Artery Vena Aortic Arch Cava Pulmonary Ligamentum Arteriosus Right Trunk Aortic Aorta Atrium Arch Pulmonary Arteries Pulmonary Coronary Veins Arteries Left Atrium Left Ventricle Right Ventricle Interventricular Sulcus (groove between ventricles) ANTERIOR VIEW Brachiocephalic Artery HEART MODEL ANTERIOR VIEW Left Common Carotid Artery Aortic Pulmonary Superior Left Subclavian Artery Arch Arteries Vena Cava Pulmonary Aortic Trunk Arch Right Pulmonary Semilunar Atrium Bicuspid Valve Aorta Valve Aortic Semilunar Valve Interventricular Septum (Separates ventricles) Tricuspid Valve Left Ventricle Chordae Pulmonary Tendineae Veins Right Left Ventricle Atrium Endocardium (inner layer) Left Myocardium (muscle layer) Papillary Muscles Ventricle Epicardium (outer layer) HEART MODEL Superior Superior Vena Vena Cava Cava RIGHT VIEW Pulmonary Trunk Aorta Right Aorta Atrium Right Right Ventricle Ventricle Fossa Ovalis Tricuspid Valve Right Inferior Atrium Vena Cava HEART MODEL Brachiocephalic Artery Brachiocephalic Left POSTERIOR VIEW Artery Subclavian Left Artery Common Left Carotid Common Artery Carotid Left Artery -

Conventional and Variant Origin of the Transverse Cervical Artery in a Select Kenyan Population
https://dx.doi.org/10.4314/aja.v9i1.11 ORIGINAL COMMUNICATION Anatomy Journal of Africa. 2020. Vol 9 (1): 1727 - 1731 CONVENTIONAL AND VARIANT ORIGIN OF THE TRANSVERSE CERVICAL ARTERY IN A SELECT KENYAN POPULATION Jeremiah Munguti, Fiona Nyaanga, Vincent Kipkorir, Shane Bhupendra, Onyango Marita, Gagandeep Kaur, Thomas Amuti Correspondence to Thomas Amuti, Department of Human Anatomy University of Nairobi Kenya. Email: [email protected] ABSTRACT Data from previous studies have highlighted on the use of transverse cervical artery (TCA) flaps as posterior neck musculocutaneous flaps in reconstructive surgeries. General preference of flap selection relies heavily on the neurovascular supply of the flap in question and even though known, the transverse cervical artery has been shown to vary among populations, therefore affecting its use as a potential flap. Additionally, variant points of origin of the trans-cervical artery have been shown to predispose to brachial plexus compression. Our data on the same, however, remains partly elucidated and therefore a study aimed at describing the conventional and variant origin of the TCA in a Kenyan population would aid in deciding on its use as musculocutaneous flaps and determining the possible prevalence of brachial plexus compression because of its variant origin. The origin of the transverse cervical artery was studied bilaterally in 26 adult Kenyan cadavers in the Department of Human Anatomy, University of Nairobi. As regards their origin, the different types were photographed and grouped into five: Types I to V relative to its origin. The data collected was then analysed using SPSS version 21 and findings presented as percentages. The findings were presented in a bar graph and pie chart. -

Branching Pattern of Collateral Branches of the Subclavian Artery
SMGr up Research Article SM Journal of Branching Pattern of Collateral Clinical Anatomy Branches of the Subclavian Artery Philippe Manyacka Ma Nyemb1,2*, Christian Fontaine3, Xavier Demondion3, Maurice Demeulaere3, Fabien Descamps3 and Jean-Marc Ndoye4 1Laboratory of Anatomy and Organogenesis, Gaston Berger University, Sénégal 2Department of General Surgery, Regional Hospital, Sénégal 3Laboratory of Anatomy, Henri Warembourg Faculty of Medicine, University of Lille 2, France 4Laboratory of Anatomy and Organogenesis, Cheikh Anta Diop University, Sénégal Article Information Abstract Received date: Feb 17, 2018 Introduction: The arteries of the posterior cervical triangle (lateral cervical region) are frequently used for Accepted date: Feb 26, 2018 flap design in plastic and reconstructive surgery. In particular, the musculocutaneous flaps, such as the flap of the lower trapezius and the dorsal scapular flap, are based on the integrity and functional availability of the dorsal Published date: Mar 01, 2018 scapular artery. Likewise, the cervico-dorsal and cervico-scapular flaps are based on the superficial cervical artery. We can assume that the mode of birth of these arteries - and the possibility of their origin directly from the *Corresponding author subclavian artery - will have consequences on their vascular dynamics. These consequences can result in good or bad viability of the irrigated flaps. The objective of the present study was to highlight the birth modalities of the Philippe Manyacka Ma Nyemb, subclavian artery branches. Laboratory of Anatomy and Material and Methods: Dissection was performed in 58 anatomical regions from 32 non-formalin fixed Organogenesis, Faculty of medicine, cadavers. The cadavers had no history of surgery or deformity in the areas targeted for dissection (supraclavicular Gaston Berger University, Saint-Louis, and dorsal regions).