Poster Abstracts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Androgen Excess in Breast Cancer Development: Implications for Prevention and Treatment
26 2 Endocrine-Related G Secreto et al. Androgen excess in breast 26:2 R81–R94 Cancer cancer development REVIEW Androgen excess in breast cancer development: implications for prevention and treatment Giorgio Secreto1, Alessandro Girombelli2 and Vittorio Krogh1 1Epidemiology and Prevention Unit, Fondazione IRCCS – Istituto Nazionale dei Tumori, Milano, Italy 2Anesthesia and Critical Care Medicine, ASST – Grande Ospedale Metropolitano Niguarda, Milano, Italy Correspondence should be addressed to G Secreto: [email protected] Abstract The aim of this review is to highlight the pivotal role of androgen excess in the Key Words development of breast cancer. Available evidence suggests that testosterone f breast cancer controls breast epithelial growth through a balanced interaction between its two f ER-positive active metabolites: cell proliferation is promoted by estradiol while it is inhibited by f ER-negative dihydrotestosterone. A chronic overproduction of testosterone (e.g. ovarian stromal f androgen/estrogen balance hyperplasia) results in an increased estrogen production and cell proliferation that f androgen excess are no longer counterbalanced by dihydrotestosterone. This shift in the androgen/ f testosterone estrogen balance partakes in the genesis of ER-positive tumors. The mammary gland f estradiol is a modified apocrine gland, a fact rarely considered in breast carcinogenesis. When f dihydrotestosterone stimulated by androgens, apocrine cells synthesize epidermal growth factor (EGF) that triggers the ErbB family receptors. These include the EGF receptor and the human epithelial growth factor 2, both well known for stimulating cellular proliferation. As a result, an excessive production of androgens is capable of directly stimulating growth in apocrine and apocrine-like tumors, a subset of ER-negative/AR-positive tumors. -

Progestin-Only Systemic Hormone Therapy for Menopausal Hot Flashes
EDITORIAL Progestin-only systemic hormone therapy for menopausal hot flashes Clinicians treating postmenopausal hot flashes often recommend “systemic estrogen treatment.” However, progestin-only therapy also can effectively treat hot flashes and is an option for women with a contraindication to estrogen therapy. Robert L. Barbieri, MD Editor in Chief, OBG MANAGEMENT Chair, Obstetrics and Gynecology Brigham and Women’s Hospital Boston, Massachusetts Kate Macy Ladd Professor of Obstetrics, Gynecology and Reproductive Biology Harvard Medical School he field of menopause medi- women. In one study, 133 postmeno- in postmenopausal women with cine is dominated by studies pausal women with an average age an American Heart Association risk T documenting the effective- of 55 years and approximately 3 years score greater than 10% over 10 years.3 ness of systemic estrogen or estro- from their last menstrual period were Additional contraindications to sys- gen-progestin hormone therapy for randomly assigned to 12 weeks of temic estrogen include women with the treatment of hot flashes caused treatment with placebo or micronized cardiac disease who have a throm- by hypoestrogenism. The effective- progesterone 300 mg daily taken at bophilia, such as the Factor V Leiden ness of progestin-only systemic bedtime.1 Mean serum progesterone mutation.4 hormone therapy for the treatment levels were 0.28 ng/mL (0.89 nM) and For women who are at high risk of hot flashes is much less studied 27 ng/mL (86 nM) in the women taking for estrogen-induced cardiovascu- and seldom is utilized in clinical placebo and micronized progesterone, lar events, micronized progesterone practice. -

Recapturing Our Identity Through Arts and Crafts" Event to Make Sure That Doesn't Occur
Rez Car Show Teaching Hammock Youth Conference “Looking Back at the Seminole Trail” Page 3 Page 13 Page 14 Presort Standard U.S. Postage Paid S. Florida, FL Permit No. 1624 “Voice of the Unconquered” 50¢ www.seminoletribe.com Volume XXIV • Number 11 August 15, 2003 2003-2004 Seminole Princesses Hollywood Youth Conference Visits Historical Sites “Looking Back at the Seminole Trail” ORLANDO — Members of the Hollywood Youth Conference journeyed back in time, visiting the historic grounds of Fort King, Castillo de San Marcos, and the infamous Dade Battlefield. "Looking Back at the Seminole Trail" offered Seminoles a look into their distinguished past. From July 7 through 11, Children and adults learned about the brave warriors who refused to relin- quish their land, their homes, and their way of life. The Seminoles fought back against the U.S. Army and never signed a treaty, which is why the Seminoles are known as "The Unconquered." On Tuesday July 8, Chairman Mitchell Cypress, President Moses B. Osceola, Hollywood Council Representative Max B. Osceola, and Michael Kelly Hollywood Board Representative David DeHass Dan Osceola prefers using cypress wood for his carvings. spoke to everyone in attendance. They stressed the importance of the Youth Conference and wanted each and everyone to get something out of it. "As a youth, we didn't get much of a chance to see all these historic sites. We only read about Recapturing Our them. You all have the opportunity to see history," said Mitchell Cypress. Moses Osceola stated, "The staff has planned Identity Through some great things for you this week. -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

6 Ways Your Brain Transforms During Menopause
6 Ways Your Brain Transforms During Menopause By Aviva Patz Movies and TV shows have gotten a lot of laughs out of menopause, with its dramatic hot flashes and night sweats. But the midlife transition out of our reproductive years—marked by yo-yoing of hormones, mostly estrogen—is a serious quality-of-life issue for many women, and as we're now learning, may leave permanent marks on our health. "There is a critical window hypothesis in that what is done to treat the symptoms and risk factors during perimenopause predicts future health and symptoms," explains Diana Bitner, MD, assistant professor at Michigan State University College of Human Medicine and author of I Want to Age Like That: Healthy Aging Through Midlife and Menopause. "If women act on the mood changes in perimenopause and get healthy and take estrogen, the symptoms are much better immediately and also lifelong." (Going through menopause and your hormones are out of whack? Then check out The Hormone Reset Diet to balance your hormones and lose weight.) For many decades, the mantra has been that the only true menopausal symptoms are hot flashes and vaginal dryness. Certainly they're the easiest signs to spot! But we have estrogen receptors throughout the brain and body, so when estrogen levels change, we experience the repercussions all over—especially when it comes to how we think and feel. Two large studies, including one of the nation's longest longitudinal investigations, have revealed that there's a lot going on in the brain during this transition. "Before it was hard to tease out: How much of this is due to the ovaries aging and how much is due to the whole body aging?" says Pauline Maki, PhD, professor of psychiatry and psychology at the University of Illinois at Chicago and Immediate Past President of the North American Menopause Society (NAMS). -

Memorandum Date: June 6, 2014
DEPARTMENT OF HEALTH & HUMAN SERVICES Public Health Service Food and Drug Administration Memorandum Date: June 6, 2014 From: Bisphenol A (BPA) Joint Emerging Science Working Group Smita Baid Abraham, M.D. ∂, M. M. Cecilia Aguila, D.V.M. ⌂, Steven Anderson, Ph.D., M.P.P.€* , Jason Aungst, Ph.D.£*, John Bowyer, Ph.D. ∞, Ronald P Brown, M.S., D.A.B.T.¥, Karim A. Calis, Pharm.D., M.P.H. ∂, Luísa Camacho, Ph.D. ∞, Jamie Carpenter, Ph.D.¥, William H. Chong, M.D. ∂, Chrissy J Cochran, Ph.D.¥, Barry Delclos, Ph.D.∞, Daniel Doerge, Ph.D.∞, Dongyi (Tony) Du, M.D., Ph.D. ¥, Sherry Ferguson, Ph.D.∞, Jeffrey Fisher, Ph.D.∞, Suzanne Fitzpatrick, Ph.D. D.A.B.T. £, Qian Graves, Ph.D.£, Yan Gu, Ph.D.£, Ji Guo, Ph.D.¥, Deborah Hansen, Ph.D. ∞, Laura Hungerford, D.V.M., Ph.D.⌂, Nathan S Ivey, Ph.D. ¥, Abigail C Jacobs, Ph.D.∂, Elizabeth Katz, Ph.D. ¥, Hyon Kwon, Pharm.D. ∂, Ifthekar Mahmood, Ph.D. ∂, Leslie McKinney, Ph.D.∂, Robert Mitkus, Ph.D., D.A.B.T.€, Gregory Noonan, Ph.D. £, Allison O’Neill, M.A. ¥, Penelope Rice, Ph.D., D.A.B.T. £, Mary Shackelford, Ph.D. £, Evi Struble, Ph.D.€, Yelizaveta Torosyan, Ph.D. ¥, Beverly Wolpert, Ph.D.£, Hong Yang, Ph.D.€, Lisa B Yanoff, M.D.∂ *Co-Chair, € Center for Biologics Evaluation & Research, £ Center for Food Safety and Applied Nutrition, ∂ Center for Drug Evaluation and Research, ¥ Center for Devices and Radiological Health, ∞ National Center for Toxicological Research, ⌂ Center for Veterinary Medicine Subject: 2014 Updated Review of Literature and Data on Bisphenol A (CAS RN 80-05-7) To: FDA Chemical and Environmental Science Council (CESC) Office of the Commissioner Attn: Stephen M. -
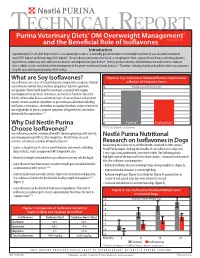
What Are Soy Isoflavones? Figure 2: Soy Isoflavones Reduced Plasma Isoprostanes Soy Isoflavones Are a Class of Natural Bioactive Compounds in Soybeans
TECHNICAL REPORT Purina Veterinary Diets® OM Overweight Management® brand canine dry formula and the Beneficial Role of Isoflavones Introduction Approximately 35% of adult dogs in the U.S. are overweight or obese1. A markedly greater incidence of overweight and obesity was observed in neutered male (59% higher) and female dogs (40% higher)1. Chronic obesity can increase the risk of, or complications from, several chronic diseases including diabetes, hypertension, pulmonary and cardiovascular disease, and degenerative joint disease2. Obesity produces chronic, mild inflammation and increases oxidative stress, which, in turn, contributes to the development of the above-mentioned chronic diseases.3,4 Therefore, reducing obesity and oxidative stress can promote a long life span and improved quality of life in dogs. What are Soy Isoflavones? Figure 2: Soy Isoflavones Reduced Plasma Isoprostanes Soy isoflavones are a class of natural bioactive compounds in soybeans. Natural a Marker of Oxidative Stress soy isoflavones include three chemical compounds: daidzein, genistein, 5 Plasma Isoprostanes (ng/ml) and glycitein. Many health benefits have been associated with regular consumption of soy products. In humans, soy has been found to reduce the 4 risk of cardiovascular disease and certain types of cancer (breast and prostate cancer); relieve a number of problems in post menopausal women including 3 hot flashes, osteoporosis, and decline in cognitive function; reduce cholesterol and triglycerides in plasma; improve symptoms of hypertension; and reduce 2 abdominal fat accumulation.5,6,7 1 Why Did Nestlé Purina 0 Control Isoflavones* Choose Isoflavones? *P<0.01 for Control vs. Isoflavones Soy isoflavones provide a number of benefits for managing dogs with obesity, and reducing rebound effects after weight loss. -

Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis
ORIGINAL ARTICLE Effect of Dehydroepiandrosterone and Testosterone Supplementation on Systemic Lipolysis Ana E. Espinosa De Ycaza, Robert A. Rizza, K. Sreekumaran Nair, and Michael D. Jensen Division of Endocrinology, Endocrine Research Unit, Mayo Clinic, Rochester, Minnesota 55905 Downloaded from https://academic.oup.com/jcem/article/101/4/1719/2804555 by guest on 24 September 2021 Context: Dehydroepiandrosterone (DHEA) and T hormones are advertised as antiaging, antiobe- sity products. However, the evidence that these hormones have beneficial effects on adipose tissue metabolism is limited. Objective: The objective of the study was to determine the effect of DHEA and T supplementation on systemic lipolysis during a mixed-meal tolerance test (MMTT) and an iv glucose tolerance test (IVGTT). Design: This was a 2-year randomized, double-blind, placebo-controlled trial. Setting: The study was conducted at a general clinical research center. Participants: Sixty elderly women with low DHEA concentrations and 92 elderly men with low DHEA and bioavailable T concentrations participated in the study. Interventions: Elderly women received 50 mg DHEA (n ϭ 30) or placebo (n ϭ 30). Elderly men received 75 mg DHEA (n ϭ 30),5mgT(nϭ 30), or placebo (n ϭ 32). Main Outcome Measures: In vivo measures of systemic lipolysis (palmitate rate of appearance) during a MMTT or IVGTT. Results: At baseline there was no difference in insulin suppression of lipolysis measured during MMTT and IVGTT between the treatment groups and placebo. For both sexes, a univariate analysis showed no difference in changes in systemic lipolysis during the MMTT or IVGTT in the DHEA group and T group when compared with placebo. -

Properties and Units in Clinical Pharmacology and Toxicology
Pure Appl. Chem., Vol. 72, No. 3, pp. 479–552, 2000. © 2000 IUPAC INTERNATIONAL FEDERATION OF CLINICAL CHEMISTRY AND LABORATORY MEDICINE SCIENTIFIC DIVISION COMMITTEE ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)# and INTERNATIONAL UNION OF PURE AND APPLIED CHEMISTRY CHEMISTRY AND HUMAN HEALTH DIVISION CLINICAL CHEMISTRY SECTION COMMISSION ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)§ PROPERTIES AND UNITS IN THE CLINICAL LABORATORY SCIENCES PART XII. PROPERTIES AND UNITS IN CLINICAL PHARMACOLOGY AND TOXICOLOGY (Technical Report) (IFCC–IUPAC 1999) Prepared for publication by HENRIK OLESEN1, DAVID COWAN2, RAFAEL DE LA TORRE3 , IVAN BRUUNSHUUS1, MORTEN ROHDE1, and DESMOND KENNY4 1Office of Laboratory Informatics, Copenhagen University Hospital (Rigshospitalet), Copenhagen, Denmark; 2Drug Control Centre, London University, King’s College, London, UK; 3IMIM, Dr. Aiguader 80, Barcelona, Spain; 4Dept. of Clinical Biochemistry, Our Lady’s Hospital for Sick Children, Crumlin, Dublin 12, Ireland #§The combined Memberships of the Committee and the Commission (C-NPU) during the preparation of this report (1994–1996) were as follows: Chairman: H. Olesen (Denmark, 1989–1995); D. Kenny (Ireland, 1996); Members: X. Fuentes-Arderiu (Spain, 1991–1997); J. G. Hill (Canada, 1987–1997); D. Kenny (Ireland, 1994–1997); H. Olesen (Denmark, 1985–1995); P. L. Storring (UK, 1989–1995); P. Soares de Araujo (Brazil, 1994–1997); R. Dybkær (Denmark, 1996–1997); C. McDonald (USA, 1996–1997). Please forward comments to: H. Olesen, Office of Laboratory Informatics 76-6-1, Copenhagen University Hospital (Rigshospitalet), 9 Blegdamsvej, DK-2100 Copenhagen, Denmark. E-mail: [email protected] Republication or reproduction of this report or its storage and/or dissemination by electronic means is permitted without the need for formal IUPAC permission on condition that an acknowledgment, with full reference to the source, along with use of the copyright symbol ©, the name IUPAC, and the year of publication, are prominently visible. -

UFC PROHIBITED LIST Effective June 1, 2021 the UFC PROHIBITED LIST
UFC PROHIBITED LIST Effective June 1, 2021 THE UFC PROHIBITED LIST UFC PROHIBITED LIST Effective June 1, 2021 PART 1. Except as provided otherwise in PART 2 below, the UFC Prohibited List shall incorporate the most current Prohibited List published by WADA, as well as any WADA Technical Documents establishing decision limits or reporting levels, and, unless otherwise modified by the UFC Prohibited List or the UFC Anti-Doping Policy, Prohibited Substances, Prohibited Methods, Specified or Non-Specified Substances and Specified or Non-Specified Methods shall be as identified as such on the WADA Prohibited List or WADA Technical Documents. PART 2. Notwithstanding the WADA Prohibited List and any otherwise applicable WADA Technical Documents, the following modifications shall be in full force and effect: 1. Decision Concentration Levels. Adverse Analytical Findings reported at a concentration below the following Decision Concentration Levels shall be managed by USADA as Atypical Findings. • Cannabinoids: natural or synthetic delta-9-tetrahydrocannabinol (THC) or Cannabimimetics (e.g., “Spice,” JWH-018, JWH-073, HU-210): any level • Clomiphene: 0.1 ng/mL1 • Dehydrochloromethyltestosterone (DHCMT) long-term metabolite (M3): 0.1 ng/mL • Selective Androgen Receptor Modulators (SARMs): 0.1 ng/mL2 • GW-1516 (GW-501516) metabolites: 0.1 ng/mL • Epitrenbolone (Trenbolone metabolite): 0.2 ng/mL 2. SARMs/GW-1516: Adverse Analytical Findings reported at a concentration at or above the applicable Decision Concentration Level but under 1 ng/mL shall be managed by USADA as Specified Substances. 3. Higenamine: Higenamine shall be a Prohibited Substance under the UFC Anti-Doping Policy only In-Competition (and not Out-of- Competition). -

Applications of in Silico Methods to Analyze the Toxicity and Estrogen T Receptor-Mediated Properties of Plant-Derived Phytochemicals ∗ K
Food and Chemical Toxicology 125 (2019) 361–369 Contents lists available at ScienceDirect Food and Chemical Toxicology journal homepage: www.elsevier.com/locate/foodchemtox Applications of in silico methods to analyze the toxicity and estrogen T receptor-mediated properties of plant-derived phytochemicals ∗ K. Kranthi Kumara, P. Yugandharb, B. Uma Devia, T. Siva Kumara, N. Savithrammab, P. Neerajaa, a Department of Zoology, Sri Venkateswara University, Tirupati, 517502, India b Department of Botany, Sri Venkateswara University, Tirupati, 517502, India ARTICLE INFO ABSTRACT Keywords: A myriad of phytochemicals may have potential to lead toxicity and endocrine disruption effects by interfering Phytochemicals with nuclear hormone receptors. In this examination, the toxicity and estrogen receptor−binding abilities of a QSAR modeling set of 2826 phytochemicals were evaluated. The endpoints mutagenicity, carcinogenicity (both CAESAR and ISS Toxicity models), developmental toxicity, skin sensitization and estrogen receptor relative binding affinity (ER_RBA) Nuclear hormone receptor binding were studied using the VEGA QSAR modeling package. Alongside the predictions, models were providing pos- Self−Organizing maps sible information for applicability domains and most similar compounds as similarity sets from their training Clustering and classification schemes sets. This information was subjected to perform the clustering and classification of chemicals using Self−Organizing Maps. The identified clusters and their respective indicators were considered as potential hotspot structures for the specified data set analysis. Molecular screening interpretations of models wereex- hibited accurate predictions. Moreover, the indication sets were defined significant clusters and cluster in- dicators with probable prediction labels (precision). Accordingly, developed QSAR models showed good pre- dictive abilities and robustness, which observed from applicability domains, representation spaces, clustering and classification schemes. -

Estetrol: New Perspectives for HRT in Menopause and Breast Cancer
Graziottin A. Singer C. Kubista E. Visser M. Coelingh Bennink H. Estetrol: new perspectives for HRT in menopause and breast cancer patients V Annual International Congress on Human Reproduction on "Family Reproductive Health", Moscow, Russia, January 18-21, 2011 Estetrol: new perspectives for HRT in menopause and breast cancer patients Alessandra Graziottin *, Christian Singer **, Ernst Kubista **, Monique Visser *** and Herjan J.T. Coelingh Bennink *** * Professor at the University of Florence, Italy – Director, Center of Gynaecology, H San Raffaele Resnati, Milan, Italy ** Akademisches Krankenhaus Wien, Wien, Austria *** Pantarhei Bioscience, Zeist, The Netherlands Estetrol (E 4) is a foetal estrogen, produced by the foetal liver during pregnancy only. It has a selective ERalpha and ERbeta receptor bindin g with preference for ERalpha, with antagonist action. E 4 is present at 9 weeks of gestation, with exponential increase of synthesis and blood levels. At term the foetus produces about 3 mg/day. Elimination half-life is 28 hours. Potential applications in women’s life-span include: contraception, hormone replacement therapy (HRT), specifically for vasomotor symptoms, vulvovaginal atrophy and osteoporosis, and therapy of breast cancer. Preliminary data support its efficacy in the treatment of: hot flushes, with significant reduction; in the maturation of the vaginal mucosa, with significant increase of superficial cells at the cytological evaluation; a dose dependent effect on the endometrium: low doses such as 2 mg of Estetrol/day, sufficient to treat a number of symptoms, do not stimulate the endometrium; a significant protective effect on bone: this growing set of data suggest that E 4 could have a new, significant role in the treatment of menopausal symptoms, with an extraordinary safe profile.