Expression Analysis and Functional Significance of Chondroitin Sulphate Proteoglycans and Heparan Sulphate Proteoglycans in Prostate Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Serine Proteases with Altered Sensitivity to Activity-Modulating
(19) & (11) EP 2 045 321 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 08.04.2009 Bulletin 2009/15 C12N 9/00 (2006.01) C12N 15/00 (2006.01) C12Q 1/37 (2006.01) (21) Application number: 09150549.5 (22) Date of filing: 26.05.2006 (84) Designated Contracting States: • Haupts, Ulrich AT BE BG CH CY CZ DE DK EE ES FI FR GB GR 51519 Odenthal (DE) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • Coco, Wayne SK TR 50737 Köln (DE) •Tebbe, Jan (30) Priority: 27.05.2005 EP 05104543 50733 Köln (DE) • Votsmeier, Christian (62) Document number(s) of the earlier application(s) in 50259 Pulheim (DE) accordance with Art. 76 EPC: • Scheidig, Andreas 06763303.2 / 1 883 696 50823 Köln (DE) (71) Applicant: Direvo Biotech AG (74) Representative: von Kreisler Selting Werner 50829 Köln (DE) Patentanwälte P.O. Box 10 22 41 (72) Inventors: 50462 Köln (DE) • Koltermann, André 82057 Icking (DE) Remarks: • Kettling, Ulrich This application was filed on 14-01-2009 as a 81477 München (DE) divisional application to the application mentioned under INID code 62. (54) Serine proteases with altered sensitivity to activity-modulating substances (57) The present invention provides variants of ser- screening of the library in the presence of one or several ine proteases of the S1 class with altered sensitivity to activity-modulating substances, selection of variants with one or more activity-modulating substances. A method altered sensitivity to one or several activity-modulating for the generation of such proteases is disclosed, com- substances and isolation of those polynucleotide se- prising the provision of a protease library encoding poly- quences that encode for the selected variants. -

Supplemental Table S1. Primers for Sybrgreen Quantitative RT-PCR Assays
Supplemental Table S1. Primers for SYBRGreen quantitative RT-PCR assays. Gene Accession Primer Sequence Length Start Stop Tm GC% GAPDH NM_002046.3 GAPDH F TCCTGTTCGACAGTCAGCCGCA 22 39 60 60.43 59.09 GAPDH R GCGCCCAATACGACCAAATCCGT 23 150 128 60.12 56.52 Exon junction 131/132 (reverse primer) on template NM_002046.3 DNAH6 NM_001370.1 DNAH6 F GGGCCTGGTGCTGCTTTGATGA 22 4690 4711 59.66 59.09% DNAH6 R TAGAGAGCTTTGCCGCTTTGGCG 23 4797 4775 60.06 56.52% Exon junction 4790/4791 (reverse primer) on template NM_001370.1 DNAH7 NM_018897.2 DNAH7 F TGCTGCATGAGCGGGCGATTA 21 9973 9993 59.25 57.14% DNAH7 R AGGAAGCCATGTACAAAGGTTGGCA 25 10073 10049 58.85 48.00% Exon junction 9989/9990 (forward primer) on template NM_018897.2 DNAI1 NM_012144.2 DNAI1 F AACAGATGTGCCTGCAGCTGGG 22 673 694 59.67 59.09 DNAI1 R TCTCGATCCCGGACAGGGTTGT 22 822 801 59.07 59.09 Exon junction 814/815 (reverse primer) on template NM_012144.2 RPGRIP1L NM_015272.2 RPGRIP1L F TCCCAAGGTTTCACAAGAAGGCAGT 25 3118 3142 58.5 48.00% RPGRIP1L R TGCCAAGCTTTGTTCTGCAAGCTGA 25 3238 3214 60.06 48.00% Exon junction 3124/3125 (forward primer) on template NM_015272.2 Supplemental Table S2. Transcripts that differentiate IPF/UIP from controls at 5%FDR Fold- p-value Change Transcript Gene p-value p-value p-value (IPF/UIP (IPF/UIP Cluster ID RefSeq Symbol gene_assignment (Age) (Gender) (Smoking) vs. C) vs. C) NM_001178008 // CBS // cystathionine-beta- 8070632 NM_001178008 CBS synthase // 21q22.3 // 875 /// NM_0000 0.456642 0.314761 0.418564 4.83E-36 -2.23 NM_003013 // SFRP2 // secreted frizzled- 8103254 NM_003013 -

Knockdown of Carboxypeptidase A6 in Zebrafish Larvae Reduces Response to Seizure-Inducing Drugs and Causes Changes in the Level of Mrnas Encoding Signaling Molecules
RESEARCH ARTICLE Knockdown of Carboxypeptidase A6 in Zebrafish Larvae Reduces Response to Seizure-Inducing Drugs and Causes Changes in the Level of mRNAs Encoding Signaling Molecules Mark William Lopes1, Matthew R. Sapio2, Rodrigo B. Leal1, Lloyd D. Fricker2,3* a11111 1 Programa de Pós-graduação em Bioquímica, Departamento de Bioquímica, Centro de Ciências Biológicas, Universidade Federal de Santa Catarina, Florianópolis, SC, Brazil, 2 Department of Neuroscience, Albert Einstein College of Medicine, Bronx, New York, United States of America, 3 Department of Molecular Pharmacology, Albert Einstein College of Medicine, Bronx, New York, United States of America * [email protected] OPEN ACCESS Citation: Lopes MW, Sapio MR, Leal RB, Fricker LD (2016) Knockdown of Carboxypeptidase A6 in Abstract Zebrafish Larvae Reduces Response to Seizure- Inducing Drugs and Causes Changes in the Level of Carboxypeptidase A6 (CPA6) is an extracellular matrix metallocarboxypeptidase that mod- mRNAs Encoding Signaling Molecules. PLoS ONE ulates peptide and protein function by removal of hydrophobic C-terminal amino acids. 11(4): e0152905. doi:10.1371/journal.pone.0152905 Mutations in the human CPA6 gene that reduce enzymatic activity in the extracellular matrix Editor: Giuseppe Biagini, University of Modena and are associated with febrile seizures, temporal lobe epilepsy, and juvenile myoclonic epi- Reggio Emilia, ITALY lepsy. The characterization of these human mutations suggests a dominant mode of inheri- Received: August 26, 2015 tance by haploinsufficiency through loss of function mutations, however the total number of Accepted: March 21, 2016 humans with pathologic mutations in CPA6 identified to date remains small. To better Published: April 6, 2016 understand the relationship between CPA6 and seizures we investigated the effects of mor- pholino knockdown of cpa6 mRNA in zebrafish (Danio rerio) larvae. -

Substrate Specificity and Structural Modeling of Human
International Journal of Molecular Sciences Article Substrate Specificity and Structural Modeling of Human Carboxypeptidase Z: A Unique Protease with a Frizzled-Like Domain Javier Garcia-Pardo 1 , Sebastian Tanco 1,2 , Maria C. Garcia-Guerrero 1, Sayani Dasgupta 3, Francesc Xavier Avilés 1 , Julia Lorenzo 1,* and Lloyd D. Fricker 3,* 1 Institut de Biotecnologia i Biomedicina and Departament de Bioquimica i Biologia Molecular, Universitat Autònoma de Barcelona, 08193 Bellaterra, Barcelona, Spain; [email protected] (J.G.-P.); [email protected] (S.T.); [email protected] (M.C.G.-G.); [email protected] (F.X.A.) 2 BiosenSource BV, B-1800 Vilvoorde, Belgium 3 Department of Molecular Pharmacology, Albert Einstein College of Medicine, Bronx, New York, NY 10461, USA; [email protected] * Correspondence: [email protected] (J.L.); [email protected] (L.D.F.); Tel.: +34-93-5868936 (J.L.); +1-718-430-4225 (L.D.F.) Received: 24 October 2020; Accepted: 14 November 2020; Published: 18 November 2020 Abstract: Metallocarboxypeptidase Z (CPZ) is a secreted enzyme that is distinguished from all other members of the M14 metallocarboxypeptidase family by the presence of an N-terminal cysteine-rich Frizzled-like (Fz) domain that binds Wnt proteins. Here, we present a comprehensive analysis of the enzymatic properties and substrate specificity of human CPZ. To investigate the enzymatic properties, we employed dansylated peptide substrates. For substrate specificity profiling, we generated two different large peptide libraries and employed isotopic labeling and quantitative mass spectrometry to study the substrate preference of this enzyme. Our findings revealed that CPZ has a strict requirement for substrates with C-terminal Arg or Lys at the P10 position. -

CPA6 (Center) Rabbit Polyclonal Antibody – AP51046PU-N | Origene
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for AP51046PU-N CPA6 (Center) Rabbit Polyclonal Antibody Product data: Product Type: Primary Antibodies Applications: WB Recommended Dilution: ELISA: 1/1000. Western Blot: 1/100-1/500. Reactivity: Human Host: Rabbit Isotype: Ig Clonality: Polyclonal Immunogen: KLH conjugated synthetic peptide between 292-323 amino acids from the Central region of Human CPA6. Specificity: This antibody recognizes Human Carboxypeptidase A6 (Center). Formulation: PBS State: Aff - Purified State: Liquid purified Ig fraction Preservative: 0.09% Sodium Azide Concentration: lot specific Purification: Affinity Chromatography on Protein A Conjugation: Unconjugated Storage: Store undiluted at 2-8°C for one month or (in aliquots) at -20°C for longer. Avoid repeated freezing and thawing. Stability: Shelf life: one year from despatch. Gene Name: Homo sapiens carboxypeptidase A6 (CPA6) Database Link: Entrez Gene 57094 Human Q8N4T0 This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 CPA6 (Center) Rabbit Polyclonal Antibody – AP51046PU-N Background: The protein encoded by this gene belongs to the family of carboxypeptidases, which catalyze the release of C-terminal amino acid, and have functions ranging from digestion of food to selective biosynthesis of neuroendocrine peptides. Polymorphic variants and a reciprocal translocation t(6;8)(q26;q13) involving this gene, have been associated with Duane retraction syndrome. Synonyms: CPA6, CPAH, Carboxypeptidase B Note: Molecular Weight: 51008 Da Protein Families: Protease, Secreted Protein Product images: Western blot analysis of Carboxypeptidase A6 Antibody in NCI-H460 cell line lysates (35ug/lane).This demonstrates the CPA6 antibody detected the CPA6 protein (arrow). -

( 12 ) United States Patent
US010245229B2 (12 ) United States Patent ( 10 ) Patent No. : US 10 , 245 ,229 B2 Heartlein et al. (45 ) Date of Patent: Apr. 2 , 2019 ( 54 ) PULMONARY DELIVERY OF MRNA TO ( 56 ) References Cited NON -LUNG TARGET CELLS U . S . PATENT DOCUMENTS ( 71 ) Applicants : Shire Human Genetic Therapies, Inc. , 5 ,705 , 385 A 1 / 1998 Bally et al . Lexington , MA (US ) ; Ethris GmbH , 5 , 965, 434 A 10 / 1999 Wolff et al . Martinsried (DE ) 5 , 976 , 567 A 11 / 1999 Wheeler et al. 5 , 981 ,501 A 11/ 1999 Wheeler et al. 6 ,077 ,835 A 6 / 2000 Hanson et al . (72 ) Inventors : Michael Heartlein , Lexington , MA 6 ,534 , 484 B1 3 / 2003 Wheeler et al . (US ) ; Braydon Charles Guild , 6 ,734 , 171 B1 5 /2004 Saravolac et al. Lexington , MA (US ) ; Frank DeRosa , 6 , 815 ,432 B2 11/ 2004 Wheeler et al . Lexington , MA (US ) ; Carsten 7 , 422 , 902 B1 9 / 2008 Wheeler et al . Rudolph , Krailling ( DE ) ; Christian 7 ,745 ,651 B2 6 /2010 Heyes et al. 7 ,799 , 565 B2 9 /2010 MacLachlan et al. Plank , Wessling (DE ) 7 , 803 ,397 B2 9 / 2010 Heyes et al . 7 , 901, 708 B2 3 / 2011 MacLachlan et al. (73 ) Assignees : Translate Bio , Inc . , Lexington , MA 8 , 101 ,741 B2 1 / 2012 MacLachlan et al . (US ) ; Ethris GmbH , Martinsried (DE ) 8 , 188 , 263 B2 5 / 2012 MacLachlan et al . 8 , 236 , 943 B2 8 / 2012 Lee et al. 8 ,329 ,070 B2 12 /2012 MacLachlan et al . ( * ) Notice : Subject to any disclaimer , the term of this 8 ,513 ,403 B2 8 / 2013 MacLachlan et al. -

(12) United States Patent (10) Patent No.: US 9,358,282 B2 Cobbold Et Al
US009358282B2 (12) United States Patent (10) Patent No.: US 9,358,282 B2 Cobbold et al. (45) Date of Patent: *Jun. 7, 2016 (54) RE-DIRECTED IMMUNOTHERAPY CI2N 7/00 (2013.01); A61K 2039/505 (2013.01); A61K 2039/585 (2013.01); A61 K (71) Applicant: The University of Birmingham, 2039/6056 (2013.01); A61K 2039/627 Birmingham (GB) (2013.01); C07K 2317/24 (2013.01); C07K 2317/622 (2013.01); C07K 2319/33 (2013.01); (72) Inventors: Mark Cobbold, Birmingham (GB); C07K 2319/50 (2013.01); C12N 27.10/16134 David Millar, Birmingham (GB) (2013.01) (73) Assignee: As ther of Birmingham, (58) CPCField ....................of Classification A61K Search 47/48276; A61 K47/4833; A61K 47/48415: A61 K47/48584: A61 K (*) Notice: Subject to any disclaimer, the term of this 47/4863; A61 K 2039,505. A61 K 2039,585, patent is extended or adjusted under 35 A61K2037/6056; A61K 38/2026; CO7K U.S.C. 154(b) by 0 days. 16/2887; C07K 16/32: C07K 14/045 USPC .............. 424/178.1, 134.1, 133.1; 530/387.3, This patent is Subject to a terminal dis- 530/3917 claimer. See application file for complete search history. (21) Appl. No.: 14/660,137 (56) References Cited (22) Filed: Mar 17, 2015 U.S. PATENT DOCUMENTS (65) Prior Publication Data 5,585,089 A 12/1996 Queen et al. 5,693,762 A 12/1997 Queen et al. US 2015/O250868A1 Sep. 10, 2015 5,739,116 A 4, 1998 Hamann et al. 5,767.285 A 6/1998 Hamann et al. -

A Genomic Analysis of Rat Proteases and Protease Inhibitors
A genomic analysis of rat proteases and protease inhibitors Xose S. Puente and Carlos López-Otín Departamento de Bioquímica y Biología Molecular, Facultad de Medicina, Instituto Universitario de Oncología, Universidad de Oviedo, 33006-Oviedo, Spain Send correspondence to: Carlos López-Otín Departamento de Bioquímica y Biología Molecular Facultad de Medicina, Universidad de Oviedo 33006 Oviedo-SPAIN Tel. 34-985-104201; Fax: 34-985-103564 E-mail: [email protected] Proteases perform fundamental roles in multiple biological processes and are associated with a growing number of pathological conditions that involve abnormal or deficient functions of these enzymes. The availability of the rat genome sequence has opened the possibility to perform a global analysis of the complete protease repertoire or degradome of this model organism. The rat degradome consists of at least 626 proteases and homologs, which are distributed into five catalytic classes: 24 aspartic, 160 cysteine, 192 metallo, 221 serine, and 29 threonine proteases. Overall, this distribution is similar to that of the mouse degradome, but significatively more complex than that corresponding to the human degradome composed of 561 proteases and homologs. This increased complexity of the rat protease complement mainly derives from the expansion of several gene families including placental cathepsins, testases, kallikreins and hematopoietic serine proteases, involved in reproductive or immunological functions. These protease families have also evolved differently in the rat and mouse genomes and may contribute to explain some functional differences between these two closely related species. Likewise, genomic analysis of rat protease inhibitors has shown some differences with the mouse protease inhibitor complement and the marked expansion of families of cysteine and serine protease inhibitors in rat and mouse with respect to human. -

Novel Carboxypeptidase A6 (CPA6) Mutations Identified in Patients with Juvenile Myoclonic and Generalized Epilepsy
RESEARCH ARTICLE Novel Carboxypeptidase A6 (CPA6) Mutations Identified in Patients with Juvenile Myoclonic and Generalized Epilepsy Matthew R. Sapio1, Monique Vessaz2, Pierre Thomas3, Pierre Genton4, Lloyd D. Fricker1,5*, Annick Salzmann6* 1 Department of Neuroscience, Albert Einstein College of Medicine, Bronx, NY, United States of America, 2 Department of Genetic Medicine and Laboratory, University Hospitals of Geneva, Geneva, Switzerland, 3 Department of Neurology, University Hospital, Nice, France, 4 Centre Saint Paul, Hôpital Henri Gastaut, Marseille, France, 5 Department of Molecular Pharmacology, Albert Einstein College of Medicine, Bronx, NY, United States of America, 6 Department of Psychiatry, University of Geneva, Geneva, Switzerland a11111 * [email protected] (LDF); [email protected] (AS) Abstract Carboxypeptidase A6 (CPA6) is a peptidase that removes C-terminal hydrophobic amino OPEN ACCESS acids from peptides and proteins. The CPA6 gene is expressed in the brains of humans and Citation: Sapio MR, Vessaz M, Thomas P, Genton P, animals, with high levels of expression during development. It is translated with a prodomain Fricker LD, Salzmann A (2015) Novel (as proCPA6), which is removed before secretion. The active form of CPA6 binds tightly to Carboxypeptidase A6 (CPA6) Mutations Identified in the extracellular matrix (ECM) where it is thought to function in the processing of peptides Patients with Juvenile Myoclonic and Generalized and proteins. Mutations in the CPA6 gene have been identified in patients with temporal Epilepsy. PLoS ONE 10(4): e0123180. doi:10.1371/ journal.pone.0123180 lobe epilepsy and febrile seizures. In the present study, we screened for CPA6 mutations in patients with juvenile myoclonic epilepsy and identified two novel missense mutations: Academic Editor: Coro Paisan-Ruiz, Icahn School of Medicine at Mount Sinai, UNITED STATES Arg36His and Asn271Ser. -

Methods for Inducing Differentiation of Undifferentiated Mammalian Cells Into Osteoblasts
(19) & (11) EP 2 248 896 A2 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 10.11.2010 Bulletin 2010/45 C12N 15/113 (2010.01) A61K 31/713 (2006.01) C12Q 1/68 (2006.01) C12N 5/10 (2006.01) (2006.01) (2006.01) (21) Application number: 10174533.9 G01N 33/68 A61P 19/08 A61P 19/10 (2006.01) A61P 19/08 (2006.01) (2006.01) (22) Date of filing: 29.12.2004 A61P 19/10 (84) Designated Contracting States: • Tomme, Peter Herwig Maria AT BE BG CH CY CZ DE DK EE ES FI FR GB GR 9000 Gent (BE) HU IE IS IT LI LT LU MC NL PL PT RO SE SI SK TR • Brown, Robin John 9800 Bachte-Maria-Leerne (BE) (30) Priority: 29.12.2003 PCT/EP03/14994 (74) Representative: van Kooij, Adriaan et al (62) Document number(s) of the earlier application(s) in Arnold & Siedsma accordance with Art. 76 EPC: Sweelickplein 1 04804467.1 / 1 709 173 2517 GK Den Haag (NL) (71) Applicant: Galapagos N.V. Remarks: 2800 Mechelen (BE) This application was filed on 30-08-2010 as a divisional application to the application mentioned (72) Inventors: under INID code 62. • Van Rompaye, Luc Juliaan Corina 3140 Keerbergen (BE) (54) Methods for inducing differentiation of undifferentiated mammalian cells into osteoblasts (57) The present invention provides methods for in- use thereof as a medicament for the treatment of a dis- ducing differentiation of undifferentiated mammalian ease involving a systemic or local decrease in mean bone cells into osteoblasts, and methods for identifying a com- density. -
Mrna Expression in Human Leiomyoma and Eker Rats As Measured by Microarray Analysis
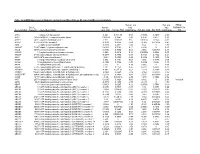
Table 3S: mRNA Expression in Human Leiomyoma and Eker Rats as Measured by Microarray Analysis Human_avg Rat_avg_ PENG_ Entrez. Human_ log2_ log2_ RAPAMYCIN Gene.Symbol Gene.ID Gene Description avg_tstat Human_FDR foldChange Rat_avg_tstat Rat_FDR foldChange _DN A1BG 1 alpha-1-B glycoprotein 4.982 9.52E-05 0.68 -0.8346 0.4639 -0.38 A1CF 29974 APOBEC1 complementation factor -0.08024 0.9541 -0.02 0.9141 0.421 0.10 A2BP1 54715 ataxin 2-binding protein 1 2.811 0.01093 0.65 0.07114 0.954 -0.01 A2LD1 87769 AIG2-like domain 1 -0.3033 0.8056 -0.09 -3.365 0.005704 -0.42 A2M 2 alpha-2-macroglobulin -0.8113 0.4691 -0.03 6.02 0 1.75 A4GALT 53947 alpha 1,4-galactosyltransferase 0.4383 0.7128 0.11 6.304 0 2.30 AACS 65985 acetoacetyl-CoA synthetase 0.3595 0.7664 0.03 3.534 0.00388 0.38 AADAC 13 arylacetamide deacetylase (esterase) 0.569 0.6216 0.16 0.005588 0.9968 0.00 AADAT 51166 aminoadipate aminotransferase -0.9577 0.3876 -0.11 0.8123 0.4752 0.24 AAK1 22848 AP2 associated kinase 1 -1.261 0.2505 -0.25 0.8232 0.4689 0.12 AAMP 14 angio-associated, migratory cell protein 0.873 0.4351 0.07 1.656 0.1476 0.06 AANAT 15 arylalkylamine N-acetyltransferase -0.3998 0.7394 -0.08 0.8486 0.456 0.18 AARS 16 alanyl-tRNA synthetase 5.517 0 0.34 8.616 0 0.69 AARS2 57505 alanyl-tRNA synthetase 2, mitochondrial (putative) 1.701 0.1158 0.35 0.5011 0.6622 0.07 AARSD1 80755 alanyl-tRNA synthetase domain containing 1 4.403 9.52E-05 0.52 1.279 0.2609 0.13 AASDH 132949 aminoadipate-semialdehyde dehydrogenase -0.8921 0.4247 -0.12 -2.564 0.02993 -0.32 AASDHPPT 60496 aminoadipate-semialdehyde -

Mammalian Metallopeptidase Inhibition at the Defense Barrier of Ascaris Parasite
Mammalian metallopeptidase inhibition at the defense barrier of Ascaris parasite Laura Sanglasa, Francesc X. Avilesa, Robert Huberb,c,d,1, F. Xavier Gomis-Ru¨ the,1, and Joan L. Arolasa,e,1 aInstitut de Biotecnologia i de Biomedicina and Departament de Bioquímica i Biologia Molecular, Facultat de Cie`ncies, Universitat Auto`noma de Barcelona, E-08193 Bellaterra, Barcelona, Spain; bMax-Planck-Institut fu¨r Biochemie, Am Klopferspitz 18a, D-82152 Martinsried, Germany; cSchool of Biosciences, Cardiff University, Cardiff CF10 3US, United Kingdom; dCentre for Medical Biotechnology, Fachbereich Biology and Geography, University Duisburg-Essen, Universita¨tsstrasse, D-45117 Essen, Germany; and eDepartment of Structural Biology, Proteolysis Laboratory, Molecular Biology Institute of Barcelona, Consejo Superior de Investigaciones Cientificas, Barcelona Science Park, Helix Building, c/Baldiri Reixac 15-21, E-08028 Barcelona, Spain Contributed by Robert Huber, December 12, 2008 (sent for review November 17, 2008) Roundworms of the genus Ascaris are common parasites of the catalyze the hydrolysis of C-terminal amino acids from proteins human gastrointestinal tract. A battery of selective inhibitors and peptides. They perform a large variety of physiologically protects them from host enzymes and the immune system. Here, a relevant functions in organisms of different phyla (17). These metallocarboxypeptidase (MCP) inhibitor, ACI, was identified in enzymes have been grouped into the funnelin tribe of proteases protein extracts from Ascaris by intensity-fading MALDI-TOF mass and are subdivided into A/B- and N/E-type MCPs (18). Human spectrometry. The 67-residue amino acid sequence of ACI showed A/B-type funnelins include the digestive enzymes CPA1, CPA2, no significant homology with any known protein.