Hearing Research 310 (2014) 27E35
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

United States Patent (19) 11 Patent Number: 5,993,812 Tsoukas Et Al
USOO5993812A United States Patent (19) 11 Patent Number: 5,993,812 TSOukas et al. (45) Date of Patent: Nov.30, 1999 54 METHOD OF DELAYING THE Brunkhorst et al., Infection 18:28-32, 1990. PROGRESSION OF AN INFECTION WITH Coyle et al., Changes in the Lymphocyte Count and Lym THE HUMAN IMMUNODEFICIENCY VIRUS phocyte Subsets After Splenectomy in Human Immunode ficiency Virus Infection, Letters and Correspondence, pp. 75 Inventors: Christos M. Tsoukas, Montreal; Barry 144-146. Michael Woloski, Winnipeg, both of DeSimone et al., Immunopharma. and Immunotoxic., Canada 13:447-458, 1991. Gringeri et al., British Journal of Haemotology, 80:337-340, 73 Assignee: Cangene Corporation, Winnipeg, 1992. Canada Gingör et al., Eur. J. Pediatr., 152:650–654, 1993. Mofenson and Moye, Pediatric Research, 33:80-S89, 1993. 21 Appl. No.: 08/835,400 Mofenson et al., Journal of Acquired Immune Deficiency 22 Filed: Apr. 7, 1997 Syndrome, 6:1103-1113, 1993. Schrappe-Bächer et al., Vox Sang, 59:3-14, 1990. Related U.S. Application Data Shearer et al., Ann. N.Y. Acad. Sci., pp. 35-51. Wagner et al., Arch. of Disease in Childhood., 63 Continuation-in-part of application No. 08/713,765, Sep. 13, 67:1267-1271, 1992. 1996, abandoned. Watson, et al., “Recombinant DNA”, Scientific American 60 Provisional application No. 60/003,756, Sep. 14, 1995. Books, Chapter 25. 51) Int. Cl. ............................ A61K 39/395; CO7K 1/00 Okesenhendeler, et al., “Anti-RH immunoglobulin therapy 52 U.S. Cl. ................... 424/130.1; 530/350, 530/388.7; for human immunodeficiency virus-related immune throm 424/142.1; 424/141.1; 424/153.1 bocytopenic purpura’, Blood, 71 (5) 1499-502. -

VIDEX (Didanosine) Chewable/Dispersible Buffered Tablets
Rx only VIDEXâ (didanosine) â VIDEX (didanosine) Chewable/Dispersible Buffered Tablets â VIDEX (didanosine) Buffered Powder for Oral Solution â VIDEX (didanosine) Pediatric Powder for Oral Solution (Patient Information Leaflet Included) WARNING FATAL AND NONFATAL PANCREATITIS HAVE OCCURRED DURING THERAPY WITH VIDEX USED ALONE OR IN COMBINATION REGIMENS IN BOTH TREATMENT-NAIVE AND TREATMENT-EXPERIENCED PATIENTS, REGARDLESS OF DEGREE OF IMMUNOSUPPRESSION. VIDEX SHOULD BE SUSPENDED IN PATIENTS WITH SUSPECTED PANCREATITIS AND DISCONTINUED IN PATIENTS WITH CONFIRMED PANCREATITIS (SEE WARNINGS). LACTIC ACIDOSIS AND SEVERE HEPATOMEGALY WITH STEATOSIS, INCLUDING FATAL CASES, HAVE BEEN REPORTED WITH THE USE OF NUCLEOSIDE ANALOGUES ALONE OR IN COMBINATION, INCLUDING DIDANOSINE AND OTHER ANTIRETROVIRALS. FATAL LACTIC ACIDOSIS HAS BEEN REPORTED IN PREGNANT WOMEN WHO RECEIVED THE COMBINATION OF DIDANOSINE AND STAVUDINE WITH OTHER ANTIRETROVIRAL AGENTS. THE COMBINATION OF DIDANOSINE AND STAVUDINE SHOULD BE USED WITH CAUTION DURING PREGNANCY AND IS RECOMMENDED ONLY IF THE POTENTIAL BENEFIT CLEARLY OUTWEIGHS THE POTENTIAL RISK. (SEE WARNINGS AND PRECAUTIONS: PREGNANCY.) Page 4 of 39 DESCRIPTION â VIDEX (didanosine) is a brand name for didanosine (ddI), a synthetic purine nucleoside analogue active against the Human Immunodeficiency Virus (HIV). VIDEX Chewable/Dispersible Buffered Tablets are available for oral administration in strengths of 25, 50, 100, 150, and 200 mg of didanosine. Each tablet is buffered with calcium carbonate and magnesium hydroxide. VIDEX tablets also contain aspartame, sorbitol, microcrystalline cellulose, polyplasdone, mandarin-orange flavor, and magnesium stearate. VIDEX Buffered Powder for Oral Solution is supplied for oral administration in single- dose packets containing 100, 167, or 250 mg of didanosine. Packets of each product strength also contain a citrate-phosphate buffer (composed of dibasic sodium phosphate, sodium citrate, and citric acid) and sucrose. -
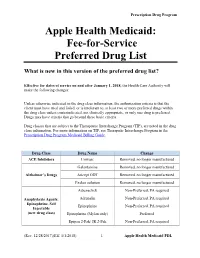
Fee-For-Service Preferred Drug List
Prescription Drug Program Apple Health Medicaid: Fee-for-Service Preferred Drug List What is new in this version of the preferred drug list? Effective for dates of service on and after January 1, 2018, the Health Care Authority will make the following changes: Unless otherwise indicated in the drug class information, the authorization criteria is that the client must have tried and failed, or is intolerant to, at least two or more preferred drugs within the drug class unless contraindicated, not clinically appropriate, or only one drug is preferred. Drugs may have criteria that go beyond these basic criteria. Drug classes that are subject to the Therapeutic Interchange Program (TIP), are noted in the drug class information. For more information on TIP, see Theraputic Interchange Program in the Prescription Drug Program Medicaid Billing Guide. Drug Class Drug Name Change ACE Inhibitors Univasc Removed, no longer manufactured Galantamine Removed, no longer manufactured Alzheimer’s Drugs Aricept ODT Removed, no longer manufactured Exelon solution Removed, no longer manufactured Adrenaclick Non-Preferred, PA required Anaphylaxis Agents: Adrenalin Non-Preferred, PA required Epinephrine, Self Epinephrine Non-Preferred, PA required Injectable (new drug class) Epinephrine (Mylan only) Preferred Epipen 2-Pak/ JR 2-Pak Non-Preferred, PA required (Rev. 12/28/2017)(Eff. 1/1/2018) – 1 – Apple Health Medicaid PDL Prescription Drug Program Renamed drug class “Anticoagulants: Anticoagulants Entire class Factor XA and Thrombin Inhibitors.” Anticoagulants: -

Non-Anntoated Product Monograph
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PrTRIUMEQ dolutegravir, abacavir, and lamivudine tablets 50 mg dolutegravir (as dolutegravir sodium), 600 mg abacavir (as abacavir sulfate) and 300 mg lamivudine Antiretroviral Agent ViiV Healthcare ULC 245, boulevard Armand-Frappier Laval, Quebec H7V 4A7 Date of Revision: January 31, 2020 Submission Control No: 233245 © 2020 ViiV Healthcare group of companies or its licensor Trademarks are owned by or licensed to the ViiV Healthcare group of companies Page 1 of 61 TABLE OF CONTENTS PAGE PART I: HEALTH PROFESSIONAL INFORMATION ........................................................ 3 SUMMARY PRODUCT INFORMATION ................................................................... 3 INDICATIONS AND CLINICAL USE ........................................................................ 3 CONTRAINDICATIONS ........................................................................................... 4 WARNINGS AND PRECAUTIONS............................................................................ 4 ADVERSE REACTIONS.......................................................................................... 11 DRUG INTERACTIONS .......................................................................................... 19 DOSAGE AND ADMINISTRATION ........................................................................ 24 OVERDOSAGE....................................................................................................... 26 ACTION AND CLINICAL PHARMACOLOGY........................................................ -
Clinician's Reference Guide to Curanderismo
Clinician’s Reference Guide to Curanderismo Reference Guide Focus Scope of reference guide – to provide a basic introduc‐ tion to “curanderismo” to enhance the provider’s ability to confidently initiate conversations with patients who practice this form of traditional healing/complementary and alternative medicine (TCAM). This reference guide will 1) demystify common myths about curanderismo by clarifying what it is/is not, 2) review benefits of knowing about curanderismo to improve communication be‐ tween patient and provider; and 3) highlight some use‐ ful terminology for use with patients who practice forms of curanderismo. Goal – To improve health outcomes among Latino/as living with HIV disease, the health care provider and patient/client will collaborate on a more culturally ap‐ propriate treatment plan through a better understand‐ ing of the patient’s 1) core health beliefs and practices, 2) reasons Latino/a patients may use curanderismo and highlights of risks and 3) how the practices may inter‐ fere with conventional medical practices. Target audience – health care providers including: physi‐ cians, physician assistants, advanced practice nurses, nurses, pharmacists, oral health professionals as well as substance abuse counselors and mental health counsel‐ ors. TABLE OF CONTENTS: Introduction What Is and What Isn't Curanderismo Benefits to Knowing about Curanderismo Useful Terminology Commonly Used Herbs, Spices, & Other Items Why It Is Important to ask Introduction According to the World Health Organization, traditional medicine continues to be used in Latin America, Africa, and Asia to meet primary health care needs. In many developed countries, up to 80% of the population have used some form of traditional healing, complementary or alternative medi‐ cine ‐ TCAM (e.g. -
![1-Acetyl-17-{2-Hydroxy-3-[4-(2-Methoxyphenyl)Piperazin-1- Yl]Propyl}-17-Azapentacyclo[6.6.5.0 2,7 .0 9,14 .0 15,19 ]Nonadeca- 2,4,6,9,11,13-Hexaene-16,18-Dione](https://docslib.b-cdn.net/cover/2983/1-acetyl-17-2-hydroxy-3-4-2-methoxyphenyl-piperazin-1-yl-propyl-17-azapentacyclo-6-6-5-0-2-7-0-9-14-0-15-19-nonadeca-2-4-6-9-11-13-hexaene-16-18-dione-1512983.webp)
1-Acetyl-17-{2-Hydroxy-3-[4-(2-Methoxyphenyl)Piperazin-1- Yl]Propyl}-17-Azapentacyclo[6.6.5.0 2,7 .0 9,14 .0 15,19 ]Nonadeca- 2,4,6,9,11,13-Hexaene-16,18-Dione
Molbank 2010 , M697; doi:10.3390/M697 OPEN ACCESS molbank ISSN 1422-8599 www.mdpi.com/journal/molbank Short Note 1-Acetyl-17-{2-hydroxy-3-[4-(2-methoxyphenyl)piperazin-1- yl]propyl}-17-azapentacyclo[6.6.5.0 2,7 .0 9,14 .0 15,19 ]nonadeca- 2,4,6,9,11,13-hexaene-16,18-dione Magdalena Pakosi ńska-Parys *, Jerzy Kossakowski and Marta Struga Chair and Department of Medical Chemistry, 1 st Faculty of Medicine, Medical University of Warsaw, 3 Oczki Street, 02-007 Warsaw, Poland * Author to whom correspondence should be addressed; E-Mail: [email protected] Received: 5 August 2010 / Accepted: 14 September 2010 / Published: 17 September 2010 Abstract: The title compound was synthesized by condensation of an oxiran imide derivative with an appropriate amine and its IR, 1H NMR, 13 C NMR and mass spectroscopic data are reported. The synthesized compound was evaluated for its cytotoxicity and anti-HIV-1 activity in MT-4 cells. Keywords: 1-acetyl-17-{2-hydroxy-3-[4-(2-methoxyphenyl)piperazin-1-yl]propyl}-17- azapentacyclo[6.6.5.0 2,7 .0 9,14 .0 15,19 ]nonadeca-2,4,6,9,11,13-hexaene-16,18-dione; cytotoxicity Introduction Currently available drugs for the treatment of HIV infections are based on combination of two types of anti-HIV-1 agents: nucleoside reverse transcriptase inhibitors (RTIs) and protease inhibitors [1]. The RTIs can be divided into nucleoside (NI) and non-nucleoside RT inhibitors (NNRTI). Several non-nucleoside inhibitors have been described, including nevirapine, thiobenzimidazolone (TIBO) derivatives, pyridinone derivatives and the bis(heteroaryl)piperazines (BHAPs), such as delavirdine and atevirdine [2]. -
Abacavir Sulfate and Lamivudine Tablets
P1501370 Rx only (60 mg/30 mg) Abacavir Sulfate and Lamivudine Tablets * Data presented as mean ± standard deviation except where noted. suspected hypersensitivity were collected on a detailed data collection module. The frequencies of symptoms Approximate range. are shown in Figure 1. Symptoms usually appeared within the first 6 weeks of treatment with abacavir, although the reaction may occur at any time during therapy. Median time to onset was 9 days; 89% appeared within the Abacavir Sulfate and Lamivudine Tablets Effect of Food on Absorption of Abacavir Sulfate and Lamivudine Tablets first 6 weeks; 95% of patients reported symptoms from 2 or more of the 5 groups listed above. Abacavir Sulfate and Lamivudine Tables may be administered with or without food. Administration with a high- Figure 1: Hypersensitivity-Related Symptoms Reported with ³10% Frequency in Clinical Trials (n = 206 (60 mg/30 mg) fat meal in a single-dose bioavailability study resulted in no change in AUC last, AUC , and Cmax for lamivudine. Patients) Rx only Food did not alter the extent of systemic exposure to abacavir (AUC ), but the rate of absorption (Cmax) was decreased approximately 24% compared to fasted conditions (n = 25). These results are similar to those from 70 WARNINGS previous studies of the effect of food on abacavir and lamivudine tablets administered separately. Abacavir Sulfate and Lamivudine Tablets contain 2 nucleoside analogues (abacavir sulfate and lamivudine) Special Populations 60 and are intended only for patients whose regimen would otherwise include these 2 components. Renal Impairment Hypersensitivity Reactions: Serious and sometimes fatal hypersensitivity reactions have been associated Abacavir Sulfate and Lamivudine: The pharmacokinetic properties of abacavir sulfate have not been determined 50 with abacavir sulfate, a component of Abacavir Sulfate and Lamivudine Tablets. -

Managing Side Effects of HIV Medications | 1 Managing Side Effects of HIV Medications | 2 Your Doctor Can Also Help You Prepare for Any Side Effects
Managing Side Eects of HIV MEDICATIONS Table of Contents What are side effects?..........................................................................................1 Side effects of different classes of HIV drugs ....................................................9 Why do I need to know about side effects of HIV medications? ......................2 Protease inhibitors ..................................................................................................................9 Fat problems (lipodystrophy) ..............................................................................................9 What questions should I ask when my doctor first prescribes an HIV medication? .............................................................................................2 Metabolic problems ................................................................................................................9 Make sure you understand what the medication does and the best way Heart disease, heart attacks, stroke ...................................................................................9 to take it ......................................................................................................................................2 Diabetes ................................................................................................................................... 10 Your doctor can also help you prepare for any side effects .....................................3 Nucleoside Reverse Transcriptase Inhibitors (NRTIs) ............................................. -

NNRTI) Resistance Mutations
Nonnucleoside RT inhibitor (NNRTI) resistance mutations The NNRTIs bind to a hydrophobic pocket in the RT located between the β6-β10-β9 and β 2-β13-β14 sheets of the p66 subunit (Hsiou et al., 2001) (Figure 7). A small portion of the pocket is also formed by residues from the p51 subunit. The NNRTI-binding pocket is close to but not contiguous with, the active site. The NNRTIs inhibit HIV-1 replication allosterically by displacing the catalytic aspartate residues relative to the polymerase-binding site (Kohlstaedt et al., 1992; Esnouf et al., 1995; Spence et al., 1995). The hydrophobic NNRTI-binding pocket is less well conserved than the dNTP-binding site. Indeed, HIV-1 Group O and HIV-2 (Shih et al., 1991; Hizi et al., 1993; Yang et al., 1996; Descamps et al., 1997) are intrinsically resistant to most NNRTIs. A single mutation in the NNRTI-binding pocket may result in high-level resistance to one or more of the NNRTIs. Resistance usually emerges rapidly when NNRTIs are administered as monotherapy or in the presence of incomplete virus suppression, suggesting that resistance is caused by the selection of a pre-existing population of mutant viruses within an individual (Wei et al., 1995; Havlir et al., 1996; Jackson et al., 2000; Conway et al., 2001). Several studies have shown that a single dose of nevirapine used to prevent mother-to-child HIV transmission can select for NNRTI-resistant mutants that are detectable for at least two months (Jackson et al., 2000; Cunningham et al., 2002; Kantor et al., 2003). -

Delavirdine (Rescriptor)
Delavirdine FACT (Rescriptor) SHEET Published 2014 Summary Delavirdine is a type of anti-HIV drug called a non-nucleoside reverse transcriptase inhibitor. The most common side effect CONTACT US is a skin rash that usually goes away on its own. Delavirdine is taken three times a day, with or without food. by telephone 1-800-263-1638 416-203-7122 What is delavirdine? by fax Delavirdine, sold under the brand name Rescriptor, is a type of antiretroviral 416-203-8284 drug called a non-nucleoside reverse transcriptase inhibitor. by e-mail How does delavirdine work? [email protected] To explain how delavirdine works, we need to first tell you some information about HIV. When HIV infects a cell, it takes control of that cell. HIV then forces by mail the cell to make many more copies of the virus. To make these copies, the cell 555 Richmond Street West uses proteins called enzymes. When the activity of these enzymes is reduced Suite 505, Box 1104 the production of HIV slows. Toronto ON M5V 3B1 Delavirdine belongs to a group of drugs called non-nucleoside reverse transcriptase inhibitors (NNRTIs or “non-nukes”). The enzyme reverse transcriptase is used by HIV-infected cells to make new viruses. Since delavirdine inhibits, or reduces the activity of this enzyme, this drug causes HIV-infected cells to produce fewer viruses. How do people with HIV use delavirdine? Delavirdine is rarely used in Canada today. Delavirdine is used in combination with other anti-HIV drugs. For more information on combinations of anti-HIV drugs, see CATIE’s Your Guide to HIV Treatment. -

Drugs That Fight
A reference guide for prescription HIV medications Several different kinds of antiretroviral drugs are currently used to treat HIV infection. • These medicines do not cure HIV infection or AIDS • These medicines do not eliminate the risk of passing HIV to others • Treatment of HIV infection requires a combination of HIV medicines • Not all medicines are right for all people, and treatments may be different for each person; talk with your doctor or other health care provider if you have questions about your treatment NOTE: Many of these medications pictured may also be available in a generic form, but the generic forms are not pictured here. Tablets and capsules pictured are not actual size. A program of the National Institutes of Health NIH...Turning Discovery into Health® Published by The U.S. Department of Health and Human Services Nucleoside Reverse Non-Nucleoside Reverse Transcriptase Inhibitors (NRTIs) Transcriptase Inhibitors (NNRTIs) NRTIs block reverse transcriptase, an enzyme NNRTIs bind to and later reverse transcriptase, an HIV needs to make copies of itself. enzyme HIV needs to make copies of itself. Abacavir (ABC) Stavudine (d4T) Delavirdine trade name: trade name: trade name: Ziagen Zerit Rescriptor 200 mg Rescriptor tablet 15 mg Zerit capsule 300 mg Ziagen tablet 100 mg Rescriptor tablet 20 mg Zerit capsule Efavirenz (EFV) 30 mg Zerit capsule trade name: Sustiva 50 mg Sustiva capsule 20 mg/mL Ziagen oral solution 40 mg Zerit capsule 1 mg/mL Zerit oral solution 600 mg Sustiva tablet 200 mg Sustiva capsule Didanosine (ddl) -

Kentucky Aids Drug Assistance Program (Kadap)
KENTUCKY AIDS DRUG ASSISTANCE PROGRAM (KADAP) (Revised July 3, 2019) ANTIRETROVIRAL (ARV) THERAPY OPPORTUNISTIC INFECTION (OI) THERAPY Class Generic Name(s) Trade Name Abbreviation(s) Generic Name(s) Trade Name(s) CD4 Post-Attachment HIV-1 Inhibitor acyclovir Zovirax ibalizumab-uiyk for injection Trogarzo IBA atovaquone Mepron Entry Inhibitor azithromycin Zithromax maraviroc Selzentry MVC ciprofloxacin Cipro, Ciloxan, Centraxal Fusion Inhibitor clarithromycin Biaxin enfuvirtide Fuzeon T20 clotrimazole Canesten, Lotrimin Integrase Inhibitor dapsone Aczone dolutegravir Tivcay DTG Alodox, Atridox, Doryx, Monodox, Morgidox, Ocudox, doxycycline raltegravir Isentress RAL Oracea, Periostat, VibraTabs Multi-Class ARV Agent ethambutol Myambutol, Servambutol abacavir / dolutegravir / lamivudine Triumeq or Trii ABC + DTG + 3TC fluconazole● Diflucan bictegravir / emtricitabine / tenofovir AF Biktarvy BIC + FTC + TAF isoniazid - darunavir / cobicistat / emtrictabine / itraconozole Sporanox Symtuza DRV + COBI + FTC + TAF tenofovir AF ketoconzaole▲ Extina, Nizoral, Xolegel dolutegravir / rilpivirine Juluca DTG + RPV leucovorin - efavirenz / emtrictabine / tenofovir DF Atripla EFV + FTC + TDF nystatin NyStop elvitegravir / cobicistat / emtricitabine / paramomycin - Genvoya EVG + COBI + FTC + TAF tenofovir AF primaquine - elvitegravir / cobicistat / emtricitibine / pyrimethamine Daraprim Stribild EVG + COBI + FTC + TDF tenofovir DF rifabutin Mycobutin emtricitabine / rilpivirine / tenofovir AF Odefsey FTC + RPV + TAF rifampin Rifadin, Rimactane emtricitabine