NNRTI) Resistance Mutations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

<I>Efavirenz</I>, New Therapeutic Agents for AIDS
CONFERENCE REPORTS 295 CHIMIA 1999. 53. NO.6 CONFERENCE REPORTS Chimia 53 (1999) 295-304 © Neue Schweizerische Chemische Gesellschaft ISSN 0009-4293 Second Swiss/German Meeting on Medicinal Chemistry Fruhjahrsversammlung 1999 der Neuen Schweizerischen Chemischen Gesellschaft (NSCG) 22./23. Marz 1999, Basel Vier Mini-Symposia uber Virologie, Multidrug Resistance, Immunologie und Gene Therapie Organisiert von der Sektion Medizinische Ghemie der NSGG, der Fachgruppe fUr Medizinische Chemie der GDGh und der Basler Chemischen Gesellschatt mit Unterstutzung der Pharmazeutischen Industrie. Report by the Research Team of G. Folkers' 'Correspondence: Prof. Dr. G. Folkers Department of Pharmacy Winterthurerstrasse 190 CH-8057Zi.irich E-Mail: [email protected] Discovery of Indinavir and Efavirenz, New Therapeutic Agents for AIDS Terry A. Lyle, Merck Research Laboratories, West Point, PA, USA For the treatment of HIV infection, two enzymes are of major interest: The HIV-l Protease (PR) and the Reverse- Tran- scriptase (RT). The HIV -Protease, an aspartic-acid pro- tease active as a dimer, is responsible for H 0 the cleavage of polypeptides assembled at o N~' the cell membrane. The inhibition of the Y I( ; N 1\ 0 = H protease-mediated cleavage of the viral "0 o o o precursor polyproteins results in the pro- duction of noninfectious progeny viral par- ticles. The development of lndinavir start- ed with screening a collection of renin inhibitors. A seven-amino-acid analog 1 1 which contains the hydroxyethylene tran- CONFERENCE REPORTS 296 CHIMIA 1999, 53. No.6 prevents the spread of the virus. Different nucleoside inhibitors like AZT, ddI, ddC, d4T and 3TC are already known, but new QH non-nucleoside inhibitors (NNRTI) are U'O developed to decrease the cytotoxicity and N : to improve the selectivity of the viral polymerases vs. -

Characterization of Resistance to a Potent D-Peptide HIV Entry Inhibitor
Smith et al. Retrovirology (2019) 16:28 https://doi.org/10.1186/s12977-019-0489-7 Retrovirology RESEARCH Open Access Characterization of resistance to a potent D-peptide HIV entry inhibitor Amanda R. Smith1†, Matthew T. Weinstock1†, Amanda E. Siglin2, Frank G. Whitby1, J. Nicholas Francis1, Christopher P. Hill1, Debra M. Eckert1, Michael J. Root2 and Michael S. Kay1* Abstract Background: PIE12-trimer is a highly potent D-peptide HIV-1 entry inhibitor that broadly targets group M isolates. It specifcally binds the three identical conserved hydrophobic pockets at the base of the gp41 N-trimer with sub- femtomolar afnity. This extremely high afnity for the transiently exposed gp41 trimer provides a reserve of binding energy (resistance capacitor) to prevent the viral resistance pathway of stepwise accumulation of modest afnity- disrupting mutations. Such modest mutations would not afect PIE12-trimer potency and therefore not confer a selective advantage. Viral passaging in the presence of escalating PIE12-trimer concentrations ultimately selected for PIE12-trimer resistant populations, but required an extremely extended timeframe (> 1 year) in comparison to other entry inhibitors. Eventually, HIV developed resistance to PIE12-trimer by mutating Q577 in the gp41 pocket. Results: Using deep sequence analysis, we identifed three mutations at Q577 (R, N and K) in our two PIE12-trimer resistant pools. Each point mutant is capable of conferring the majority of PIE12-trimer resistance seen in the poly- clonal pools. Surface plasmon resonance studies demonstrated substantial afnity loss between PIE12-trimer and the Q577R-mutated gp41 pocket. A high-resolution X-ray crystal structure of PIE12 bound to the Q577R pocket revealed the loss of two hydrogen bonds, the repositioning of neighboring residues, and a small decrease in buried surface area. -

2D6 Substrates 2D6 Inhibitors 2D6 Inducers
Physician Guidelines: Drugs Metabolized by Cytochrome P450’s 1 2D6 Substrates Acetaminophen Captopril Dextroamphetamine Fluphenazine Methoxyphenamine Paroxetine Tacrine Ajmaline Carteolol Dextromethorphan Fluvoxamine Metoclopramide Perhexiline Tamoxifen Alprenolol Carvedilol Diazinon Galantamine Metoprolol Perphenazine Tamsulosin Amiflamine Cevimeline Dihydrocodeine Guanoxan Mexiletine Phenacetin Thioridazine Amitriptyline Chloropromazine Diltiazem Haloperidol Mianserin Phenformin Timolol Amphetamine Chlorpheniramine Diprafenone Hydrocodone Minaprine Procainamide Tolterodine Amprenavir Chlorpyrifos Dolasetron Ibogaine Mirtazapine Promethazine Tradodone Aprindine Cinnarizine Donepezil Iloperidone Nefazodone Propafenone Tramadol Aripiprazole Citalopram Doxepin Imipramine Nifedipine Propranolol Trimipramine Atomoxetine Clomipramine Encainide Indoramin Nisoldipine Quanoxan Tropisetron Benztropine Clozapine Ethylmorphine Lidocaine Norcodeine Quetiapine Venlafaxine Bisoprolol Codeine Ezlopitant Loratidine Nortriptyline Ranitidine Verapamil Brofaramine Debrisoquine Flecainide Maprotline olanzapine Remoxipride Zotepine Bufuralol Delavirdine Flunarizine Mequitazine Ondansetron Risperidone Zuclopenthixol Bunitrolol Desipramine Fluoxetine Methadone Oxycodone Sertraline Butylamphetamine Dexfenfluramine Fluperlapine Methamphetamine Parathion Sparteine 2D6 Inhibitors Ajmaline Chlorpromazine Diphenhydramine Indinavir Mibefradil Pimozide Terfenadine Amiodarone Cimetidine Doxorubicin Lasoprazole Moclobemide Quinidine Thioridazine Amitriptyline Cisapride -

United States Patent (19) 11 Patent Number: 5,993,812 Tsoukas Et Al
USOO5993812A United States Patent (19) 11 Patent Number: 5,993,812 TSOukas et al. (45) Date of Patent: Nov.30, 1999 54 METHOD OF DELAYING THE Brunkhorst et al., Infection 18:28-32, 1990. PROGRESSION OF AN INFECTION WITH Coyle et al., Changes in the Lymphocyte Count and Lym THE HUMAN IMMUNODEFICIENCY VIRUS phocyte Subsets After Splenectomy in Human Immunode ficiency Virus Infection, Letters and Correspondence, pp. 75 Inventors: Christos M. Tsoukas, Montreal; Barry 144-146. Michael Woloski, Winnipeg, both of DeSimone et al., Immunopharma. and Immunotoxic., Canada 13:447-458, 1991. Gringeri et al., British Journal of Haemotology, 80:337-340, 73 Assignee: Cangene Corporation, Winnipeg, 1992. Canada Gingör et al., Eur. J. Pediatr., 152:650–654, 1993. Mofenson and Moye, Pediatric Research, 33:80-S89, 1993. 21 Appl. No.: 08/835,400 Mofenson et al., Journal of Acquired Immune Deficiency 22 Filed: Apr. 7, 1997 Syndrome, 6:1103-1113, 1993. Schrappe-Bächer et al., Vox Sang, 59:3-14, 1990. Related U.S. Application Data Shearer et al., Ann. N.Y. Acad. Sci., pp. 35-51. Wagner et al., Arch. of Disease in Childhood., 63 Continuation-in-part of application No. 08/713,765, Sep. 13, 67:1267-1271, 1992. 1996, abandoned. Watson, et al., “Recombinant DNA”, Scientific American 60 Provisional application No. 60/003,756, Sep. 14, 1995. Books, Chapter 25. 51) Int. Cl. ............................ A61K 39/395; CO7K 1/00 Okesenhendeler, et al., “Anti-RH immunoglobulin therapy 52 U.S. Cl. ................... 424/130.1; 530/350, 530/388.7; for human immunodeficiency virus-related immune throm 424/142.1; 424/141.1; 424/153.1 bocytopenic purpura’, Blood, 71 (5) 1499-502. -

VIDEX (Didanosine) Chewable/Dispersible Buffered Tablets
Rx only VIDEXâ (didanosine) â VIDEX (didanosine) Chewable/Dispersible Buffered Tablets â VIDEX (didanosine) Buffered Powder for Oral Solution â VIDEX (didanosine) Pediatric Powder for Oral Solution (Patient Information Leaflet Included) WARNING FATAL AND NONFATAL PANCREATITIS HAVE OCCURRED DURING THERAPY WITH VIDEX USED ALONE OR IN COMBINATION REGIMENS IN BOTH TREATMENT-NAIVE AND TREATMENT-EXPERIENCED PATIENTS, REGARDLESS OF DEGREE OF IMMUNOSUPPRESSION. VIDEX SHOULD BE SUSPENDED IN PATIENTS WITH SUSPECTED PANCREATITIS AND DISCONTINUED IN PATIENTS WITH CONFIRMED PANCREATITIS (SEE WARNINGS). LACTIC ACIDOSIS AND SEVERE HEPATOMEGALY WITH STEATOSIS, INCLUDING FATAL CASES, HAVE BEEN REPORTED WITH THE USE OF NUCLEOSIDE ANALOGUES ALONE OR IN COMBINATION, INCLUDING DIDANOSINE AND OTHER ANTIRETROVIRALS. FATAL LACTIC ACIDOSIS HAS BEEN REPORTED IN PREGNANT WOMEN WHO RECEIVED THE COMBINATION OF DIDANOSINE AND STAVUDINE WITH OTHER ANTIRETROVIRAL AGENTS. THE COMBINATION OF DIDANOSINE AND STAVUDINE SHOULD BE USED WITH CAUTION DURING PREGNANCY AND IS RECOMMENDED ONLY IF THE POTENTIAL BENEFIT CLEARLY OUTWEIGHS THE POTENTIAL RISK. (SEE WARNINGS AND PRECAUTIONS: PREGNANCY.) Page 4 of 39 DESCRIPTION â VIDEX (didanosine) is a brand name for didanosine (ddI), a synthetic purine nucleoside analogue active against the Human Immunodeficiency Virus (HIV). VIDEX Chewable/Dispersible Buffered Tablets are available for oral administration in strengths of 25, 50, 100, 150, and 200 mg of didanosine. Each tablet is buffered with calcium carbonate and magnesium hydroxide. VIDEX tablets also contain aspartame, sorbitol, microcrystalline cellulose, polyplasdone, mandarin-orange flavor, and magnesium stearate. VIDEX Buffered Powder for Oral Solution is supplied for oral administration in single- dose packets containing 100, 167, or 250 mg of didanosine. Packets of each product strength also contain a citrate-phosphate buffer (composed of dibasic sodium phosphate, sodium citrate, and citric acid) and sucrose. -

Sustiva, INN-Efavirenz
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT SUSTIVA 50 mg hard capsules SUSTIVA 100 mg hard capsules SUSTIVA 200 mg hard capsules 2. QUALITATIVE AND QUANTITATIVE COMPOSITION SUSTIVA 50 mg hard capsules Each hard capsule contains 50 mg of efavirenz. Excipient with known effect Each hard capsule contains 28.5 mg of lactose (as monohydrate). SUSTIVA 100 mg hard capsules Each hard capsule contains 100 mg of efavirenz. Excipient with known effect Each hard capsule contains 57.0 mg of lactose (as monohydrate). SUSTIVA 200 mg hard capsules Each hard capsule contains 200 mg of efavirenz. Excipient with known effect Each hard capsule contains 114.0 mg of lactose (as monohydrate). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Hard capsule SUSTIVA 50 mg hard capsules Dark yellow and white, printed with "SUSTIVA" on the dark yellow cap and "50 mg" on the white body. SUSTIVA 100 mg hard capsules White, printed with "SUSTIVA" on the body and "100 mg" on the cap. SUSTIVA 200 mg hard capsules Dark yellow, printed with "SUSTIVA" on the body and "200 mg" on the cap. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications SUSTIVA is indicated in antiviral combination treatment of human immunodeficiency virus-1 (HIV- 1) infected adults, adolescents and children 3 months of age and older and weighing at least 3.5 kg. SUSTIVA has not been adequately studied in patients with advanced HIV disease, namely in patients with CD4 counts < 50 cells/mm3, or after failure of protease inhibitor (PI) containing regimens. -
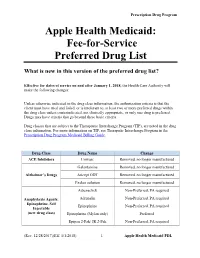
Fee-For-Service Preferred Drug List
Prescription Drug Program Apple Health Medicaid: Fee-for-Service Preferred Drug List What is new in this version of the preferred drug list? Effective for dates of service on and after January 1, 2018, the Health Care Authority will make the following changes: Unless otherwise indicated in the drug class information, the authorization criteria is that the client must have tried and failed, or is intolerant to, at least two or more preferred drugs within the drug class unless contraindicated, not clinically appropriate, or only one drug is preferred. Drugs may have criteria that go beyond these basic criteria. Drug classes that are subject to the Therapeutic Interchange Program (TIP), are noted in the drug class information. For more information on TIP, see Theraputic Interchange Program in the Prescription Drug Program Medicaid Billing Guide. Drug Class Drug Name Change ACE Inhibitors Univasc Removed, no longer manufactured Galantamine Removed, no longer manufactured Alzheimer’s Drugs Aricept ODT Removed, no longer manufactured Exelon solution Removed, no longer manufactured Adrenaclick Non-Preferred, PA required Anaphylaxis Agents: Adrenalin Non-Preferred, PA required Epinephrine, Self Epinephrine Non-Preferred, PA required Injectable (new drug class) Epinephrine (Mylan only) Preferred Epipen 2-Pak/ JR 2-Pak Non-Preferred, PA required (Rev. 12/28/2017)(Eff. 1/1/2018) – 1 – Apple Health Medicaid PDL Prescription Drug Program Renamed drug class “Anticoagulants: Anticoagulants Entire class Factor XA and Thrombin Inhibitors.” Anticoagulants: -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Efavirenz) Capsules and Tablets 3 Rx Only
1 SUSTIVA® 2 (efavirenz) capsules and tablets 3 Rx only 4 DESCRIPTION 5 SUSTIVA® (efavirenz) is a human immunodeficiency virus type 1 (HIV-1) specific, non- 6 nucleoside, reverse transcriptase inhibitor (NNRTI). 7 Capsules: SUSTIVA is available as capsules for oral administration containing either 8 50 mg, 100 mg, or 200 mg of efavirenz and the following inactive ingredients: lactose 9 monohydrate, magnesium stearate, sodium lauryl sulfate, and sodium starch glycolate. 10 The capsule shell contains the following inactive ingredients and dyes: gelatin, sodium 11 lauryl sulfate, titanium dioxide, and/or yellow iron oxide. The capsule shells may also 12 contain silicon dioxide. The capsules are printed with ink containing carmine 40 blue, 13 FD&C Blue No. 2, and titanium dioxide. 14 Tablets: SUSTIVA is available as film-coated tablets for oral administration containing 15 600 mg of efavirenz and the following inactive ingredients: croscarmellose sodium, 16 hydroxypropyl cellulose, lactose monohydrate, magnesium stearate, microcrystalline 17 cellulose, and sodium lauryl sulfate. The film coating contains Opadry® Yellow and 18 Opadry® Clear. The tablets are polished with carnauba wax and printed with purple ink, 19 Opacode® WB. 20 Efavirenz is chemically described as (S)-6-chloro-4-(cyclopropylethynyl)-1,4-dihydro-4- 21 (trifluoromethyl)-2H-3,1-benzoxazin-2-one. 22 Its empirical formula is C14H9ClF3NO2 and its structural formula is: 1 of 45 Approved v2.0 F C 3 Cl O NO 23 H 24 Efavirenz is a white to slightly pink crystalline powder with a molecular mass of 315.68. 25 It is practically insoluble in water (<10 µg/mL). -

SUSTIVA Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION • Embryo-Fetal Toxicity: Avoid administration in the first trimester of These highlights do not include all the information needed to use pregnancy as fetal harm may occur. (5.6, 8.1) SUSTIVA safely and effectively. See full prescribing information for • Hepatotoxicity: Monitor liver function tests before and during treatment in SUSTIVA. patients with underlying hepatic disease, including hepatitis B or C SUSTIVA (efavirenz) capsules for oral use coinfection, marked transaminase elevations, or who are taking medications associated with liver toxicity. Among reported cases of SUSTIVA (efavirenz) tablets for oral use hepatic failure, a few occurred in patients with no pre-existing hepatic Initial U.S. Approval: 1998 disease. (5.8, 6.1, 8.6) ---------------------------INDICATIONS AND USAGE--------------------------- • Rash: Rash usually begins within 1-2 weeks after initiating therapy and SUSTIVA is a non-nucleoside reverse transcriptase inhibitor indicated in resolves within 4 weeks. Discontinue if severe rash develops. (5.7, 6.1, 17) combination with other antiretroviral agents for the treatment of human • Convulsions: Use caution in patients with a history of seizures. (5.9) immunodeficiency virus type 1 infection in adults and in pediatric patients at • Lipids: Total cholesterol and triglyceride elevations. Monitor before least 3 months old and weighing at least 3.5 kg. (1) therapy and periodically thereafter. (5.10) • Immune reconstitution syndrome: May necessitate further evaluation and -----------------------DOSAGE AND ADMINISTRATION---------------------- treatment. (5.11) • SUSTIVA should be taken orally once daily on an empty stomach, • Redistribution/accumulation of body fat: Observed in patients receiving preferably at bedtime. (2) antiretroviral therapy. (5.12, 17) • Recommended adult dose: 600 mg. -

HIV Genotyping and Phenotyping AHS – M2093
Corporate Medical Policy HIV Genotyping and Phenotyping AHS – M2093 File Name: HIV_genotyping_and_phenotyping Origination: 1/2019 Last CAP Review: 2/2021 Next CAP Review: 2/2022 Last Review: 2/2021 Description of Procedure or Service Description Human immunodeficiency virus (HIV) is an RNA retrovirus that infects human immune cells (specifically CD4 cells) causing progressive deterioration of the immune system ultimately leading to acquired immune deficiency syndrome (AIDS) characterized by susceptibility to opportunistic infections and HIV-related cancers (CDC, 2014). Related Policies Plasma HIV-1 and HIV-2 RNA Quantification for HIV Infection Scientific Background Human immunodeficiency virus (HIV) targets the immune system, eventually hindering the body’s ability to fight infections and diseases. If not treated, an HIV infection may lead to acquired immunodeficiency syndrome (AIDS) which is a condition caused by the virus. There are two main types of HIV: HIV-1 and HIV-2; both are genetically different. HIV-1 is more common and widespread than HIV-2. HIV replicates rapidly; a replication cycle rate of approximately one to two days ensures that after a single year, the virus in an infected individual may be 200 to 300 generations removed from the initial infection-causing virus (Coffin & Swanstrom, 2013). This leads to great genetic diversity of each HIV infection in a single individual. As an RNA retrovirus, HIV requires the use of a reverse transcriptase for replication purposes. A reverse transcriptase is an enzyme which generates complimentary DNA from an RNA template. This enzyme is error-prone with the overall single-step point mutation rate reaching ∼3.4 × 10−5 mutations per base per replication cycle (Mansky & Temin, 1995), leading to approximately one genome in three containing a mutation after each round of replication (some of which confer drug resistance). -

Summary of Neuraminidase Amino Acid Substitutions Associated with Reduced Inhibition by Neuraminidase Inhibitors
Summary of neuraminidase amino acid substitutions associated with reduced inhibition by neuraminidase inhibitors. Susceptibility assessed by NA inhibition assays Source of Type/subtype Amino acid N2 b (IC50 fold change vs wild type [NAI susceptible virus]) viruses/ References Comments substitutiona numberinga Oseltamivir Zanamivir Peramivir Laninamivir selection withc A(H1N1)pdm09 I117R 117 NI (1) RI (10) ? ?d Sur (1) E119A 119 NI/RI (8-17) RI (58-90) NI/RI (7-12) RI (82) RG (2, 3) E119D 119 RI (25-23) HRI (583-827) HRI (104-286) HRI (702) Clin/Zan; RG (3, 4) E119G 119 NI (1-7) HRI (113-1306) RI/HRI (51-167) HRI (327) RG; Clin/Zan (3, 5, 6) E119V 119 RI (60) HRI (571) RI (25) ? RG (5) Q136K/Q 136 NI (1) RI (20) ? ? Sur (1) Q136K 136 NI (1) HRI (86-749) HRI (143) RI (42-45) Sur; RG; in vitro (2, 7, 8) Q136R was host Q136R 136 NI (1) HRI (200) HRI (234) RI (33) Sur (9) cell selected D151D/E 151 NI (3) RI (19) RI (14) NI (5) Sur (9) D151N/D 151 RI (22) RI (21) NI (3) NI (3) Sur (1) R152K 152 RI(18) NI(4) NI(4) ? RG (3, 6) D199E 198 RI (16) NI (7) ? ? Sur (10) D199G 198 RI (17) NI (6) NI (2) NI (2) Sur; in vitro; RG (2, 5) I223K 222 RI (12–39) NI (5–6) NI (1–4) NI (4) Sur; RG (10-12) Clin/No; I223R 222 RI (13–45) NI/RI (8–12) NI (5) NI (2) (10, 12-15) Clin/Ose/Zan; RG I223V 222 NI (6) NI (2) NI (2) NI (1) RG (2, 5) I223T 222 NI/RI(9-15) NI(3) NI(2) NI(2) Clin/Sur (2) S247N 246 NI (4–8) NI (2–5) NI (1) ? Sur (16) S247G 246 RI (15) NI (1) NI (1) NI (1) Clin/Sur (10) S247R 246 RI (36-37) RI (51-54) RI/HRI (94-115) RI/HRI (90-122) Clin/No (1)