Non-Anntoated Product Monograph
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Targeting Fibrosis in the Duchenne Muscular Dystrophy Mice Model: an Uphill Battle
bioRxiv preprint doi: https://doi.org/10.1101/2021.01.20.427485; this version posted January 21, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Title: Targeting fibrosis in the Duchenne Muscular Dystrophy mice model: an uphill battle 2 Marine Theret1#, Marcela Low1#, Lucas Rempel1, Fang Fang Li1, Lin Wei Tung1, Osvaldo 3 Contreras3,4, Chih-Kai Chang1, Andrew Wu1, Hesham Soliman1,2, Fabio M.V. Rossi1 4 1School of Biomedical Engineering and the Biomedical Research Centre, Department of Medical 5 Genetics, 2222 Health Sciences Mall, Vancouver, BC, V6T 1Z3, Canada 6 2Department of Pharmacology and Toxicology, Faculty of Pharmaceutical Sciences, Minia 7 University, Minia, Egypt 8 3Developmental and Stem Cell Biology Division, Victor Chang Cardiac Research Institute, 9 Darlinghurst, NSW, 2010, Australia 10 4Departamento de Biología Celular y Molecular and Center for Aging and Regeneration (CARE- 11 ChileUC), Facultad de Ciencias Biológicas, Pontificia Universidad Católica de Chile, 8331150 12 Santiago, Chile 13 # Denotes Co-first authorship 14 15 Keywords: drug screening, fibro/adipogenic progenitors, fibrosis, repair, skeletal muscle. 16 Correspondence to: 17 Marine Theret 18 School of Biomedical Engineering and the Biomedical Research Centre 19 University of British Columbia 20 2222 Health Sciences Mall, Vancouver, British Columbia 21 Tel: +1(604) 822 0441 fax: +1(604) 822 7815 22 Email: [email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.01.20.427485; this version posted January 21, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. -

Viiv Healthcare Drug Class1,4: Antiretroviral Agent, Integrase
Brand Name: Tivicay Generic Name: dolutegravir Manufacturer1: ViiV Healthcare Drug Class1,4: Antiretroviral Agent, Integrase Inhibitor Labeled Uses4,5: Labeled1,4: In combination with other antiretroviral agents for the treatment of human immunodeficiency virus type 1 (HIV-1) infection in adults and children aged 12 years and older and weighing at least 40 kg. Mechanism of Action1,2: Dolutegravir inhibits the catalytic activity of HIV integrase, which is an HIV encoded enzyme required for viral replication. Integrase is one of the three HIV-1 enzymes required for viral replication. Integration of HIV into cellular DNA is a multi-step process. First, the assembly of integrase in a stable complex with the viral DNA occurs. Second, the terminal dinucleotides from each end of the viral DNA are removed by endonucleolytic processing. Lastly, the viral DNA 3' ends are covalently linked to the cellular (target) DNA by strand transfer. The last two processes, which are catalytic, require integrase to be appropriately assembled on a specific viral DNA substrate. Inhibition of integrase by dolutegravir prevents the covalent insertion, or integration, of unintegrated linear HIV DNA into the host cell genome preventing the formation of the HIV provirus. The provirus is required to direct the production of progeny virus, so inhibiting integration prevents propagation of the viral infection. Pharmacokinetics1: Absorption: Tmax 2-3 hours Vd 17.4L T1/2 14 hours Clearance 1.0 L/h Protein Binding >98.9% Bioavailability Not established Metabolism1,2: Dolutegravir is primarily metabolized via UGT1A1 with some contribution from CYP3A. Metabolism occurs via UDP-glucuronosyltransferase (UGT)1A1 (major) and by the hepatic isoenzyme CYP3A (minor). -

United States Patent (19) 11 Patent Number: 5,993,812 Tsoukas Et Al
USOO5993812A United States Patent (19) 11 Patent Number: 5,993,812 TSOukas et al. (45) Date of Patent: Nov.30, 1999 54 METHOD OF DELAYING THE Brunkhorst et al., Infection 18:28-32, 1990. PROGRESSION OF AN INFECTION WITH Coyle et al., Changes in the Lymphocyte Count and Lym THE HUMAN IMMUNODEFICIENCY VIRUS phocyte Subsets After Splenectomy in Human Immunode ficiency Virus Infection, Letters and Correspondence, pp. 75 Inventors: Christos M. Tsoukas, Montreal; Barry 144-146. Michael Woloski, Winnipeg, both of DeSimone et al., Immunopharma. and Immunotoxic., Canada 13:447-458, 1991. Gringeri et al., British Journal of Haemotology, 80:337-340, 73 Assignee: Cangene Corporation, Winnipeg, 1992. Canada Gingör et al., Eur. J. Pediatr., 152:650–654, 1993. Mofenson and Moye, Pediatric Research, 33:80-S89, 1993. 21 Appl. No.: 08/835,400 Mofenson et al., Journal of Acquired Immune Deficiency 22 Filed: Apr. 7, 1997 Syndrome, 6:1103-1113, 1993. Schrappe-Bächer et al., Vox Sang, 59:3-14, 1990. Related U.S. Application Data Shearer et al., Ann. N.Y. Acad. Sci., pp. 35-51. Wagner et al., Arch. of Disease in Childhood., 63 Continuation-in-part of application No. 08/713,765, Sep. 13, 67:1267-1271, 1992. 1996, abandoned. Watson, et al., “Recombinant DNA”, Scientific American 60 Provisional application No. 60/003,756, Sep. 14, 1995. Books, Chapter 25. 51) Int. Cl. ............................ A61K 39/395; CO7K 1/00 Okesenhendeler, et al., “Anti-RH immunoglobulin therapy 52 U.S. Cl. ................... 424/130.1; 530/350, 530/388.7; for human immunodeficiency virus-related immune throm 424/142.1; 424/141.1; 424/153.1 bocytopenic purpura’, Blood, 71 (5) 1499-502. -

HIV Integrase Inhibitor Pharmacogenetics and Clinical Outcomes: an Exploratory Association Study Derek E
East Tennessee State University Digital Commons @ East Tennessee State University Electronic Theses and Dissertations Student Works 8-2018 HIV Integrase Inhibitor Pharmacogenetics and Clinical Outcomes: An Exploratory Association Study Derek E. Murrell East Tennessee State University Follow this and additional works at: https://dc.etsu.edu/etd Part of the Other Pharmacy and Pharmaceutical Sciences Commons, Pharmacology Commons, and the Virus Diseases Commons Recommended Citation Murrell, Derek E., "HIV Integrase Inhibitor Pharmacogenetics and Clinical Outcomes: An Exploratory Association Study" (2018). Electronic Theses and Dissertations. Paper 3465. https://dc.etsu.edu/etd/3465 This Dissertation - Open Access is brought to you for free and open access by the Student Works at Digital Commons @ East Tennessee State University. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of Digital Commons @ East Tennessee State University. For more information, please contact [email protected]. HIV Integrase Inhibitor Pharmacogenetics and Clinical Outcomes: An Exploratory Association Study _____________________ A dissertation presented to the faculty of the Department of Biomedical Sciences East Tennessee State University In partial fulfillment of the requirements for the degree Doctor of Philosophy in Biomedical Sciences, Pharmaceutical Sciences Concentration _____________________ by Derek Edward Murrell August 2018 _____________________ Sam Harirforoosh, PharmD, PhD, Chair Jonathan Moorman, MD, PhD David Roane, PhD Robert Schoborg, PhD Zhi Qiang Yao, MD, PhD Keywords: Integrase Strand Transfer Inhibitor, Dolutegravir, Elvitegravir, Raltegravir, Pharmacogenetics, HIV, Renal, Hepatic, Adverse events ABSTRACT HIV Integrase Inhibitor Pharmacogenetics and Clinical Outcomes: An Exploratory Association Study by Derek Edward Murrell As HIV is now primarily a chronic condition, treatment is given life-long with changes as necessitated by alterations in tolerability and efficacy. -

VIDEX (Didanosine) Chewable/Dispersible Buffered Tablets
Rx only VIDEXâ (didanosine) â VIDEX (didanosine) Chewable/Dispersible Buffered Tablets â VIDEX (didanosine) Buffered Powder for Oral Solution â VIDEX (didanosine) Pediatric Powder for Oral Solution (Patient Information Leaflet Included) WARNING FATAL AND NONFATAL PANCREATITIS HAVE OCCURRED DURING THERAPY WITH VIDEX USED ALONE OR IN COMBINATION REGIMENS IN BOTH TREATMENT-NAIVE AND TREATMENT-EXPERIENCED PATIENTS, REGARDLESS OF DEGREE OF IMMUNOSUPPRESSION. VIDEX SHOULD BE SUSPENDED IN PATIENTS WITH SUSPECTED PANCREATITIS AND DISCONTINUED IN PATIENTS WITH CONFIRMED PANCREATITIS (SEE WARNINGS). LACTIC ACIDOSIS AND SEVERE HEPATOMEGALY WITH STEATOSIS, INCLUDING FATAL CASES, HAVE BEEN REPORTED WITH THE USE OF NUCLEOSIDE ANALOGUES ALONE OR IN COMBINATION, INCLUDING DIDANOSINE AND OTHER ANTIRETROVIRALS. FATAL LACTIC ACIDOSIS HAS BEEN REPORTED IN PREGNANT WOMEN WHO RECEIVED THE COMBINATION OF DIDANOSINE AND STAVUDINE WITH OTHER ANTIRETROVIRAL AGENTS. THE COMBINATION OF DIDANOSINE AND STAVUDINE SHOULD BE USED WITH CAUTION DURING PREGNANCY AND IS RECOMMENDED ONLY IF THE POTENTIAL BENEFIT CLEARLY OUTWEIGHS THE POTENTIAL RISK. (SEE WARNINGS AND PRECAUTIONS: PREGNANCY.) Page 4 of 39 DESCRIPTION â VIDEX (didanosine) is a brand name for didanosine (ddI), a synthetic purine nucleoside analogue active against the Human Immunodeficiency Virus (HIV). VIDEX Chewable/Dispersible Buffered Tablets are available for oral administration in strengths of 25, 50, 100, 150, and 200 mg of didanosine. Each tablet is buffered with calcium carbonate and magnesium hydroxide. VIDEX tablets also contain aspartame, sorbitol, microcrystalline cellulose, polyplasdone, mandarin-orange flavor, and magnesium stearate. VIDEX Buffered Powder for Oral Solution is supplied for oral administration in single- dose packets containing 100, 167, or 250 mg of didanosine. Packets of each product strength also contain a citrate-phosphate buffer (composed of dibasic sodium phosphate, sodium citrate, and citric acid) and sucrose. -
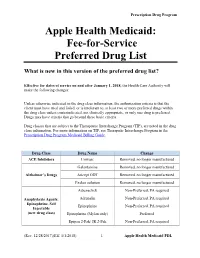
Fee-For-Service Preferred Drug List
Prescription Drug Program Apple Health Medicaid: Fee-for-Service Preferred Drug List What is new in this version of the preferred drug list? Effective for dates of service on and after January 1, 2018, the Health Care Authority will make the following changes: Unless otherwise indicated in the drug class information, the authorization criteria is that the client must have tried and failed, or is intolerant to, at least two or more preferred drugs within the drug class unless contraindicated, not clinically appropriate, or only one drug is preferred. Drugs may have criteria that go beyond these basic criteria. Drug classes that are subject to the Therapeutic Interchange Program (TIP), are noted in the drug class information. For more information on TIP, see Theraputic Interchange Program in the Prescription Drug Program Medicaid Billing Guide. Drug Class Drug Name Change ACE Inhibitors Univasc Removed, no longer manufactured Galantamine Removed, no longer manufactured Alzheimer’s Drugs Aricept ODT Removed, no longer manufactured Exelon solution Removed, no longer manufactured Adrenaclick Non-Preferred, PA required Anaphylaxis Agents: Adrenalin Non-Preferred, PA required Epinephrine, Self Epinephrine Non-Preferred, PA required Injectable (new drug class) Epinephrine (Mylan only) Preferred Epipen 2-Pak/ JR 2-Pak Non-Preferred, PA required (Rev. 12/28/2017)(Eff. 1/1/2018) – 1 – Apple Health Medicaid PDL Prescription Drug Program Renamed drug class “Anticoagulants: Anticoagulants Entire class Factor XA and Thrombin Inhibitors.” Anticoagulants: -

Guidelines for the Use of Antiretroviral Agents in Adults and Adolescent Living With
Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV Developed by the DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents – A Working Group of the Office of AIDS Research Advisory Council (OARAC) How to Cite the Adult and Adolescent Guidelines: Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Department of Health and Human Services. Available at https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/ AdultandAdolescentGL.pdf. Accessed [insert date] [insert page number, table number, etc. if applicable] It is emphasized that concepts relevant to HIV management evolve rapidly. The Panel has a mechanism to update recommendations on a regular basis, and the most recent information is available on the HIVinfo Web site (http://hivinfo.nih.gov). What’s New in the Guidelines? August 16, 2021 Hepatitis C Virus/HIV Coinfection • Table 18 of this section has been updated to include recommendations regarding concomitant use of fostemsavir or long acting cabotegravir plus rilpivirine with different hepatitis C treatment regimens. June 3, 2021 What to Start • Since the release of the last guidelines, updated data from the Botswana Tsepamo study have shown that the prevalence of neural tube defects (NTD) associated with dolutegravir (DTG) use during conception is much lower than previously reported. Based on these new data, the Panel now recommends that a DTG-based regimen can be prescribed for most people with HIV who are of childbearing potential. Before initiating a DTG-based regimen, clinicians should discuss the risks and benefits of using DTG with persons of childbearing potential, to allow them to make an informed decision. -

NORVIR and Certain Other Drugs May Result in These Highlights Do Not Include All the Information Needed to Use Known Or Potentially Significant Drug Interactions
HIGHLIGHTS OF PRESCRIBING INFORMATION • The concomitant use of NORVIR and certain other drugs may result in These highlights do not include all the information needed to use known or potentially significant drug interactions. Consult the full NORVIR safely and effectively. See full prescribing information for prescribing information prior to and during treatment for potential drug NORVIR. interactions. (5.1, 7.2) • Hepatotoxicity: Fatalities have occurred. Monitor liver function before and NORVIR (ritonavir) capsules, soft gelatin for oral use during therapy, especially in patients with underlying hepatic disease, Initial U.S. Approval: 1996 including hepatitis B and hepatitis C, or marked transaminase elevations. (5.2, 8.6) WARNING: DRUG-DRUG INTERACTIONS LEADING TO • Pancreatitis: Fatalities have occurred; suspend therapy as clinically POTENTIALLY SERIOUS AND/OR LIFE THREATENING appropriate. (5.3) REACTIONS • Allergic Reactions/Hypersensitivity: Allergic reactions have been reported See full prescribing information for complete boxed warning and include anaphylaxis, toxic epidermal necrolysis, Stevens-Johnson Co-administration of NORVIR with several classes of drugs including syndrome, bronchospasm and angioedema. Discontinue treatment if severe sedative hypnotics, antiarrhythmics, or ergot alkaloid preparations may reactions develop. (5.4, 6.2) result in potentially serious and/or life-threatening adverse events due to • PR interval prolongation may occur in some patients. Cases of second and possible effects of NORVIR on the hepatic metabolism of certain drugs. third degree heart block have been reported. Use with caution with patients Review medications taken by patients prior to prescribing NORVIR or with preexisting conduction system disease, ischemic heart disease, when prescribing other medications to patients already taking NORVIR cardiomyopathy, underlying structural heart disease or when administering (4, 5.1) with other drugs that may prolong the PR interval. -
Clinician's Reference Guide to Curanderismo
Clinician’s Reference Guide to Curanderismo Reference Guide Focus Scope of reference guide – to provide a basic introduc‐ tion to “curanderismo” to enhance the provider’s ability to confidently initiate conversations with patients who practice this form of traditional healing/complementary and alternative medicine (TCAM). This reference guide will 1) demystify common myths about curanderismo by clarifying what it is/is not, 2) review benefits of knowing about curanderismo to improve communication be‐ tween patient and provider; and 3) highlight some use‐ ful terminology for use with patients who practice forms of curanderismo. Goal – To improve health outcomes among Latino/as living with HIV disease, the health care provider and patient/client will collaborate on a more culturally ap‐ propriate treatment plan through a better understand‐ ing of the patient’s 1) core health beliefs and practices, 2) reasons Latino/a patients may use curanderismo and highlights of risks and 3) how the practices may inter‐ fere with conventional medical practices. Target audience – health care providers including: physi‐ cians, physician assistants, advanced practice nurses, nurses, pharmacists, oral health professionals as well as substance abuse counselors and mental health counsel‐ ors. TABLE OF CONTENTS: Introduction What Is and What Isn't Curanderismo Benefits to Knowing about Curanderismo Useful Terminology Commonly Used Herbs, Spices, & Other Items Why It Is Important to ask Introduction According to the World Health Organization, traditional medicine continues to be used in Latin America, Africa, and Asia to meet primary health care needs. In many developed countries, up to 80% of the population have used some form of traditional healing, complementary or alternative medi‐ cine ‐ TCAM (e.g. -

AIDS Related Treatments HIV Treatment and Prevention Website: Antiretrovirals
MICHIGAN DRUG ASSISTANCE PROGRAM 1 Last Updated: 7/1/15 All Previous Versions Obsolete HIV / AIDS Related Treatments HIV Treatment and Prevention Website: http://www.aidsinfo.nih.gov/ Antiretrovirals Nucleoside/Nucleotide Reverse Non-Nucleoside Reverse CCR-5 Inhibitor Selzentry (Maraviroc) - MIDAP will no longer utilize the previous form of medical Transcriptase Inhibitors Transcriptase Inhibitors necessity for authorizing tropism assay coverage Abacavir (ZIAGEN) Delavirdine (RESCRIPTOR) Process for obtaining tropism assay: Abacavir/lamivudine (EPZICOM) Efavirenz (SUSTIVA) - Any MIDAP patient that requires a tropism test Abacavir/lamivudine/zidovudine Nevirapine (VIRAMUNE, VIRAMUNE XR) * will need to complete the ViiV Healthcare Tropsim (TRIZIVIR) Etravirine (INTELENCE) Access Program certificate form. These may be obtained by your local ViiV representative. Didanosine (VIDEX EC*, VIDEX Rilpivirine (EDURANT) - Please note that the Trofile assay requires the HIV- soln) Protease Inhibitors & Combinations 1 RNA PCR to be >1000 copies/mL. Emtricitabine (EMTRIVA) Atazanavir (REYATAZ) - The Trofile DNA assay should only be used when Emtricitabine/Tenefovir (TRUVADA) Darunavir (PREZISTA) the HIV-1 RNA PCR is less than the lower limit of Lamivudine (EPIVIR)* Fosamprenavir (LEXIVA) detection (ie. undetectable). Lamivudine/zidovudine Process for obtaining Selzentry (maraviroc) Indinavir (CRIXIVAN) (COMBIVIR)* coverage: Lopinavir/ritonavir (KALETRA) Stavudine (ZERIT)* - MIDAP will approve the use of Selzentry for Nelfinavir (VIRACEPT)* Tenofovir (VIREAD) members who have tropism results of R5 virus Ritonavir (NORVIR) ONLY. Dual / mixed virus will not be approved. Zidovudine (RETROVIR)* Saquinavir (INVIRASE) - To obtain coverage of this drug, please fax the lab HIV Integrase Inhibitor Tipranavir (APTIVUS) result to the MIDAP Office at 1-517-335-7723 Raltegravir (ISENTRESS) Darunavir/Cobicistat (PREZCOBIX) - Please allow 2 days for processing. -
![1-Acetyl-17-{2-Hydroxy-3-[4-(2-Methoxyphenyl)Piperazin-1- Yl]Propyl}-17-Azapentacyclo[6.6.5.0 2,7 .0 9,14 .0 15,19 ]Nonadeca- 2,4,6,9,11,13-Hexaene-16,18-Dione](https://docslib.b-cdn.net/cover/2983/1-acetyl-17-2-hydroxy-3-4-2-methoxyphenyl-piperazin-1-yl-propyl-17-azapentacyclo-6-6-5-0-2-7-0-9-14-0-15-19-nonadeca-2-4-6-9-11-13-hexaene-16-18-dione-1512983.webp)
1-Acetyl-17-{2-Hydroxy-3-[4-(2-Methoxyphenyl)Piperazin-1- Yl]Propyl}-17-Azapentacyclo[6.6.5.0 2,7 .0 9,14 .0 15,19 ]Nonadeca- 2,4,6,9,11,13-Hexaene-16,18-Dione
Molbank 2010 , M697; doi:10.3390/M697 OPEN ACCESS molbank ISSN 1422-8599 www.mdpi.com/journal/molbank Short Note 1-Acetyl-17-{2-hydroxy-3-[4-(2-methoxyphenyl)piperazin-1- yl]propyl}-17-azapentacyclo[6.6.5.0 2,7 .0 9,14 .0 15,19 ]nonadeca- 2,4,6,9,11,13-hexaene-16,18-dione Magdalena Pakosi ńska-Parys *, Jerzy Kossakowski and Marta Struga Chair and Department of Medical Chemistry, 1 st Faculty of Medicine, Medical University of Warsaw, 3 Oczki Street, 02-007 Warsaw, Poland * Author to whom correspondence should be addressed; E-Mail: [email protected] Received: 5 August 2010 / Accepted: 14 September 2010 / Published: 17 September 2010 Abstract: The title compound was synthesized by condensation of an oxiran imide derivative with an appropriate amine and its IR, 1H NMR, 13 C NMR and mass spectroscopic data are reported. The synthesized compound was evaluated for its cytotoxicity and anti-HIV-1 activity in MT-4 cells. Keywords: 1-acetyl-17-{2-hydroxy-3-[4-(2-methoxyphenyl)piperazin-1-yl]propyl}-17- azapentacyclo[6.6.5.0 2,7 .0 9,14 .0 15,19 ]nonadeca-2,4,6,9,11,13-hexaene-16,18-dione; cytotoxicity Introduction Currently available drugs for the treatment of HIV infections are based on combination of two types of anti-HIV-1 agents: nucleoside reverse transcriptase inhibitors (RTIs) and protease inhibitors [1]. The RTIs can be divided into nucleoside (NI) and non-nucleoside RT inhibitors (NNRTI). Several non-nucleoside inhibitors have been described, including nevirapine, thiobenzimidazolone (TIBO) derivatives, pyridinone derivatives and the bis(heteroaryl)piperazines (BHAPs), such as delavirdine and atevirdine [2]. -

Management of Antiretroviral Therapy
International AIDS Society–USA Topics in HIV Medicine Management of Antiretroviral Therapy Timothy J. Wilkin, MD, C. Mhorag Hay, MD, Christine M. Hogan, MD, and Scott M. Hammer, MD As in previous years, the 9th Conference Entry Inhibitors ants (Abstract 2). The drug is not cur- on Retroviruses and Opportunistic rently going forward in clinical develop- Infections provided a forum for a state- The chemokine receptors CCR5 and ment, but proof of principle appears to of-the-art update in antiretroviral thera- CXCR4 are coreceptors used by many have been established. py. Highlights included the status of strains of HIV-1 in addition to CD4 to new antiretroviral agents from both enter cells. Attempts are under way to CCR5 Receptor Blockers. Laughlin pre- existing and new drug classes; presenta- develop antiretroviral agents that inhib- sented the results for the first 12 HIV- tion of trials in antiretroviral-naive and it HIV-1 entry by blocking these requisite infected volunteers treated with SCH-C, antiretroviral-experienced persons; up- coreceptors. an orally bioavailable CCR5 receptor dates on strategic approaches to thera- antagonist with potent in vitro antiviral py, including when to start therapy, CXCR4 Receptor Blockers. AMD-3100 is a activity against a broad range of primary treatment interruptions, and immune- small-molecule CXCR4 receptor blocker HIV-1 isolates (Abstract 1). In this ongo- based therapies; mechanisms and evo- with potent in vitro anti-HIV activity. ing, sequential rising-dose trial, in which lution of viral drug resistance; clinical Results of an open-label dose-escala- there will be 12 subjects per group, HIV- applications of drug resistance testing; tion study to test the safety, pharma- infected volunteers receive 10 days of and therapeutic drug-level monitoring.